Abstract
Different mutations occurring in the unstable CGG repeat in 5' untranslated region of FMR1 gene are responsible for three fragile X-associated disorders. An expansion of over ∼200 CGG repeats when associated with abnormal methylation and inactivation of the promoter is the mutation termed ‘full mutation’ and is responsible for fragile X syndrome (FXS), a neurodevelopmental disorder described as the most common cause of inherited intellectual impairment. The term ‘abnormal methylation’ is used here to distinguish the DNA methylation induced by the expanded repeat from the ‘normal methylation’ occurring on the inactive X chromosomes in females with normal, premutation, and full mutation alleles. All male and roughly half of the female full mutation carriers have FXS. Another anomaly termed ‘premutation’ is characterized by the presence of 55 to ∼200 CGGs without abnormal methylation, and is the cause of two other diseases with incomplete penetrance. One is fragile X-associated primary ovarian insufficiency (FXPOI), which is characterized by a large spectrum of ovarian dysfunction phenotypes and possible early menopause as the end stage. The other is fragile X-associated tremor/ataxia syndrome (FXTAS), which is a late onset neurodegenerative disorder affecting males and females. Because of the particular pattern and transmission of the CGG repeat, appropriate molecular testing and reporting is very important for the optimal genetic counselling in the three fragile X-associated disorders. Here, we describe best practice guidelines for genetic analysis and reporting in FXS, FXPOI, and FXTAS, including carrier and prenatal testing.
Similar content being viewed by others
Fragile X syndrome, Fragile X-associated primary ovarian insufficiency, and Fragile X-associated tremor/ataxia syndrome
Fragile X syndrome (FXS, OMIM 300624), fragile X-associated primary ovarian insufficiency (FXPOI), and fragile X-associated tremor/ataxia syndrome (FXTAS, OMIM 300623) are three fragile X-associated disorders (FXDs), all caused by changes in FMR1 (fragile X mental retardation 1) gene.
Fragile X syndrome
The FXS is the most common cause of inherited intellectual disability with an estimated incidence of 1 in 4000 males1 and 1 in 5000–8000 females. Affected males present with mild to severe mental retardation with delay in language acquisition and/or behavioural problems being often the presenting symptoms. In addition to cognitive deficits, the FXS phenotype includes mild dysmorphic features (large everted ears and coarse elongated face) and macroorchidism established around puberty. Behavioural disturbances including attention-deficit, hyperactivity, or autistic-like behaviour can often be observed and around 30% of boys with FXS meet criteria for autism. Approximately 50% of female carriers of the disease causing mutation will have mild to moderate mental disabilities.
Because clinical symptoms are neither specific, nor constant, testing for fragile X mutation is usually part of the basic genetic assessment in the case of males or females who present with developmental delay, mental disabilities, and/or behavioural problems.
Carrier detection and prenatal diagnosis are other reasons for referral.
Fragile X-associated primary ovarian insufficiency
Another indication for testing is the occurrence of premature ovarian insufficiency (POI) in a female, especially in cases of familial POI. On the basis of a review of several studies,2 21% of female premutation carriers will have POI leading to an onset of menopause before 40 years of age (ie, premature ovarian failure, POF), which is significantly higher when compared with only 1% in the general population. As a group, females carrying a premutation present with a mean age at menopause ~5 years earlier than for females in the general population.3 Around 14% of families with familial POF and 2.3% of women with sporadic POF have a premutation.4, 5, 6 An elevated follicle-stimulating hormone level and an erratic menstrual function, without an otherwise known cause, are also reasons for referral before 40 years of age since they are the forerunners of a primary ovarian insufficiency leading to a POF.7
Fragile X-associated tremor/ataxia syndrome
A possible indication is a late onset neurodegenerative disorder found among some male and female carriers of the premutation.8, 9, 10, 11, 12, 13 This disorder is termed FXTAS and is characterized by intention tremor and cerebellar ataxia, as well as cognitive decline or impairment, peripheral neuropathy, Parkinsonism, and urinary and bowel incontinence. FXTAS is not only defined by clinical and molecular criteria but also by neuroradiological and neuropathological criteria. MRI findings show increased signals in the middle cerebellar peduncle and the deep white matter of the cerebellum. Testing for FMR1 premutation status should be performed for individuals over 50 years old who have symptoms consistent with FXTAS.11
Molecular genetic defects in FXS, FXPOI, and FXTAS, and transmission
The gene FMR1, located in Xq27.3, has 17 exons spanning 39 kb of genomic DNA. It encodes an RNA-binding protein termed FMRP.14, 15, 16 Different pathogenic mechanisms are thought to underlie the three fragile X-associated disorders.17
FMR1 has a polymorphic CGG repeat in its 5'-untranslated region (UTR),14,15,18 in which mutations are responsible for most of the FXS cases and for all FXPOI and FXTAS cases (Supplementary Figure 1). The CGG repeat may be ‘pure’ or interspersed with 1–4 AGGs in its 5' region. There is a threshold for major instability, leading to an increase/expansion in the CGG repeat number. This instability is thought to depend on the number of consecutive uninterrupted CGG repeats.19, 20, 21
The disease-causing mutations are (Table 1; Supplementary Table 1):
-
The premutation is an allele containing 55 to ∼200 CGG repeats, without abnormal methylation of the neighbouring CpG island and promoter, responsible for FXPOI in females and FXTAS in males and females. It has been shown that the premutation leads to overexpression and toxicity as well as a non-AUG translation of the FMR1 mRNA in FXTAS.22, 23, 24 The probability of developing FXPOI increases with increasing repeat size up to 100 CGGs, but thereafter the risk becomes stable or even decreases,3,25, 26, 27 whereas in FXTAS the penetrance is related to increasing age and size.28, 29, 30 Other phenotypes have been described in male premutation carriers, including autism spectrum disorder and attention-deficit hyperactivity disorder symptoms, as well as developmental delay. However, these data need to be confirmed by larger studies before they are used in diagnostic setting.
-
The full mutation is characterized by an allele size of over ∼200 CGG repeats, and associated abnormal methylation of the repeat, the neighbouring CpG island, and the gene promoter, thereby leading to a deficiency of FMR1 mRNA and thus FMRP, responsible for 99% of the reported FXS cases.31 All males and ~50% of females with full mutations are affected with FXS, females generally less severely than males.32
In adult tissues, the full mutation is mitotically stable when methylated.33,34 But in the early embryo, before methylation, fully expanded repeats experience mitotic instability frequently leading to size mosaicism.35
Mosaicism associating full mutation and premutation alleles (MoMP) is also not uncommon.
As established by different studies performed on male patients, other mosaic combinations can be observed: MoMN36,37 (Mosaicism for full Mutation and Normal alleles) or MoMPN genotype (Mosaicism for full Mutation, Premutation, and Normal alleles). In these cases, the normal sized alleles are usually in a lower percentage when compared with the other(s). Two laboratories calculated the frequency of the MoMN and the MoMPN as being 1% of all FXS males. In retrospective studies of 300 male carriers of a full mutation detected by Southern blot, a faint signal within or near the normal range was detectable in 30 of these patients, and PCR analysis detected a signal in the normal range for 3 out of these 30 patients, that is, 1% in 300 total (V Biancalana’s data). In a prospective study of over 15 years using both Southern blot and PCR analyses, 3 cases of MoMN have been detected on a cohort encompassing 220 male carriers of a full mutation (D Glaeser’s data).
Some individuals carry in their lymphocytes alleles >200 repeats that are completely or partially unmethylated (methylation mosaic: MoMe). Some of them have been reported to show a moderate or normal phenotype (‘high-functioning’ fragile X males).38,39
-
Other rare loss-of-function variations, such as substitutions40,41 or deletions of all or part of FMR1 have also been reported to cause the FXS, including a hot spot for deletions that occurred in the context of an expanded allele in FMR1 exon 1.42, 43, 44, 45, 46, 47, 48, 49, 50 There are gene variant public databases for the disease, in which it is important to share gene variants: the Human Gene Mutation Database (HGMD) and the locus-specific database (LOVD).
Instability of the CGG repeats and pattern of inheritance
Mutations affecting the polymorphic CGG repeat are dynamic in that they change the stability of the repeat in both somatic and germ cells, upon their mitotic proliferation, thereby favouring expansion of the repeat over generations. Contractions into another allele’s class are very rare,51, 52, 53, 54, 55 it is recommended to control by sequence analysis that the CGG repeat flanking sequences are not deleted in the case where the possible pathological impact needs to be evaluated.
Premutations are unstable and, when transmitted by a female, have a risk of expanding to a full mutation. This risk of transition is strongly dependent on the size of the maternal premutation, and is above 98% for alleles with >100 repeats.56, 57, 58, 59 The smallest described allele that underwent transition to a full mutation in a single generation is 56 CGG repeats without any AGG interruption.60 In the lower range of premutation, AGG structure and length of the 3' uninterrupted CGG array may be considered to better estimate the risk. Full mutations when transmitted by a female usually remain in the full mutation range. Prenatal diagnosis should be offered to women with 55 repeats and above.
Prenatal testing is not indicated for the pregnant partner of a male with a premutation since only transmission of premutations have been reported in all the numerous daughters of such fathers, with some exceptional cases of contraction to an allele in intermediate or normal range, but in no case has there been an expansion to a full mutation. Although a male with a full mutation is expected to transmit premutated FMR1 alleles to all his daughters based on the study of the sperm of four male carriers of a full mutation,61 it has only been confirmed at the molecular level in very few daughters.62, 63, 64, 65 There is, however, some controversy on the level of methylation of the large expansion found in the lymphocytes of the daughter of a male with a mosaic premutation and full mutation (MoMP).66,67 This controversy is due to the fact that the CGG repeat, regardless of its size, is always methylated on the inactive X chromosome. Prenatal testing may be considered for a female fetus of a full mutation father as a cautionary measure (full mutation or MoMP or MoMe).
The full mutations arise from premutations only and the premutations likely arise from large normal alleles. In the context of genetic counselling it is required to determine the significance of an allele under 55 CGGs, related to the risk of expansion in the next generation.
It has been proposed in previous EMQN guidelines (2006) to distinguish alleles likely to be stable with no need of genetic counselling (normal allele in the range of 6–49 CGGs) from alleles at the boundaries of normal alleles and premutation alleles with recommendation for genetic counselling (intermediate or grey-zone allele in the range of 50–54 CGGs). In this update, taking into account new data from the literature, we propose to use the same allele range definition for normal allele as the one used in several other guidelines68, 69, 70, 71 and based on the instability of the allele, that is, normal allele up to 44 CGGs and intermediate alleles from 45 to 54 CGGs.
It is known that alleles under 55 CGGs can show some instability upon transmission:
A study on 430 maternal transmissions in the general population has shown that <1% unstable transmissions for alleles <45 CGGs.72
There is an increasing likelihood for unstable transmissions with increasing repeat size.
Alleles in the 45–54 CGG range may show some instability, including expansion to a full mutation in two generations, although they have not been observed to expand to full mutations in only one generation:
-
An allele with 52 CGGs interspersed with two AGGs has been reported to expand to a full mutation in two generations through a 56 uninterrupted CGG repeat in one family.60 In a second family, a grandmother of two boys presenting with a full mutation was a carrier of a 45 uninterrupted CGG repeat allele whereas her two daughters were carriers of 80 and 90 CGG repeats, respectively.73 In a third family, another allele containing 44 CGGs is thought to have expanded to a full mutation in two generations through a 61 CGG repeat, although in this case, the possibility of mosaicism associated with this 44 CGG allele was not ruled out.74
-
On a study performed on 1112 maternal transmissions,59 9% of 55 alleles in the 45–49 CGG range were transmitted with instability but remained in the 45–49 range, whereas 26% of 51 alleles in the 50–54 CGG range were transmitted with instability, with 5 expanding into the premutation range. Further studies have shown that lower risk estimates for full mutation expansion may be appropriate for women identified as premutation carrier through routine screening, compared with women related to a premutation or full mutation carrier.75 The number of AGG interruptions and the length of uninterrupted CGG repeats at the 3' end are correlated with repeat instability on transmission, and their characterization may allow more accurate risk estimates of repeat instability and expansion to full mutations for intermediate and small premutation alleles.21,76
As a conclusion, alleles in the 45–54 range have not been shown to confer a risk of FXS in the very next generation but, particularly in the 50–54 range, they may show significant instability, meaning that untested asymptomatic family relatives may carry premutated alleles. It is thus recommended to always propose genetic counselling to relatives in case of alleles above or equal to 50 CGGs. In the range 45–49 the risk for instability is much lower and genetic counselling to relatives is linked to this risk. There are two additional types of data which may contribute to determine the stability of the allele. The first one is testing for AGG interspersion, but the usefulness of this data is not known for individual prediction at this time. The second point is the occurrence of larger alleles in relatives that would alert for a potential instability in case the allele in the 45–49 range share a common haplotype. Alleles in the 45–49 range can be more precisely evaluated by familial analysis when detected in a healthy relative of an individual affected by (or suspected) of a fragile X disorder who (may) carry an allele in the premutation or a full mutation range. In the context of screening in the general population in a healthy individual with no known family suspicion of FXD or in an affected individual, familial study may or may not be recommended, depending on local policy in different countries.
The term ‘fragile X syndrome’ has been used to refer to the developmental disorder caused by CGG expansions and other FMR1 mutations. However, in a small number of families, another fragile site has been linked to expansions at the nearby FRAXE locus of the AFF2 (FMR2) gene. AFF2 contains an unstable (CCG)n repeat whose expansions are responsible for a milder phenotype of non-syndromic mental impairment.77, 78, 79
Molecular diagnostic analysis in FXS, FXPOI, and FXTAS
The identification of the whole range of expansion requires an approach, which is able to accurately determine the number of repeats as well as the methylation status associated with the expanded allele.
There are different diagnostic procedures based on different combinations of techniques.
Both the clinical sensitivity and specificity are >99% when using appropriate (combinations of) techniques (Eurogen test clinical utility gene cards: http://www.eurogentest.org).80 It is best practice to use a method which detects the whole range of expansions when testing relatives (including prenatal diagnosis) in a family with any known fragile X disorder due to expansion. When testing the FMR1 gene in population screening, the report must specify that rare cases of point mutation or deletion cannot be detected, nor rare cases of CGG expansion mosaicism (MoMN) if the method used cannot detect the whole range of expansions.
It could be useful to confirm results by an independent method when detecting an expansion in an index case depending on specific pitfalls of each method.
Attention is drawn in these guidelines to the potential for misinterpretation due to the specific pitfalls of each method (Southern blot and PCR-based methods), and to the technical limitations of each protocol.
Although some tests can highlight an anomaly of the number of X chromosomes, it is not the purpose of FMR1 testing. Patients may be tested by conventional karyotype or another method to rule out sex chromosome abnormalities.
Southern blot analysis
Southern blot allows the identification of all expansions as well as the determination of the methylation status, when combined with a methylation-sensitive endonuclease. Accurate sizing of premutations requires the use of PCR. This is crucial to assess the risk of carrier females having children with FXS, and to distinguish between large normal, intermediate, and premutated alleles.
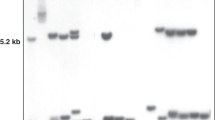
Southern blot analysis using a single enzyme (EcoRI with StB12.3, Ox1.9, pP2, or Pfxa7 which are equivalent probes) allows the detection of full mutations and large premutations, and is sufficient for testing of probands with learning difficulties (Supplementary Figure 1). However, it is often combined with methylation analysis using a methylation-sensitive enzyme that offers a very good strategy in family studies to detect premutations, full mutations, and mosaic patterns.81The need for radioactive handling can be avoided since a non-radioactive approach using a chemiluminescent probe is currently used in most of the laboratories.82
When high quality Southern blots with appropriate controls are analysed, interpretation is straightforward. However, some situations can lead to misinterpretations:
-
A full mutation can show up as a diffuse smear rather than as a single enlarged band due to heterogeneous array of FMR1 alleles: such smear of expanded fragments can be very faint and easily overlooked in case of high background and/or weak signal. In females, a normal signal is always present. It can be useful to compare the intensity of this signal with the expected intensity in order to be as sure as possible that an additional weak signal is not missed. If an expansion is suspected but the smear is too blurred to be sure about, then cleaving with BglII (which gives a normal fragment size of ~12 kb) will compress the smear enough to make it easily detectable. A female with a faint smear may be used as a control. As the amount of DNA can vary, the intensity of bands has to be compared to know whether the normal bands are strong enough to exclude a faint smear. Ethidium bromide must be absent during electrophoresis to avoid artificial smears.83
-
When the methylation status is to be determined, EcoRI is combined with a methylation-sensitive enzyme such as EagI or NruI, which gives a fragment of ~2.8 kb from the normal, unmethylated FMR1 gene. Methylated normal alleles are not cut by methylation-sensitive enzymes, and give rise to the normal 5.2-kb EcoRI fragment. Methylated and unmethylated expansions are indicated by the presence of bands and/or smears above 5.2 and 2.8 kb respectively. In premutation or full mutation females, non-random X-inactivation (seen by deviations from a 50:50 ratio between the methylated and unmethylated normal fragments) is an indication that an expansion or, rarely, a deletion of the FMR1 gene on one X chromosome may be present. But skewed inactivation is not always associated with an expansion.
-
In the methylation-sensitive digest, premutations are detected as fragments of 2.9 to about 3.3 kb in males and on the active X chromosome in females, whereas 5.3–5.7 kb fragments correspond to the premutation on the inactive X chromosome. Note that the FMR1 promoter is fully methylated on normal inactive X chromosomes in females. X-inactivation methylation of premutations should not be misinterpreted as an indication of the presence of a methylated full mutation.
-
It should be noted that in some female carriers of a premutation, skewed X inactivation can result in an atypical banding pattern (2.8 kb+expansion and 5.2 kb or 2.8 kb and 5.2 kb+expansion). Great care should be taken to ensure that the 2.8- and 5.2-kb bands are clearly aligned with the corresponding bands of the neighbouring tracks to exclude this possibility. It is good practice to place all female samples together to maximize the likelihood of detecting small migration changes. A control probe revealing a band of <2.8 kb allows a check on the homogeneity of migration throughout the gel and is useful in cases of a small premutation and/or a premutation with skewed inactivation, and for the detection of migration artefacts (caused for example by inappropriate DNA extraction protocol, samples extracted from blood collected in Lithium Heparin tubes, or sample overloading). Such a probe, StA22 associated with StB12.3, is freely available.84
-
A partial digestion may well be mistaken for a mutated (expanded) fragment.85 A useful marker to control for this is the co-migration of a size marker or, alternatively, comparison of the patterns in question with the results from an actual partial digest (fragments resulting from an incomplete EcoRI digest have around 6.5, 9, and 10 kb, and a 4.1-kb fragment appears also in EagI-EcoRI incomplete digestion when using StB12.3 or equivalent probe).
-
There are single-nucleotide polymorphisms (SNPs) creating or destroying restriction enzyme sites and thereby potentially mimicking an expansion or a deletion of the FMR1.86, 87, 88, 89, 90 Such a case can be highlighted by analysis with other methods especially by sequencing the potential SNP’s site.
PCR analysis
Compared with Southern blot, the PCR test is more rapid and easy to use but its approach encounters particular technical difficulties since the amplification of large CG-rich fragments is a laborious task. The study of the methylation pattern associated with an expansion is also a challenge.
Since the first PCR test described by Fu et al,15 several methods have been published that detect alleles in the normal range and up to the full mutation range: for example, conventional PCR across the CGG repeat using flanking primers, PCR test combined with Southern blot followed by probe detection,91 methyl sensitive PCR (MS-PCR),92 triplet-repeat primed PCR (TP-PCR) or triplet-repeat primed-methyl sensitive PCR (TP-MS-PCR).93, 94, 95, 96, 97 Commercial kits using such methods (Abbott (Chicago, IL, USA), Asuragen (Austin, TX, USA), Perkin Elmer (Waltham, MA, USA), etc) as well as a methylation sensitive-MLPA method (MRC-Holland, in male samples) are available. As a consequence, many laboratories use as a first test the conventional PCR with a threshold of detection in the premutation range, and only proceed to another method, which is able to detect the whole range of expansion, in case of need, that is, with samples that fail to amplify (males) or show a single normal sized PCR product (homozygous normal females, representing around 18% of females).
Some situations can lead to misinterpretations when using PCR approaches, some being general pitfalls and others being specific to the PCR techniques:
-
The gender of the individual and the possible occurrence of an abnormal karyotype (eg, XXX, XXY, and XXYY) should be kept in mind when interpreting a PCR result on X chromosomes.
-
PCR primers, including those from commercial kits, should be checked regularly that they do not bind to a sequence where a new SNP has been found, such an SNP could lead to false-negative results when associated with an expansion.
-
An internal control is important to distinguish a non-amplifiable allele with a probable expansion from an unsuccessful PCR. PCR for FMR1 can usefully be duplexed with PCR for AFF2,78 which provides an internal control with a similar GG content, but this strategy should be discussed with local clinicians before use to ensure they are aware that the test will also detect AFF2 expansions.
-
One possible concern about using PCR for fragile X diagnostics is that affected males who are mosaic for normal and full mutations might be missed (MoMN individuals), as the PCR would only amplify the normal allele.
-
A 49-bp tandem duplication adjacent to the triplet repeat in FMR1 has been described in the Finish population98 that affects annealing of the primers commonly used in the molecular analysis of the CGG repeat by PCR. One concern is that a female with an expansion and a variant allele may be genotyped as normal as a result of the two PCR products generated by the variant.
-
A false ‘expansion’ positive case has been reported and shown to be caused by a 5-bp deletion preventing primer annealing and leading to an apparent null allele while the CGG repeat was in the normal range.99
-
A false-negative result arising from repeat-flanking deletions has been reported using a 3' TP-PCR assay in DMPK gene study100,101 and it has been suggested to use an approach that combines 5' and 3' TP-PCR to minimize the incidence of such false-negative result.102
-
By measurement of the CGG repeat size, it may be difficult to distinguish a large premutation from a small full mutation (in the range of 200 repeats ±30). In such cases, determination of the methylation status is of great importance: premutations are not methylated on active X chromosomes whereas full mutations usually are.
-
The interpretation of an MS-PCR strategy that combines repeat length and methylation analysis of the FMR1 promoter or CGG repeat may be tricky in a female with a full mutation due to the presence of the methylated inactive normal X chromosome.
Indirect diagnosis
Indirect diagnosis with microsatellite markers is useful in very rare cases where confirmation of results is required by familial segregation analysis. A list of useful markers is set out in Supplementary Table 2. Although very rare, gene conversion, recombination events, and reduction in full mutation to premutated or even normal alleles have been described, and have to be considered in an indirect diagnosis.51, 52, 53, 54, 55,81,103, 104, 105 The possibility of microsatellite instability or of a ‘null’ or ‘cryptic’ allele (as described for DXS54853) should also be taken into consideration.
FMRP immunohistochemistry
Tests for the presence or absence of the FMR1 protein (FMRP) have been developed using immunohistochemistry.106 Validated postnatal applications include blood smears for males and hair roots for both sexes. The test has been reported in the study of some fetuses but it has not been fully validated due to limited availability of material. Logistic considerations are the major reasons for not making widely use of the FMRP test in diagnostic laboratories. Thus, the FMRP test is mainly used for the assessment of difficult cases (ie, patients with suggestive clinical phenotype but no expansion). An FMRP assay has been developed for dried blood spots as an alternative technique for newborn or population screening in male.107
Prenatal diagnosis in FXS
Prenatal diagnosis using chorionic villi and/or culture, amniotic fluid cells, and/or culture or blood samples are possible depending on physician performing the procedure and patient preference considering that (1) The use of a methylation-sensitive method is not suitable for early prenatal diagnosis because the methylation of a full mutation is not always present in DNA from chorionic villi,108 whereas it is established after the 14th week of pregnancy (true fetal age, it refers to the length of pregnancy from the time of conception). Also, in contrast to lymphocytes and amniocytes, the FMR1 gene is not methylated on the inactive X chromosome in the chorionic villi of female fetuses, (2) In most cases, the sizing of the expansion is sufficient to determine the genotype and the study on chorionic villi allows to reassure or to realize a possible therapeutic abortion at an early stage in the pregnancy, (3) The risk of miscarriage may be lower on amniotic fluid cells sampling, and (4) A test on amniotic fluid cells may be offered for confirmation in cases where a premutation has been found in chorionic villi DNA to detect or exclude a possible somatic mosaicism with a full mutation, in particular in case of great instability upon maternal transmission and/or large premutation allele, but no discrepancy has been reported in case the two tissues were analysed. An unique prenatal diagnosis on amniotic fluid cells could thus be favoured in case the risk of passing a full mutation is low (eg, when the mother is a carrier of a small premutation or the father is a carrier of a full mutation or a mosaic MoMP or MoMe), (5) If a signal in the large premutation/small full mutation range is detected on a DNA sample from chorionic villi, then determination of the methylation status is critical for distinction between the two classes of mutations, and in these rare cases a methylation-sensitive approach should be done on a DNA sample from amniotic fluid cells (at a time when full mutation methylation is to be expected) to give a definitive result.
In prenatal testing, analysis of DNA from the mother is also required to exclude maternal cell contamination in the fetal sample which can lead to a false diagnosis, especially with the CGG PCR techniques. The point being that the technique used to exclude maternal cell contamination must be as sensitive as the CCG PCR test. Maternal contamination can be checked with a panel of highly informative microsatellites markers in either the X chromosome or the autosomes (several very sensitive commercial kits are available).
The determination of the gender of the fetus using karyotyping or another method should be routinely carried out in parallel with fragile X testing on the prenatal sample.
Technical protocols
Quality assurance framework
The techniques used should be validated in-house with appropriate sample types and numbers. If CE-marked IVD kits are used, then in-house verification should be performed.
It is essential to include size markers in all types of fragile X analysis. The most useful markers are those which sizes lie at the borders of the different allele ranges. Using PCR, the conversion of base pairs, measured from the marker bands, into repeat units might not be linear, due to the high contents of C and G of the fragments which may lead to mobility shift due to structure formation of the amplicons. The CGG repeat size should be determined by means of an allelic ladder (genotyped by sequence analysis or by using validated controls, such as those available from Coriell, ATCC, etc). A WHO Certified Reference panel of five genomic DNA is available from NIBSC (UK).109
Laboratories reporting fragile X testing results should participate annually at least in external quality assessment. It is recommended that testing laboratories are accredited to international standards, for example, ISO 15189 or equivalent.
Interpretation and reporting
The reasons for referral should be restated with a clear distinction between diagnostic testing (FXS, FXTAS, or FXPOI), carrier testing (FXS), and prenatal diagnosis (FXS). The title of the report should reflect the reason for referral.
The report should indicate the gene (FMR1 and Accession number) and give data about the relevant allele’s range classes with reference source.
Nomenclature: HGVS’ nomenclature can be used but this must be in addition to an essential worded explanation describing the number of CGGs (eg, premutation, full mutation, etc) taking into account that fragile-X tri-nucleotide repeat is known as the CGG repeat, but based on the HGVS’ rule that for all descriptions the most 3' position possible should be arbitrarily assigned the repeat has to be described as a GGC repeat. On the basis of the coding DNA reference sequence (GenBank NM_002024.4), c.-128GGC(79) describes the presence of an extended GGC-repeat of exactly 79 units and c.-128GGC(1000) describes the presence of an extended GGC-repeat of about 1000 units (the ‘()’ is used to indicate uncertainties).
The technique used should be clearly indicated (Southern blot, PCR, TP-PCR, etc) with the reference of the publication which described it and the reference of the kit and the provider in such case.
A statement of the limitations/sensitivity of the technique(s) used should appear clearly in the conclusion section of the molecular diagnosis report. Whenever an exact number of the CGGs is reported it should be accompanied by a statement of the testing laboratory’s accuracy of sizing.
Some laboratories perform ‘pre-screening’ tests with a method which is not able to detect the whole range of expansions. If such a test is inconclusive, then a preliminary report can be issued that should provide information about the test’s allele range of detection (ie, report the possibility of the presence of an expansion above the sensitivity of the test used) and should report that a complementary analysis has to be done to determine the actual genotype (possibility of PCR failure, determination of the size range of the allele).
When a repeat sized around 200 CGGs is found and methylation testing has not been done or is not conclusive, the laboratory should not decide whether this is a premutation or a full mutation, but must consider both (in order to not give incomplete/wrong advice to the consultant (or ‘referring clinician’)).
When the genotype is determined, although local policy can vary with regard to reporting, suggested items to be included in the report are set out in Table 2, depending upon the reason for referral.
Concluding remarks
These guidelines are based on the knowledge acquired from peer reviewed and published data, as well as observations of the authors in their practice (MoMN’s data) and experience in the EMQN EQA for FXS, FXPOI, and FXTAS. These guidelines can only provide a snapshot of current knowledge at the time of manuscript submission. Readers are advised to keep up with the literature.
References
Hill MK, Archibald AD, Cohen J, Metcalfe SA : A systematic review of population screening for fragile X syndrome. Genet Med 2010; 12: 411–412.
Sherman SL : Premature ovarian failure in the fragile X syndrome. Am J Med Genet 2000; 97: 189–194.
Sullivan AK, Marcus M, Epstein MP et al. Association of FMR1 repeat size with ovarian dysfunction. Hum Reprod 2005; 20: 402–412.
Conway GS, Payne NN, Webb J, Murray A, Jacobs PA : Fragile X premutation screening in women with premature ovarian failure. Hum Reprod 1998; 13: 1184–1187.
Murray A, Webb J, Grimley S, Conway G, Jacobs P : Studies of FRAXA and FRAXE in women with premature ovarian failure. J Med Genet 1998; 35: 637–640.
Marozzi A, Vegetti W, Manfredini E et al. Association between idiopathic premature ovarian failure and fragile X premutation. Hum Reprod 2000; 15: 197–202.
Sullivan SD, Welt C, Sherman S : FMR1 and the continuum of primary ovarian insufficiency. Semin Reprod Med 2011; 29: 299–307.
Hagerman RJ, Leehey M, Heinrichs W et al. Intention tremor, parkinsonism, and generalized brain atrophy in male carriers of fragile X. Neurology 2001; 57: 127–130.
Jacquemont S, Hagerman RJ, Leehey M et al. Fragile X premutation tremor/ataxia syndrome: molecular, clinical, and neuroimaging correlates. Am J Hum Genet 2003; 72: 869–878.
Hagerman RJ, Leavitt BR, Farzin F et al. Fragile-X-associated tremor/ataxia syndrome (FXTAS) in females with the FMR1 premutation. Am J Hum Genet 2004; 74: 1051–1056.
Berry-Kravis E, Abrams L, Coffey SM et al. Fragile X-associated tremor/ataxia syndrome: clinical features, genetics, and testing guidelines. Mov Disord 2007; 22: 2018–2030, quiz 2140.
Rodriguez-Revenga L, Madrigal I, Pagonabarraga J et al. Penetrance of FMR1 premutation associated pathologies in fragile X syndrome families. Eur J Hum Genet 2009; 17: 1359–1362.
Tassone F, Greco CM, Hunsaker MR et al. Neuropathological, clinical and molecular pathology in female fragile X premutation carriers with and without FXTAS. Genes Brain Behav 2012; 11: 577–585.
Verkerk AJ, Pieretti M, Sutcliffe JS et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell 1991; 65: 905–914.
Fu YH, Kuhl DP, Pizzuti A et al. Variation of the CGG repeat at the fragile X site results in genetic instability: resolution of the Sherman paradox. Cell 1991; 67: 1047–1058.
Ashley Jr CT, Warren ST : Trinucleotide repeat expansion and human disease. Annu Rev Genet 1995; 29: 703–728.
Willemsen R, Levenga J, Oostra BA : CGG repeat in the FMR1 gene: size matters. Clin Genet 2011; 80: 214–225.
Eichler EE, Richards S, Gibbs RA, Nelson DL : Fine structure of the human FMR1 gene. Hum Mol Genet 1993; 2: 1147–1153.
Eichler EE, Holden JJ, Popovich BW et al. Length of uninterrupted CGG repeats determines instability in the FMR1 gene. Nat Genet 1994; 8: 88–94.
Kunst CB, Warren ST : Cryptic and polar variation of the fragile X repeat could result in predisposing normal alleles. Cell 1994; 77: 853–861.
Nolin SL, Sah S, Glicksman A et al. Fragile X AGG analysis provides new risk predictions for 45-69 repeat alleles. Am J Med Genet A 2013; 161: 771–778.
Tassone F, Hagerman RJ, Taylor AK, Gane LW, Godfrey TE, Hagerman PJ : Elevated levels of FMR1 mRNA in carrier males: a new mechanism of involvement in the fragile-X syndrome. Am J Hum Genet 2000; 66: 6–15.
Tassone F, Hagerman RJ, Garcia-Arocena D, Khandjian EW, Greco CM, Hagerman PJ : Intranuclear inclusions in neural cells with premutation alleles in fragile X associated tremor/ataxia syndrome. J Med Genet 2004; 41: e43.
Todd PK, Oh SY, Krans A et al. CGG repeat-associated translation mediates neurodegeneration in fragile X tremor ataxia syndrome. Neuron 2013; 78: 440–455.
Ennis S, Ward D, Murray A : Nonlinear association between CGG repeat number and age of menopause in FMR1 premutation carriers. Eur J Hum Genet 2006; 14: 253–255.
Wittenberger MD, Hagerman RJ, Sherman SL et al. The FMR1 premutation and reproduction. Fertil Steril 2007; 87: 456–465.
Tejada MI, Garcia-Alegria E, Bilbao A et al. Analysis of the molecular parameters that could predict the risk of manifesting premature ovarian failure in female premutation carriers of fragile X syndrome. Menopause 2008; 15: 945–949.
Jacquemont S, Hagerman RJ, Leehey MA et al. Penetrance of the fragile X-associated tremor/ataxia syndrome in a premutation carrier population. JAMA 2004; 291: 460–469.
Brega AG, Reynolds A, Bennett RE et al. Functional status of men with the fragile X premutation, with and without the tremor/ataxia syndrome (FXTAS). Int J Geriatr Psychiatry 2009; 24: 1101–1109.
Sevin M, Kutalik Z, Bergman S et al. Penetrance of marked cognitive impairment in older male carriers of the FMR1 gene premutation. J Med Genet 2009; 46: 818–824.
Pieretti M, Zhang FP, Fu YH et al. Absence of expression of the FMR-1 gene in fragile X syndrome. Cell 1991; 66: 817–822.
Rousseau F, Heitz D, Tarleton J et al. A multicenter study on genotype-phenotype correlations in the fragile X syndrome, using direct diagnosis with probe StB12.3: the first 2253 cases. Am J Hum Genet 1994; 55: 225–237.
Wohrle D, Hennig I, Vogel W, Steinbach P : Mitotic stability of fragile X mutations in differentiated cells indicates early post-conceptional trinucleotide repeat expansion. Nat Genet 1993; 4: 140–142.
Glaser D, Wohrle D, Salat U, Vogel W, Steinbach P : Mitotic behavior of expanded CGG repeats studied on cultured cells: further evidence for methylation-mediated triplet repeat stability in fragile X syndrome. Am J Med Genet 1999; 84: 226–228.
Wohrle D, Salat U, Hameister H, Vogel W, Steinbach P : Demethylation, reactivation, and destabilization of human fragile X full-mutation alleles in mouse embryocarcinoma cells. Am J Hum Genet 2001; 69: 504–515.
Schmucker B, Seidel J : Mosaicism for a full mutation and a normal size allele in two fragile X males. Am J Med Genet 1999; 84: 221–225.
Orrico A, Galli L, Dotti MT, Plewnia K, Censini S, Federico A : Mosaicism for full mutation and normal-sized allele of the FMR1 gene: a new case. Am J Med Genet 1998; 78: 341–344.
Tassone F, Hagerman RJ, Loesch DZ, Lachiewicz A, Taylor AK, Hagerman PJ : Fragile X males with unmethylated, full mutation trinucleotide repeat expansions have elevated levels of FMR1 messenger RNA. Am J Med Genet 2000; 94: 232–236.
Hagerman RJ, Hull CE, Safanda JF et al. High functioning fragile X males: demonstration of an unmethylated fully expanded FMR-1 mutation associated with protein expression. Am J Med Genet 1994; 51: 298–308.
De Boulle K, Verkerk AJ, Reyniers E et al. A point mutation in the FMR-1 gene associated with fragile X mental retardation. Nat Genet 1993; 3: 31–35.
Lugenbeel KA, Peier AM, Carson NL, Chudley AE, Nelson DL : Intragenic loss of function mutations demonstrate the primary role of FMR1 in fragile X syndrome. Nat Genet 1995; 10: 483–485.
Gedeon AK, Baker E, Robinson H et al. Fragile X syndrome without CCG amplification has an FMR1 deletion. Nat Genet 1992; 1: 341–344.
Wohrle D, Kotzot D, Hirst MC et al. A microdeletion of less than 250 kb, including the proximal part of the FMR-I gene and the fragile-X site, in a male with the clinical phenotype of fragile-X syndrome. Am J Hum Genet 1992; 51: 299–306.
Tarleton J, Richie R, Schwartz C, Rao K, Aylsworth AS, Lachiewicz A : An extensive de novo deletion removing FMR1 in a patient with mental retardation and the fragile X syndrome phenotype. Hum Mol Genet 1993; 2: 1973–1974.
Trottier Y, Imbert G, Poustka A, Fryns JP, Mandel JL : Male with typical fragile X phenotype is deleted for part of the FMR1 gene and for about 100 kb of upstream region. Am J Med Genet 1994; 51: 454–457.
Meijer H, de Graaff E, Merckx DM et al. A deletion of 1.6 kb proximal to the CGG repeat of the FMR1 gene causes the clinical phenotype of the fragile X syndrome. Hum Mol Genet 1994; 3: 615–620.
Hirst M, Grewal P, Flannery A et al. Two new cases of FMR1 deletion associated with mental impairment. Am J Hum Genet 1995; 56: 67–74.
Hammond LS, Macias MM, Tarleton JC, Shashidhar Pai G : Fragile X syndrome and deletions in FMR1: new case and review of the literature. Am J Med Genet 1997; 72: 430–434.
Coffee B, Ikeda M, Budimirovic DB, Hjelm LN, Kaufmann WE, Warren ST : Mosaic FMR1 deletion causes fragile X syndrome and can lead to molecular misdiagnosis: a case report and review of the literature. Am J Med Genet A 2008; 146A: 1358–1367.
Collins SC, Coffee B, Benke PJ et al. Array-based FMR1 sequencing and deletion analysis in patients with a fragile X syndrome-like phenotype. PLoS One 2010; 5: e9476.
Brown WT, Houck Jr GE, Ding X et al. Reverse mutations in the fragile X syndrome. Am J Med Genet 1996; 64: 287–292.
Mornet E, Chateau C, Taillandier A, Simon-Bouy B, Serre JL : Recurrent and unexpected segregation of the FMR1 CGG repeat in a family with fragile X syndrome. Hum Genet 1996; 97: 512–515.
Vaisanen ML, Haataja R, Leisti J : Decrease in the CGGn trinucleotide repeat mutation of the fragile X syndrome to normal size range during paternal transmission. Am J Hum Genet 1996; 59: 540–546.
Gasteiger M, Grasbon-Frodl E, Neitzel B, Kooy F, Holinski-Feder E : FMR1 gene deletion/reversion: a pitfall of fragile X carrier testing. Genet Test 2003; 7: 303–308.
Tabolacci E, Pomponi MG, Pietrobono R, Chiurazzi P, Neri G : A unique case of reversion to normal size of a maternal premutation FMR1 allele in a normal boy. Eur J Hum Genet 2008; 16: 209–214.
Heitz D, Devys D, Imbert G, Kretz C, Mandel JL : Inheritance of the fragile X syndrome: size of the fragile X premutation is a major determinant of the transition to full mutation. J Med Genet 1992; 29: 794–801.
Fisch GS, Snow K, Thibodeau SN et al. The fragile X premutation in carriers and its effect on mutation size in offspring. Am J Hum Genet 1995; 56: 1147–1155.
Nolin SL, Brown WT, Glicksman A et al. Expansion of the fragile X CGG repeat in females with premutation or intermediate alleles. Am J Hum Genet 2003; 72: 454–464.
Nolin SL, Glicksman A, Ding X et al. Fragile X analysis of 1112 prenatal samples from 1991 to 2010. Prenat Diagn 2011; 31: 925–931.
Fernandez-Carvajal I, Lopez Posadas B, Pan R, Raske C, Hagerman PJ, Tassone F : Expansion of an FMR1 grey-zone allele to a full mutation in two generations. J Mol Diagn 2009; 11: 306–310.
Reyniers E, Vits L, De Boulle K et al. The full mutation in the FMR-1 gene of male fragile X patients is absent in their sperm. Nat Genet 1993; 4: 143–146.
Willems PJ, Van Roy B, De Boulle K et al. Segregation of the fragile X mutation from an affected male to his normal daughter. Hum Mol Genet 1992; 1: 511–515.
Mulley JC, Yu S, Gedeon AK et al. Experience with direct molecular diagnosis of fragile X. J Med Genet 1992; 29: 368–374.
Rousseau F, Robb LJ, Rouillard P, Der Kaloustian VM : No mental retardation in a man with 40% abnormal methylation at the FMR-1 locus and transmission of sperm cell mutations as premutations. Hum Mol Genet 1994; 3: 927–930.
Kambouris M, Snow K, Thibodeau S, Bluhm D, Green M, Feldman GL : Segregation of the fragile X mutation from a male with a full mutation: unusual somatic instability in the FMR-1 locus. Am J Med Genet 1996; 64: 404–407.
Zeesman S, Zwaigenbaum L, Whelan DT, Hagerman RJ, Tassone F, Taylor SA : Paternal transmission of fragile X syndrome. Am J Med Genet A 2004; 129A: 184–189.
Steinbach D, Steinbach P : No evidence of paternal transmission of fragile X syndrome. Am J Med Genet A 2005; 136: 107–108, author reply 109-110.
Saul RA, Tarleton JC . FMR1-Related Disorders. GeneReviews™ 2012. http://www.ncbi.nlm.nih.gov/books/NBK1384/.
Kronquist KE, Sherman SL, Spector EB : Clinical significance of tri-nucleotide repeats in Fragile X testing: a clarification of American College of Medical Genetics guidelines. Genet Med 2008; 10: 845–847.
McConkie-Rosell A, Abrams L, Finucane B et al. Recommendations from multi-disciplinary focus groups on cascade testing and genetic counseling for fragile X-associated disorders. J Genet Couns 2007; 16: 593–606.
McConkie-Rosell A, Finucane B, Cronister A, Abrams L, Bennett RL, Pettersen BJ : Genetic counseling for fragile x syndrome: updated recommendations of the national society of genetic counselors. J Genet Couns 2005; 14: 249–270.
Levesque S, Dombrowski C, Morel ML et al. Screening and instability of FMR1 alleles in a prospective sample of 24449 mother-newborn pairs from the general population. Clin Genet 2009; 76: 511–523.
Zuniga A, Juan J, Mila M, Guerrero A : Expansion of an intermediate allele of the FMR1 gene in only two generations. Clin Genet 2005; 68: 471–473.
Terracciano A, Pomponi MG, Marino GM et al. Expansion to full mutation of a FMR1 intermediate allele over two generations. Eur J Hum Genet 2004; 12: 333–336.
Yrigollen CM, Durbin-Johnson B, Gane L et al. AGG interruptions within the maternal FMR1 gene reduce the risk of offspring with fragile X syndrome. Genet Med 2012; 14: 729–736.
Madrigal I, Xuncla M, Tejada MI et al. Intermediate FMR1 alleles and cognitive and/or behavioural phenotypes. Eur J Hum Genet 2011; 19: 921–923.
Knight SJ, Flannery AV, Hirst MC et al. Trinucleotide repeat amplification and hypermethylation of a CpG island in FRAXE mental retardation. Cell 1993; 74: 127–134.
Wang Q, Green E, Bobrow M, Mathew CG : A rapid, non-radioactive screening test for fragile X mutations at the FRAXA and FRAXE loci. J Med Genet 1995; 32: 170–173.
Biancalana V, Taine L, Bouix JC et al. Expansion and methylation status at FRAXE can be detected on EcoRI blots used for FRAXA diagnosis: analysis of four FRAXE families with mild mental retardation in males. Am J Hum Genet 1996; 59: 847–854.
Jacquemont S, Birnbaum S, Redler S, Steinbach P, Biancalana V : Clinical utility gene card for: fragile X mental retardation syndrome, fragile X-associated tremor/ataxia syndrome and fragile X-associated primary ovarian insufficiency. Eur J Hum Genet 2011; 19.
Rousseau F, Heitz D, Biancalana V et al. Direct diagnosis by DNA analysis of the fragile X syndrome of mental retardation. N Engl J Med 1991; 325: 1673–1681.
Gold B, Radu D, Balanko A, Chiang CS : Diagnosis of Fragile X syndrome by Southern blot hybridization using a chemiluminescent probe: a laboratory protocol. Mol Diagn 2000; 5: 169–178.
Nolin SL, Ding XH, Houck GE, Brown WT, Dobkin C : Fragile X full mutation alleles composed of few alleles: implications for CGG repeat expansion. Am J Med Genet A 2008; 146A: 60–65.
Biancalana V, Macpherson J : Molecular Diagnosis of Genetic Disease. Methods in Molecular Medicine. Neurological Applications 1. Totowa, NJ, USA: Humana Press, 2004; vol 92: 157–182.
Storm K, Handig I, Reyniers E, Oostra BA, Kooy RF, Willems PJ : Incomplete EcoRI digestion may lead to false diagnosis of fragile X syndrome. Hum Genet 1998; 102: 54–56.
Mila M, Castellvi-Bel S, Sanchez A et al. Rare variants in the promoter of the fragile X syndrome gene (FMR1). Mol Cell Probes 2000; 14: 115–119.
Daly TM, Rafii A, Martin RA, Zehnbauer BA : Novel polymorphism in the FMR1 gene resulting in a ‘pseudodeletion’ of FMR1 in a commonly used fragile X assay. J Mol Diagn 2000; 2: 128–131.
Tarleton J, Kenneson A, Taylor AK et al. A single base alteration in the CGG repeat region of FMR1: possible effects on gene expression and phenotype. J Med Genet 2002; 39: 196–200.
Thyagarajan B, Bower M, Berger M, Jones S, Dolan M, Wang X : A novel polymorphism in the FMR1 gene: implications for clinical testing of fragile X syndrome. Arch Pathol Lab Med 2008; 132: 95–98.
Liang S, Bass HN, Gao H, Astbury C, Jamehdor MR, Qu Y : A pseudo-full mutation identified in fragile X assay reveals a novel base change abolishing an EcoRI restriction site. J Mol Diagn 2008; 10: 469–474.
Brown WT, Houck Jr GE, Jeziorowska A et al. Rapid fragile X carrier screening and prenatal diagnosis using a nonradioactive PCR test. JAMA 1993; 270: 1569–1575.
Weinhausel A, Haas OA : Evaluation of the fragile X (FRAXA) syndrome with methylation-sensitive PCR. Hum Genet 2001; 108: 450–458.
Zhou Y, Law HY, Boehm CD et al. Robust fragile X (CGG)n genotype classification using a methylation specific triple PCR assay. J Med Genet 2004; 41: e45.
Tassone F, Pan R, Amiri K, Taylor AK, Hagerman PJ : A rapid polymerase chain reaction-based screening method for identification of all expanded alleles of the fragile X (FMR1) gene in newborn and high-risk populations. J Mol Diagn 2008; 10: 43–49.
Hantash FM, Goos DG, Tsao D et al. Qualitative assessment of FMR1 (CGG)n triplet repeat status in normal, intermediate, premutation, full mutation, and mosaic carriers in both sexes: implications for fragile X syndrome carrier and newborn screening. Genet Med 2010; 12: 162–173.
Lyon E, Laver T, Yu P et al. A simple, high-throughput assay for Fragile X expanded alleles using triple repeat primed PCR and capillary electrophoresis. J Mol Diagn 2010; 12: 505–511.
Chen L, Hadd A, Sah S et al. An information-rich CGG repeat primed PCR that detects the full range of fragile X expanded alleles and minimizes the need for southern blot analysis. J Mol Diagn 2012; 12: 589–600.
Mononen T, von Koskull H, Airaksinen RL, Juvonen V : A novel duplication in the FMR1 gene: implications for molecular analysis in fragile X syndrome and repeat instability. Clin Genet 2007; 72: 528–531.
Hegde MR, Chong B, Fawkner M et al. Microdeletion in the FMR-1 gene: an apparent null allele using routine clinical PCR amplification. J Med Genet 2001; 38: 624–629.
Braida C, Stefanatos RK, Adam B et al. Variant CCG and GGC repeats within the CTG expansion dramatically modify mutational dynamics and likely contribute toward unusual symptoms in some myotonic dystrophy type 1 patients. Hum Mol Genet 2012; 19: 1399–1412.
Musova Z, Mazanec R, Krepelova A et al. Highly unstable sequence interruptions of the CTG repeat in the myotonic dystrophy gene. Am J Med Genet A 2009; 149A: 1365–1374.
Teo CR, Law HY, Lee CG, Chong SS : Screening for CGG repeat expansion in the FMR1 gene by melting curve analysis of combined 5' and 3' direct triplet-primed PCRs. Clin Chem 2012; 58: 568–579.
van den Ouweland AM, Deelen WH, Kunst CB et al. Loss of mutation at the FMR1 locus through multiple exchanges between maternal X chromosomes. Hum Mol Genet 1994; 3: 1823–1827.
Malzac P, Biancalana V, Voelckel MA et al. Unexpected inheritance of the (CGG)n trinucleotide expansion in a fragile X syndrome family. Eur J Hum Genet 1996; 4: 8–12.
Losekoot M, Hoogendoorn E, Olmer R et al. Prenatal diagnosis of the fragile X syndrome: loss of mutation owing to a double recombinant or gene conversion event at the FMR1 locus. J Med Genet 1997; 34: 924–926.
Willemsen R, Mohkamsing S, de Vries B et al. Rapid antibody test for fragile X syndrome. Lancet 1995; 345: 1147–1148.
LaFauci G, Adayev T, Kascsak R et al. Fragile X screening by quantification of FMRP in dried blood spots by a Luminex immunoassay. J Mol Diagn 2013; 15: 508–517.
Devys D, Biancalana V, Rousseau F, Boue J, Mandel JL, Oberle I : Analysis of full fragile X mutations in fetal tissues and monozygotic twins indicate that abnormal methylation and somatic heterogeneity are established early in development. Am J Med Genet 1992; 43: 208–216.
Hawkins M, Boyle J, Wright KE et al. Preparation and validation of the first WHO international genetic reference panel for Fragile X syndrome. Eur J Hum Genet 2011; 19: 10–17.
Oostra BA, Jacky PB, Brown WT, Rousseau F : Guidelines for the diagnosis of fragile X syndrome. National Fragile X Foundation. J Med Genet 1993; 30: 410–413.
Acknowledgements
The first version of the guidelines was established at the EMQN Best Practice Meeting, held 23–24 November 2001 in Strasbourg, France, and updated again in January 2006. This new update occurred in December 2013 after distribution of the revised version to participants of the FRAX EQA. We would like to acknowledge following people for carefully reading the manuscript and providing useful comments and additional information: D Barton, D Bodmer, N Canson, C Clabby, S Ceylaner on behalf of the Turkish Medical Genetic Association, I Delon, A DeSandre, A Ferlini on behalf of the Italian Molecular Genetics working group (SIGU—A Murgia, A Mesoraca, C Gervasini, C Lapucci, MC Patrosso, F Gualandi, F Brancati, G Police, G Merla, G Sabbatini, I Sani, M Seia, M Neri, MA Melis, M Grasso, P Primignani, R Stuppia, S Russo, V Bizzarri), L Jenkins, W Just, P Johnels, P Jorge, T Kahre, J MacPherson, M Milà Recasens on behalf of the Spanish expert groups working on Fragile X-associated Disorders, belonging to the AEGH—GIRMOGEN—CIBERER, A Murray, M. Morris, K Piippo, JK Ploosvan Amstel, R Santos, H Sawyer, S Seneca, A Sharif, M Sweeney, E Voorhoeve on behalf of the Dutch VKGL commission for quality control and Y Wallis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Biancalana, V., Glaeser, D., McQuaid, S. et al. EMQN best practice guidelines for the molecular genetic testing and reporting of fragile X syndrome and other fragile X-associated disorders. Eur J Hum Genet 23, 417–425 (2015). https://doi.org/10.1038/ejhg.2014.185
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2014.185
This article is cited by
-
Fragile X premutation carrier screening in Pakistani preconception women in primary care consultation
BMC Women's Health (2022)
-
Assessing clinical utility of preconception expanded carrier screening regarding residual risk for neurodevelopmental disorders
npj Genomic Medicine (2022)
-
FMR1 expression in human granulosa cells increases with exon 1 CGG repeat length depending on ovarian reserve
Reproductive Biology and Endocrinology (2018)
-
Classical fragile-X phenotype in a female infant disclosed by comprehensive genomic studies
BMC Medical Genetics (2018)
-
Leitlinien zur molekulargenetischen Diagnostik: Fragiles-X Syndrom und andere FMR1-assoziierte Syndrome
Medizinische Genetik (2017)