Abstract
Background/Objectives:
Childhood obesity is a major health problem with serious long-term metabolic consequences. CD36 is important for the development of obesity-related complications among adults. We aimed to investigate circulating sCD36 during weight loss in childhood obesity and its associations with insulin resistance, dyslipidemia, hepatic fat accumulation and low-grade inflammation.
Subjects/Methods:
The impact of a 10-week weight loss camp for obese children (N=113) on plasma sCD36 and further after a 12-month follow-up (N=68) was investigated. Clinical and biochemical data were collected, and sCD36 was measured by an in-house assay. Liver fat was estimated by ultrasonography and insulin resistance by the homeostasis model assessment (HOMA-IR).
Results:
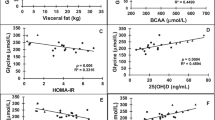
Along with marked weight loss, sCD36 was reduced by 21% (P=0.0013) following lifestyle intervention, and individual sCD36 reductions were significantly associated with the corresponding decreases in HOMA-IR, triglycerides and total cholesterol. The largest sCD36 decrease occurred among children who reduced HOMA-IR and liver fat. After 12 months of follow-up, sCD36 was increased (P=0.014) and the metabolic improvements were largely lost.
Conclusions:
Weight-loss-induced sCD36 reduction, coincident with improved insulin resistance, circulating lipids and hepatic fat accumulation, proposes that sCD36 may be an early marker of long-term health risk associated with obesity-related complications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Berghofer A, Pischon T, Reinhold T, Apovian CM, Sharma AM, Willich SN . Obesity prevalence from a European perspective: a systematic review. BMC Public Health 2008; 8: 200.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894: 1–253.
Han JC, Lawlor DA, Kimm SY . Childhood obesity. Lancet 2010; 375: 1737–1748.
Nader PR, O'Brien M, Houts R, Bradley R, Belsky J, Crosnoe R et al. Identifying risk for obesity in early childhood. Pediatrics 2006; 118: e594–e601.
Capurso C, Capurso A . From excess adiposity to insulin resistance: the role of free fatty acids. Vascul Pharmacol 2012; 57: 91–97.
Hotamisligil GS, Shargill NS, Spiegelman BM . Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 1993; 259: 87–91.
Shoelson SE, Lee J, Goldfine AB . Inflammation and insulin resistance. J Clin Invest 2006; 116: 1793–1801.
Wood IS, de Heredia FP, Wang B, Trayhurn P . Cellular hypoxia and adipose tissue dysfunction in obesity. Proc Nutr Soc 2009; 68: 370–377.
Love-Gregory L, Abumrad NA . CD36 genetics and the metabolic complications of obesity. Curr Opin Clin Nutr Metab Care 2011; 14: 527–534.
Su X, Abumrad NA . Cellular fatty acid uptake: a pathway under construction. Trends Endocrinol Metab 2009; 20: 72–77.
Febbraio M, Hajjar DP, Silverstein RL . CD36: a class B scavenger receptor involved in angiogenesis, atherosclerosis, inflammation, and lipid metabolism. J Clin Invest 2001; 108: 785–791.
Zhou D, Samovski D, Okunade AL, Stahl PD, Abumrad NA, Su X . CD36 level and trafficking are determinants of lipolysis in adipocytes. FASEB J 2012; 26: 4733–4742.
Bastie CC, Hajri T, Drover VA, Grimaldi PA, Abumrad NA . CD36 in myocytes channels fatty acids to a lipase-accessible triglyceride pool that is related to cell lipid and insulin responsiveness. Diabetes 2004; 53: 2209–2216.
Koonen DP, Jacobs RL, Febbraio M, Young ME, Soltys CL, Ong H et al. Increased hepatic CD36 expression contributes to dyslipidemia associated with diet-induced obesity. Diabetes 2007; 56: 2863–2871.
Chabowski A, Zendzian-Piotrowska M, Konstantynowicz K, Pankiewicz W, Mikłosz A, Łukaszuk B et al. Fatty acid transporters involved in the palmitate and oleate induced insulin resistance in primary rat hepatocytes. Acta Physiol (Oxf) 2013; 207: 346–357.
Cai L, Wang Z, Ji A, Meyer JM, van der Westhuyzen DR . Scavenger receptor CD36 expression contributes to adipose tissue inflammation and cell death in diet-induced obesity. PLoS One 2012; 7: e36785.
Handberg A, Levin K, Hojlund K, Beck-Nielsen H . Identification of the oxidized low-density lipoprotein scavenger receptor CD36 in plasma: a novel marker of insulin resistance. Circulation 2006; 114: 1169–1176.
Koonen DP, Jensen MK, Handberg A . Soluble CD36- a marker of the (pathophysiological) role of CD36 in the metabolic syndrome? Arch Physiol Biochem 2011; 117: 57–63.
Handberg A, Hojlund K, Gastaldelli A, Flyvbjerg A, Dekker JM, Petrie J et al. Plasma sCD36 is associated with markers of atherosclerosis, insulin resistance and fatty liver in a nondiabetic healthy population. J Intern Med 2012; 271: 294–304.
Petta S, Handberg A, Marchesini G, Cammà C, Di Marco V, Cabibi D et al. High sCD36 plasma level is associated with steatosis and its severity in patients with genotype 1 chronic hepatitis C. J Viral Hepat 2013; 20: 174–182.
Handberg A, Lopez-Bermejo A, Bassols J, Vendrell J, Ricart W, Fernandez-Real JM . Circulating soluble CD36 is associated with glucose metabolism and interleukin-6 in glucose-intolerant men. Diab Vasc Dis Res 2009; 6: 15–20.
Glintborg D, Hojlund K, Andersen M, Henriksen JE, Beck-Nielsen H, Handberg A . Soluble CD36 and risk markers of insulin resistance and atherosclerosis are elevated in polycystic ovary syndrome and significantly reduced during pioglitazone treatment. Diabetes Care 2008; 31: 328–334.
Knosgaard L, Thomsen SB, Stockel M, Vestergaard H, Handberg A . Circulating sCD36 is associated with unhealthy fat distribution and elevated circulating triglycerides in morbidly obese individuals. Nutr Diabetes 2014; 4: e114.
Handberg A, Skjelland M, Michelsen AE, Sagen EL, Krohg-Sørensen K, Russell D et al. Soluble CD36 in plasma is increased in patients with symptomatic atherosclerotic carotid plaques and is related to plaque instability. Stroke 2008; 39: 3092–3095.
Coker RH, Williams RH, Yeo SE, Kortebein PM, Bodenner DL, Kern PA et al. The impact of exercise training compared to caloric restriction on hepatic and peripheral insulin resistance in obesity. J Clin Endocrinol Metab 2009; 94: 4258–4266.
O'Gorman DJ, Krook A . Exercise and the treatment of diabetes and obesity. Endocrinol Metab Clin North Am 2008; 37: 887–903.
Vitola BE, Deivanayagam S, Stein RI, Mohammed BS, Magkos F, Kirk EP et al. Weight loss reduces liver fat and improves hepatic and skeletal muscle insulin sensitivity in obese adolescents. Obesity (Silver Spring) 2009; 17: 1744–1748.
Birkebaek NH, Lange A, Holland-Fischer P, Kristensen K, Rittig S, Vilstrup H et al. Effect of weight reduction on insulin sensitivity, sex hormone-binding globulin, sex hormones and gonadotrophins in obese children. Eur J Endocrinol 2010; 163: 895–900.
Gronbaek H, Lange A, Birkebaek NH, Holland-Fischer P, Solvig J, Hørlyck A et al. Effect of a 10-week weight loss camp on fatty liver disease and insulin sensitivity in obese Danish children. J Pediatr Gastroenterol Nutr 2012; 54: 223–228.
Kazankov K, Moller HJ, Lange A, Birkebaek NH, Holland-Fischer P, Solvig J et al. The macrophage activation marker sCD163 is associated with changes in NAFLD and metabolic profile during lifestyle intervention in obese children. Pediatr Obes 2014; 10: 226–233.
Kuk JL, Ardern CI . Are metabolically normal but obese individuals at lower risk for all-cause mortality? Diabetes Care 2009; 32: 2297–2299.
Keskin M, Kurtoglu S, Kendirci M, Atabek ME, Yazici C . Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics 2005; 115: e500–e503.
Kurtoglu S, Hatipoglu N, Mazicioglu M, Kendirici M, Keskin M, Kondolot M . Insulin resistance in obese children and adolescents: HOMA-IR cut-off levels in the prepubertal and pubertal periods. J Clin Res Pediatr Endocrinol 2010; 2: 100–106.
Sahin NM, Kinik ST, Tekindal MA . OGTT results in obese adolescents with normal HOMA-IR values. J Pediatr Endocrinol Metab 2013; 26: 285–291.
Reinehr T, Andler W . Changes in the atherogenic risk factor profile according to degree of weight loss. Arch Dis Child 2004; 89: 419–422.
Liani R, Halvorsen B, Sestili S, Handberg A, Santilli F, Vazzana N et al. Plasma levels of soluble CD36, platelet activation, inflammation, and oxidative stress are increased in type 2 diabetic patients. Free Radic Biol Med 2012; 52: 1318–1324.
Chmielewski M, Bragfors-Helin AC, Stenvinkel P, Lindholm B, Anderstam B . Serum soluble CD36, assessed by a novel monoclonal antibody-based sandwich ELISA, predicts cardiovascular mortality in dialysis patients. Clin Chim Acta 2010; 411: 2079–2082.
Miquilena-Colina ME, Lima-Cabello E, Sanchez-Campos S, García-Mediavilla MV, Fernández-Bermejo M, Lozano-Rodríguez T et al. Hepatic fatty acid translocase CD36 upregulation is associated with insulin resistance, hyperinsulinaemia and increased steatosis in non-alcoholic steatohepatitis and chronic hepatitis C. Gut 2011; 60: 1394–1402.
Efrat M, Tepper S, Birk RZ . From fat cell biology to public health preventive strategies - pinpointing the critical period for obesity prevention. J Pediatr Endocrinol Metab 2013; 26: 197–209.
Ye J . Emerging role of adipose tissue hypoxia in obesity and insulin resistance. Int J Obes (Lond) 2009; 33: 54–66.
Acknowledgements
We thank Jane Hansen, Aarhus University Hospital, Skejby, Denmark, for the collection and processing of blood samples; Lone Larsen, Clinical Institute, Aarhus University Hospital, Denmark, for skillful laboratory assistance; Morten H Nielsen, Department of Clinical Biochemistry, Aalborg University Hospital, for assistance in preparation of figures, as well as the staff of Julemærkehjemmet, Hobro, Denmark, for their collaboration during the study. The NOVO Nordisk Foundation supported the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
A Handberg is the inventor of two patent applications on sCD36 as a biomarker of the metabolic syndrome. The Ideas Clinic of Aalborg University Hospital owns the patent IP rights.
Rights and permissions
About this article
Cite this article
Knøsgaard, L., Kazankov, K., Birkebæk, N. et al. Reduced sCD36 following weight loss corresponds to improved insulin sensitivity, dyslipidemia and liver fat in obese children. Eur J Clin Nutr 70, 1073–1077 (2016). https://doi.org/10.1038/ejcn.2016.88
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.88