Abstract
The phenotypic variability of hypertrophic cardiomyopathy (HCM) in patients with identical pathogenic mutations suggests additional modifiers. In view of the regulatory role in cardiac function, blood pressure, and electrolyte homeostasis, polymorphisms in the renin–angiotensin–aldosterone system (RAAS) are candidates for modifying phenotypic expression. In order to investigate whether RAAS polymorphisms modulate HCM phenotype, we selected a large cohort of carriers of one of the three functionally equivalent truncating mutations in the MYBPC3 gene. Family-based association analysis was performed to analyze the effects of five candidate RAAS polymorphisms (ACE, rs4646994; AGTR1, rs5186; CMA, rs1800875; AGT, rs699; CYP11B2, rs1799998) in 368 subjects carrying one of the three mutations in the MYBPC3 gene. Interventricular septum (IVS) thickness and Wigle score were assessed by 2D-echocardiography. SNPs in the RAAS system were analyzed separately and combined as a pro-left ventricular hypertrophy (LVH) score for effects on the HCM phenotype. Analyzing the five polymorphisms separately for effects on IVS thickness and Wigle score detected two modest associations. Carriers of the CC genotype in the AGT gene had less pronounced IVS thickness compared with CT and TT genotype carriers. The DD polymorphism in the ACE gene was associated with a high Wigle score (P=0.01). No association was detected between the pro-LVH score and IVS thickness or Wigle score. In conclusion, in contrast to previous studies, in our large study population of HCM patients with functionally equivalent mutations in the MYBPC3 gene we did not find major effects of genetic variation within the genes of the RAAS system on phenotypic expression of HCM.
Similar content being viewed by others
Introduction
Hypertrophic cardiomyopathy (HCM) is the most common inheritable cardiac disorder with a phenotypic prevalence of 1:500.1 It is defined by the presence of left ventricular hypertrophy (LVH) in the absence of loading conditions (hypertension, valve disease) sufficient to cause the observed abnormality.2 Hundreds of mutations scattered among at least 25 HCM susceptibility genes encoding various sarcomere, Z-disk, calcium-handling, and mitochondrial proteins are known to cause HCM in 60% of cases.3
In the Netherlands, approximately one third of all HCM cases are caused by carriership of any one of the three founder mutations in the myosin-binding protein C gene (MYBPC3). All three are truncating mutations, namely c.2373dupG, c.2827C>T (p.Arg943X), and c.2864_2865delCT.4, 5, 6 Immunoblotting studies on myocardial tissue from carriers of the c.2373dupG and c.2864_2865delCT truncating mutations have demonstrated absence of the truncated MyBPC3 protein product coupled to a decreased total (full-length) MyBPC3 content, strongly suggesting a mechanism of haploinsufficiency.5 Although not functionally investigated, the c.2827C>T mutation, which introduces a premature stop codon at residue 943, encodes for a similarly C-terminally truncated protein (Figure 1), and is therefore also expected to lead to haploinsufficiency. These three founder mutations may therefore be considered functionally equivalent.
Schematic representation of MyBPC3 structure and the effects of the three founder mutations on the structure of the protein. Adapted from van Dijk et al.5
Extensive phenotypic variability exists among HCM mutation carriers. Even individuals with the same underlying genetic substrate show a broad spectrum of clinical manifestations.7, 8 This indicates that HCM features are not solely determined by the nature of the pathogenic mutation and that additional environmental and/or other genetic factors (genetic modifiers) have a role in the clinical expression of the disease.
Genetic variants in the renin–angiotensin–aldosterone system (RAAS) are considered candidates for these modifying effects. The RAAS system contributes to LVH through effects mediated by circulating angiotensin as well as local activation of RAAS in the myocardium.9 Angiotensin (Ang) I, produced from angiotensinogen (AGT), is converted to Ang II predominantly by angiotensin-converting enzyme (ACE) and possibly by chymase 1 (CMA1).10 Ang II binds primarily to the Ang II type 1 receptor (AGTR1) to promote cell growth and hypertrophy. It also stimulates aldosterone by aldosterone synthase (CYP11B2) synthesis, thereby increasing the release of aldosterone, which promotes fluid retention and cardiac fibrosis.11
Previous studies suggested a role for specific genetic variants in genes encoding components of the RAAS pathway in modulation of the severity of LVH in patients with HCM.12, 13, 14 In particular, two studies investigated five candidate polymorphisms within these genes in HCM patients with an identified HCM-causing mutation. The RAAS polymorphisms tested in these studies included: (1) an insertion/deletion (I/D) polymorphism in intron 16 of the ACE gene (rs4646994), where the D-allele was considered as the pro-LVH allele, (2) an A>C polymorphism at position 1166 of the AGTR1 gene (rs5186), where the C-allele was considered as the pro-LVH allele, (3) an A>G polymorphism at position 1903 of the CMA1 gene (rs1800875), where the A-allele was considered as the pro-LVH allele, (4) a T>C (p.M235T) polymorphism in the AGT gene (rs699), where the C-allele was considered as the pro-LVH allele, and (5) a C>T polymorphism at position 344 of the CYP11B2 gene (rs1799998), where the C-allele was considered as the pro-LVH allele.
The first of these two studies was carried out in a small number (n=26) of carriers of the MYBPC3-c.2373dupG mutation from a single family. In this study, c.2373dupG mutation carriers that harbored one or more pro-LVH RAAS polymorphisms genotypes (n=16 individuals) had greater left ventricular muscle mass and interventricular septum (IVS) thickness compared with those that harbored no pro-LVH genotypes (n=10).13 This study also provided some evidence for a pro-LVH effect of these polymorphisms when assessed individually.
The second study was carried out in a cohort of 389 unrelated patients with HCM, of which 63 and 54 patients, respectively, carried a mutation in the MYBPC3 and MYH7 HCM-associated genes.14 In this study, although the ACE I/D polymorphism displayed no effect on any LVH parameter in the entire cohort, subset analysis of the MYBPC3 and MYH7 genetic subtypes demonstrated a pro-LVH effect of the DD-ACE genotype in the MYBPC3-HCM subtype. In this study, there was some evidence that the burden of pro-LVH genotypes was associated with an increased left ventricular wall thickness, although this was only present in the group of patients that were negative for myofilament gene mutations.
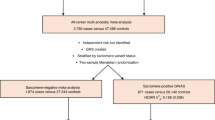
The results of these previous studies addressing effects of genetic modifiers in HCM have, however, been difficult to interpret because of the small sample size and/or by inclusion of a genetically heterogeneous study population with respect to the primary genetic defect. In this study, we used a large cohort of subjects having one of the three functionally equivalent truncating founder mutations in the MYBPC3 gene, to investigate whether the five RAAS gene polymorphisms investigated in these previous studies modulate echocardiographic features of HCM.
Materials and methods
Study population
In the Netherlands, genetic counseling and genetic testing is offered to all HCM patients visiting cardiogenetics outpatient clinics. Upon the identification of the causal mutation in a proband, genetic testing is extended to relatives following appropriate genetic counselling (cascade screening).15, 16 For this study all subjects, including probands and relatives, carrying one of the three truncating founder mutations in the MYBPC3 gene (c.2373dupG, c.2864_2865delCT, c.2827C>T) were selected from two university hospitals in the Netherlands; the Academic Medical Center in Amsterdam and the Erasmus Medical Center in Rotterdam. In this way, 368 carriers of equally pathogenetic MYPBC3 mutations were included. All subjects were normotensive (blood pressure <140/90 mm Hg) and did not take medication known to influence the RAAS. All subjects provided written informed consent. The study complies with the declaration of Helsinki, and the local review boards of the respective hospitals approved the study.
Echocardiographic evaluation
Echocardiography was performed in all subjects using commercially available equipment. The acquired data were digitally stored and subsequently analyzed by two physicians who were blinded to the clinical and genetic data. IVS thickness was measured in diastole from the parasternal short-axis view at the level of the papillary muscles. For relatives ≥16 years a IVS thickness ≥13 mm was considered as abnormal.17 For subjects <16 years IVS thickness was corrected for height and weight and was considered abnormal if the z-score was >2. The extent of hypertrophy was assessed by a semi-quantitative score method developed by Wigle et al.18 A maximum of 10 points were given: 1–4 points for IVS thickness (one point for IVS thickness between 15–19 mm; two points for IVS thickness between 20–24 mm; three points for IVS thickness 25–29 mm and four points if IVS thickness ≥30 mm), two points for extension of hypertrophy beyond the level of the papillary muscles (basal two thirds of the IVS), two points for extension of hypertrophy to the apex (total IVS involvement), and two points for extension of hypertrophy into the lateral wall.
SNP genotyping
The five polymorphisms investigated in this study were the same as those studied previously by Ortlepp et al13 and by Perkins et al,14 that is (1) rs4646994 in the ACE gene, (2) rs5186 in AGTR1, (3) rs1800875 in CMA1 gene, (4) rs699 in AGT, and (5) rs1799998 in CYP11B2. Patient genomic DNA was extracted from peripheral blood lymphocytes using standard protocols. Genotyping was carried out as described previously. Pro-LVH genotypes were defined as described previously, namely as DD-ACE, CC-AGTR1, AA-CMA, CC-AGT, and CC-CYP11B2. The pro-LVH score was calculated for each patient by adding the number of pro-LVH genotypes present.13, 14
Statistical analyses
Phenotypic data for probands and relatives that was normally distributed (Shapiro–Wilk statistic W>0.9) are reported as mean±SD, otherwise as median with interquartile range. Pedigree information was available for all related subjects. Allele frequencies of polymorphisms tested in the study population were compared with those reported for the CEU population in the 1000 Genomes database using a Pearson χ2 test.
We assumed that each polymorphism–phenotype relationship followed a recessive genetic model as previously reported.14, 15 Effects on IVS thickness and the ranked Wigle score were estimated using a linear mixed model with adjustment for sex, age, and proband status, whereas effects on the dichotomous variables IVS thickness ≥13 or ≥30 mm were estimated using a logistic regression model with adjustment for sex and age. Next to models with a single SNP or the pro-LVH score, a model with all five SNPs and their interactions was also used. To account for the relatedness of study subjects, either the linear mixed model from the Kinship package or the generalized estimation equations from the geepack package in R (R foundation for Statistical Computing, Vienna, Austria) were used. P-values<0.05 were considered significant.
On the basis of the sample size (n=368), our study had 90% power to detect a 0.30 mm difference in IVS thickness between the RAAS polymorphism genotype groups and a correlation coefficient of 0.167 (±3% explained variance) between IVS thickness and the pro-LVH score (α=0.05 two-sided).
Results
Study population
DNA and echocardiography data were available for 368 carriers of one of the three Dutch MYBC3 founder mutations, including 100 probands and 268 relatives. The age distribution of probands and relatives was similar (Table 1). By definition, all probands had an IVS thickness ≥13 mm. Extreme hypertrophy (IVS thickness ≥30 mm), a known risk factor for sudden death was present in nine (10%) probands.19, 20 There was a male preponderance in probands compared with the relatives (64 vs 47%, P=0.007). LVH (defined as IVS≥13 mm)16 was present in 107 (40%) of relatives and was extreme in 1 (0.4%) relative.
The MYBPC3 founder mutations in the study population are presented in Table 2. The most common founder mutation was c.2373dupG, present in 70% of the individuals.
Influence of age, sex, and proband status
Proband status, age, and gender had a significant effect on IVS thickness. Probands displayed a greater mean IVS thickness compared with relatives (22±5 vs 13±4 mm) (Table 1). Although in the relatives group, IVS thickness was greater in older individuals; within the proband group, it was smaller in the older individuals (Figure 2). This apparent interaction effect was, however, not significant (P=0.76). On average, men had a thicker IVS than women (17±6 vs 14±6 mm; P=0.0014). This influence of male sex is especially clear in the relatives group (Figure 2).
SNP association analyses
The minor allele frequency (MAF) of four of the polymorphisms tested did not differ from that reported for the CEU population in the 1000 Genomes database (P>0.05) (rs5186, MAF of this study=0.31/MAF CEU 1000 Genomes=0.28; rs1800875, MAF=0.52/0.54; rs699, MAF=0.36/0.36; rs1799998, MAF=0.39/0.43). The MAF of rs4646994 (MAF=0.49 this study) was not reported in 1000 Genomes.
The five polymorphisms were analyzed separately and combined as a pro-LVH score for (i) effects on IVS thickness, (ii) association with IVS thickness ≥13 mm, (iii) association with IVS thickness ≥30 mm, and (iv) effects on the Wigle score (Tables 3, 4, 5).
Analyzing the five polymorphisms separately with correction for gender, proband status and age using a recessive genetic model (Table 3) showed an association of the T>C (p.M235T) polymorphism in the AGT gene with IVS thickness (P=0.02); the CC genotype (homozygous for threonine at position 235) was associated with attenuated IVS thickness compared with the other AGT genotypes (TC, TT). As expected from the distribution of septum thickness for the three genotype groups of this polymorphism, applying a dominant genetic model resulted in a more significant association (P=2.4e-04). The DD genotype at the ACE I/D polymorphism was associated with a high Wigle score (P=0.05) as compared with the ID and DD genotypes. Applying an additive or dominant model for the relations between the SNPs and the phenotypes did not reveal any other significant associations. Association analysis results were unchanged when the analysis was restricted to only those patients carrying the most prevalent founder mutation (c.2373dupG, see Supplementary Table). Furthermore, no significant interactions were found between the five polymorphisms for any of the phenotypes tested. No association was detected between pro-LVH score and IVS thickness or Wigle score in probands or relatives (Tables 4 and 5).
Discussion
In a large cohort of carriers of one of the three functionally equivalent truncating Dutch founder mutations in MYBPC3, we found only minor effects of candidate SNPs in the RAAS system on IVS thickness and Wigle score. These effects were limited to (i) an association of the CC genotype of the AGT T>C (p.M235T) polymorphism with a smaller IVS thickness, and (ii) an association of the DD genotype of the ACE I/D polymorphism with a higher Wigle score. There was no effect of the previously described pro-LVH score on IVS thickness or Wigle score.13, 14
The T>C (p.M235T) polymorphism in the AGT gene has been described as a predisposing factor for cardiac hypertrophy in patients with hypertension, in endurance athletes and in sporadic cases of HCM.21, 22, 23 Furthermore, Ortlepp et al13 found an association between the CC genotype of this polymorphism with increased left ventricular mass and increased IVS thickness. The AGT gene encodes angiotensinogen and the C-allele of this polymorphism is associated with elevated AGT serum concentrations.24 Although we found an association between the CC genotype of the AGT T>C polymorphism (p.M235T) and IVS thickness, it is important to note that the direction of the effect in our patient population was opposite to what is predicted based on these previous studies, that is, increased hypertrophy in the presence of elevated AGT concentrations. As the observed association in our study was not supported by a decreased risk for an IVS thickness of ≥13 mm or ≥30 mm, the observed association is suggestive of a spurious association. Indeed, also no association was detected for this polymorphism with Wigle score.
Tissue levels of angiotensin-converting enzyme are increased in patients with the DD-ACE genotype, which is considered to be a pro-LVH genotype.25, 26 Furthermore, the previous study by Perkins et al14 showed that in 63 HCM patients with single (different) mutations in the MYBPC3 gene, the DD-ACE genotype was a significant pro-LVH modifier, being associated with an increased left ventricular wall thickness, and with extreme IVS thickness (>30 mm). Similar findings were reported by Ortlepp et al13 in 26 c.2373dupG mutation carriers from one family. In our study, although we found that the DD-ACE was significantly associated with the Wigle score, suggesting a pro-hypertrophic effect, we did not detect an association with IVS thickness or risk of having an IVS thickness of ≥13 mm or ≥30 mm.
There was no effect of the combined pro-LVH genotypes in the pro-LVH score on IVS thickness or Wigle score. This is in contrast to the report of Ortlepp et al,13 where among the 26 c.2373dupG mutation carriers extent of cardiac hypertrophy was associated with the burden of pro-LVH genotypes. Although the same mutation was present in 257 of the 368 patients (70%) of the current study, we failed to observe a relation between the pro-LVH score and hypertrophy in our much larger study population. Furthermore, we found no major effects of the pro-LVH genotypes when the patient subset with the c.2373dupG was studied separately. Our findings in a much larger set of patients with the same mutation suggest that cardiac hypertrophy in MYBPC3-related HCM is not influenced by the pro-LVH score/genotypes.
IVS thickness in HCM mutation carriers increases progressively with age.8, 9 In our study, this was the case for relatives carrying MYBPC3 mutations but not for probands. A major difference between probands and relatives is their reason for cardiac evaluation. Probands are referred because of symptoms, abnormalities at routine physical examination or electrocardiography, that is, before non-cardiac surgery; whereas relatives are usually asymptomatic and are referred after positive presymptomatic DNA testing. Therefore, a sampling or referral bias may occur; HCM patients with severe IVS thickening at young age are more likely to be referred because of symptoms than those with minimal or moderate thickening. The fact that older probands displayed less extensive IVS thickness than the younger ones might be due to the fact that probands with larger IVS thickness die at younger age (the so-called healthy survivor phenomenon). Besides this possible explanation, it is known that about 5–10% of HCM patients progress to an end-stage form, which is characterized by systolic dysfunction, dilatation of the left ventricle and wall thinning.27, 28
Males and females differ in their presentation of HCM, with cohorts usually having a predominance of males.29, 30, 31 In our study, an effect of gender on age at onset in the relatives was observed: men were affected at younger age than women. This may be explained by a protective role of estrogens in the hypertrophic response and the evidence that exposure of cardiac myocytes to androgen results in hypertrophy.32, 33 Furthermore, the HCM phenotype is influenced by sex hormone receptor variants.34 However, in our study, the sex effect in the probands was less clear, with females tending to be more heavily affected at young age, although one must acknowledge that there was considerable overlap between males and females in this group (Figure 2). This illustrates that there are other, currently unknown modifiers of phenotypic expression in HCM.
In conclusion, we have investigated the role of genetic polymorphisms in genes of the RAAS pathway in a large and genetically homogeneous HCM population. Our findings do not provide support for a marked effect of genetic variation in the RAAS pathway on phenotypic expression of LVH in this disorder. This does not necessarily mean that HCM patients will not benefit from the prescription of drugs blocking the RAAS system.35 However, small studies showing a positive effect of RAAS inhibitors on progression of hypertrophy and fibrosis in HCM need confirmation.36, 37 Furthermore, our study was limited to five candidate polymorphisms and the role of other common genetic variants in explaining phenotypic variability among HCM patients, which may act in a mutation-specific way, merits investigation perhaps in future genome-wide association studies.
References
Maron BJ, Gardin JM, Flack JM et al: Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA study. Coronary artery risk development in (young) adults. Circulation 1995; 92: 785–789.
Task Force for Diagnosis and Treatment of Acute and Chronic Heart Failure of European Society of C, Dickstein K, Cohen-Solal A, Filippatos G et al: Document R. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008; 29: 2388–2442.
Bos JM, Towbin JA, Ackerman MJ : Diagnostic, prognostic, and therapeutic implications of genetic testing for hypertrophic cardiomyopathy. J Am Coll Cardiol 2009; 54: 201–211.
Alders M, Jongbloed R, Deelen W et al: The 2373insG mutation in the MYBPC3 gene is a founder mutation, which accounts for nearly one-fourth of the HCM cases in the Netherlands. Eur Heart J 2003; 24: 1848–1853.
van Dijk SJ, Dooijes D, dos Remedios C et al: Cardiac myosin-binding protein C mutations and hypertrophic cardiomyopathy: haploinsufficiency, deranged phosphorylation, and cardiomyocyte dysfunction. Circulation 2009; 119: 1473–1483.
Michels M, Soliman OI, Kofflard MJ et al: Diastolic abnormalities as the first feature of hypertrophic cardiomyopathy in Dutch myosin-binding protein C founder mutations. JACC Imaging 2009; 2: 58–64.
Michels M, Soliman OI, Phefferkorn J et al: Disease penetrance and risk stratification for sudden cardiac death in asymptomatic hypertrophic cardiomyopathy mutation carriers. Eur Heart J 2009; 30: 2593–2598.
Christiaans I, Birnie E, van Langen IM et al: The yield of risk stratification for sudden cardiac death in hypertrophic cardiomyopathy myosin-binding protein C gene mutation carriers: focus on predictive screening. Eur Heart J 2010; 31: 842–848.
Kim S, Iwao H : Molecular and cellular mechanisms of angiotensin II-mediated cardiovascular and renal diseases. Pharmacol Rev 2000; 52: 11–34.
Tom B, Garrelds IM, Scalbert E, Stegman APA, Boomsma F, Saxena PR, Danser AHJ : ACE- versus chymase-dependent angiotensin II generation in human coronary arteries. Arterioscler Thromb Vasc Biol 2003; 23: 251–256.
Chai W, Hofland J, Jansen PM et al: Steroidogenesis vs, steroid uptake in the heart: do corticosteroids mediate effects via cardiac mineralocorticoid receptors? J Hypertension 2010; 28: 1044–1053.
Orenes-Piñero E, Hernández-Romero D, Jover E, Valdés M, Lip GY, Marín F : Impact of polymorphisms in the renin-angiotensin-aldosterone system on hypertrophic cardiomyopathy. J Renin Angiotensin Aldosterone Syst 2011; 12: 521–530.
Ortlepp JR, Vosberg HP, Reith S et al: Genetic polymorphisms in the renin-angiotensin-aldosterone system associated with expression of left ventricular hypertrophy in hypertrophic cardiomyopathy: a study of five polymorphic genes in a family with a disease causing mutation in the myosin binding protein C gene. Heart 2002; 87: 270–275.
Perkins MJ, Van Driest SL, Ellsworth EG et al: Gene-specific modifying effects of pro-LVH polymorphisms involving the renin-angiotensin-aldosterone system among 389 unrelated patients with hypertrophic cardiomyopathy. Eur Heart J 2005; 26: 2457–2462.
Michels M, Hoedemaekers YM, Kofflard MJ et al: Familial screening and genetic counselling in hypertrophic cardiomyopathy: the Rotterdam experience. Neth Heart J 2007; 15: 184–190.
Christiaans I, Birnie E, Bonsel GJ, Wilde AA, van Langen IM : Uptake of genetic counselling and predictive DNA testing in hypertrophic cardiomyopathy. Eur J Hum Genet 2008; 16: 1201–1207.
McKenna WJ, Spirito P, Desnos M, Dubourg O, Komajda M : Experience from clinical genetics in hypertrophic cardiomyopathy: proposal for new diagnostic criteria in adult members of affected families. Heart 1997; 77: 130–132.
Wigle ED, Sasson Z, Henderson MA et al: Hypertrophic cardiomyopathy. The importance of the site and the extent of hypertrophy. A review. Prog Cardiovasc Dis 1985; 28: 1–83.
Elliott PM, Poloniecki J, Dickie S et al: Sudden death in hypertrophic cardiomyopathy: identification of high risk patients. J Am Coll Cardiol 2000; 36: 2212–2218.
Christiaans I, van Engelen K, van Langen IM et al: Risk stratification for sudden cardiac death in hypertrophic cardiomyopathy: systematic review of clinical risk markers. Europace 2010; 12: 313–321.
Ishanov A, Okamoto H, Yoneya K et al: Angiotensinogen gene polymorphism in Japanese patients with hypertrophic cardiomyopathy. Am Heart J 1997; 133: 184–189.
Corvol P, Jeunemaitre X : Molecular genetics of human hypertension: role of angiotensinogen. Endocr rev 1997; 18: 662–677.
Karjalainen J, Kujala UM, Stolt A et al: Angiotensinogen gene M235T polymorphism predicts left ventricular hypertrophy in endurance athletes. J Am Coll Cardiol 1999; 34: 494–499.
Danser AHJ, Derkx FHM, Hense HW, Jeunemaitre X, Riegger GAJ, Schunkert H : Angiotensinogen (M235T) and angiotensin-converting enzyme (I/D) polymorphims in association with plasma renin and prorenin levels. J Hypertension 1998; 16: 1879–1883.
Danser AHJ, MADH Schaalekamp, Bax WA et al: Angiotensin-converting enzyme in the human heart: effect of the deletion/insertion polymorphism. Circulation 1995; 92: 1387–1388.
Wang JG, Staessen JA : Genetic polymorphisms in the renin-angiotensin system: relevance for susceptibility to cardiovascular disease. Eur J Pharmacol 2000; 410: 289–302.
Maron BJ, Casey SA, Hurrell DG, Aeppli DM : Relation of left ventricular thickness to age and gender in hypertrophic cardiomyopathy. Am J Cardiol 2003; 91: 1195–1198.
Maron BJ : Hypertrophic cardiomyopathy: a systematic review. JAMA 2002; 287: 1308–1320.
Spirito P, Bellone P, Harris KM, Bernabo P, Bruzzi P, Maron BJ : Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. N Engl J Med 2000; 342: 1778–1785.
Van Driest SL, Ommen SR, Tajik AJ, Gersh BJ, Ackerman MJ : Yield of genetic testing in hypertrophic cardiomyopathy. Mayo Clin Proc 2005; 80: 739–744.
Olivotto I, Maron MS, Selcuk Adabag A et al: Gender-related differences in the clinical presentation and outcome of hypertrophic cardiomyopathy. J Am Coll Cardiol 2005; 45: 480–487.
Marsh JD, Lehmann MH, Ritchie RH, Gwathmey JK, Green GE, Schiebinger RJ : Androgen receptors mediate hypertrophy in cardiac myocytes. Circulation 1998; 98: 256–261.
Xin HB, Senbonmatsu T, Cheng DS et al: Oestrogen protects FKBP12.6 null mice from cardiac hypertrophy. Nature 2002; 416: 334–338.
Lind JM, Chiu C, Ingles J et al: Sex hormone receptor gene variation associated with phenotype in male hypertrophic cardiomyopathy patients. J Mol Cell Cardiol 2008; 45: 217–222.
Brugts JJ, Isaacs A, de Maat MP et al: A pharmacogenetic analysis of determinants of hypertension and blood pressure response to angiotensin-converting enzyme inhibitor therapy in patients with vascular disease and healthy individuals. J Hypertens 2011; 29: 509–519.
Yamazaki T, Suzuki J, Shimamoto R, Tsuji T, Ohmoto K, Nagai R : A new therapeutic strategy for hypertrophic nonobstructive cardiomyopathy in humans. A randomized and prospective study with an Angiotensin II receptor blocker. Int Heart J 2007; 48: 715–724.
Penicka M, Gregor P, Kerekes R, Marek D, Curila K, Krupicka J : The effects of candesartan on left ventricular hypertrophy and function in nonobstructive hypertrophic cardiomyopathy: a pilot, randomized study. J Mol Diagn 2009; 11: 35–41.
Acknowledgements
This study was financially supported by ZorgOnderzoek Nederland (ZonMw, grant 62000010) and the Netherlands Heart Foundation (NHS, grants 2003D302 and NHS/2003T302). The funding organizations have had no involvement in study design, collection, analysis, and interpretation of data, in the writing of this paper and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Kolder, I., Michels, M., Christiaans, I. et al. The role of renin–angiotensin–aldosterone system polymorphisms in phenotypic expression of MYBPC3-related hypertrophic cardiomyopathy. Eur J Hum Genet 20, 1071–1077 (2012). https://doi.org/10.1038/ejhg.2012.48
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2012.48