Abstract
Background/objectives:
Caregiving can be a stressful task with severe consequences on caregivers’ health. Our aim was to evaluate the profile and the burden of caregivers of patients with home artificial nutrition (HAN) in our area.
Subjects/methods:
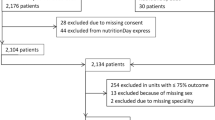
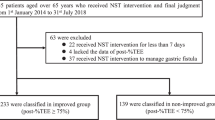
We conducted a prospective observational study of patients who had started HAN over a period of a year (n=573) and their home caregivers (n=103). Epidemiological characteristics of the patients and the type of HAN were registered. Caregivers’ profile data (gender, age and degree of kinship) and Zarit Burden Assessments were recorded.
Results:
Care recipients had a median age of 79.0 (IQR 87) years, neurological and oncological diseases in 50% and a high rate of mobility limitations (80%). Oral supplements with high-calorie formulas were predominant (60%). The usual caregiver profile was a patient’s daughter with a mean age of 53.1 (s.d. 13.4) years acting as the primary caregiver. Burden was absent in 49.5%, light in 18.4% and intense in 32% of caregivers. Intense burden was more frequent in oral over enteral nutrition (42% versus 22.6%; P=0.036). Supplementary nutrition was also associated with higher caregiver burden scores compared with complete diets. In patients with functional limitations, a tendency toward a slightly higher burden was observed. No differences in caregiver burden were detected according to other patient or caregiver characteristics.
Conclusions:
HAN type appears to be a factor influencing caregiver burden and therefore, evaluation of caregiver burden should be part of HAN programs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Mc Whirter JP, Pennington CR . Incidence and recognition of malnutrition in hospital. BMJ 1994; 308: 945–948.
Thorsdottir I, Eriksen B, Eysteinsdottir S . Nutritional status at submission for dietetic services and screening for malnutrition at admission to hospital. Clin Nutr 1999; 18: 15–21.
Aznarte Padial P, Pareja Rodríguez de Vera A, de la Rubia Nieto A, López Soriano F, Martínez de Guzmán M . Impact of hospitalization on patients with nutrition status evaluation at admission. Nutr Hosp 2001; 16: 14–18.
Martínez Olmos MA, Martínez Vázquez MJ, Martínez-Puga López E, del Campo Pérez V . Collaborative group for the study of hospital malnutrition in Galicia (Spain). Eur J Clin Nutr 2005; 59: 938–946.
Milà Villarroel R, Formiga F, Duran Alert P, Abellana Sangrà R . Prevalence of malnutrition in Spanish elders: systematic review. Med Clin (Barc) 2012; 139: 502–508.
Parsons EL, Stratton RJ, Cawood AL, Smith TR, Elia M . Oral nutritional supplements in a randomised trial are more effective than dietary advice at improving quality of life in malnourished care home residents. Clin Nutr 2016, e-pub ahead of print 11 January 2016 doi:10.1016/j.clnu.2016.01.002.
Atención a las personas en situación de dependencia en España Libro blanco. IMSERSO. 2005. (Accessed 24 February 2016, available at http://www.dependencia.imserso.es/InterPresent2/groups/imserso/documents/binario/libroblanco.pdf).
Girgis A, Lambert S, Johnson C, Waller A, Currow D . Physical, psychosocial, relationship, and economic burden of caring for people with cancer: a review. J Oncol Pract 2013; 9: 197–202.
Zarit SH, Reever KE, Bach-Peterson J . Relatives of the impaired elderly: Correlates of feeling of burden. Gerontologist 1980; 20: 649–655.
González F, Graz A, Pitiot D, Podestá J . Sobrecarga del cuidador de personas con lesiones neurológicas. Revista del Hospital J. M. Ramos Mejía 2004; 9: 1–22. (Accessed 24 February 2016, available at http://hospitalramosmejia.info/r/200404/7.pdf).
Seira MP, Aller A, Calvo A . morbilidad sentida y diagnosticada en cuidadores de pacientes inmovilizados de una zona rural. Rev Esp Salud Pública 2002; 76: 713–721.
Crespo M, López J . Los costes de cuidar: análisis del estado emocional de cuidadores informales de ancianos dependientes. JANO 2004; 1511: 78–79.
Badia X, Lara N, Roset M . Calidad de vida, tiempo de dedicación y carga percibida por el cuidador informal del enfermo de Alzheimer. Aten Primaria 2004; 34: 170–177.
Schulz R, Beach SR . Caregiving as a risk factor for mortality: the caregiver health effects study. JAMA 1999; 282: 2215–2219.
Álvarez J, Del Río J, Planas M, García Peris P, García de Lorenzo, Calvo V et al. Documento SENPE-SEDOM sobre la codificación de la desnutrición hospitalaria. Nutr Hosp 2008; 23: 536–540.
Álvarez L, González AM, Muñoz P . El cuestionario de sobrecarga del cuidador de Zarit. Cómo administrarlo e interpretarlo. Gac Sanit 2008; 22: 618–619.
Martín M, Salvadó I, Nadal S, Miji LC, Rico JM, Lanz P . Adaptación para nuestro medio de la Escala de Sobrecarga del Cuidador (Caregiver Burden Interview) de Zarit. Rev Gerontol 1996; 6: 338–346.
Wanden-Berghe C, Puiggrós JC, Calañas A, Cuerda C, García-Luna PP, Rabassa-Soler A et al. Registro español de nutrición enteral domiciliaria del año 2009; Grupo NADYA-SENPE. Nutr Hosp 2010; 25: 959–963.
Frías L, Puiggrós C, Calañas A, Cuerda C, García-Luna PP, Camarero E et al. Nutrición enteral domiciliaria en España: registro NADYA del año 2010. Nutr Hosp 2012; 27: 266–269.
Wanden-Berghe C, Álvarez Hernández J, Burgos Peláez R, Cuerda Compes C, Matía Martín P, Luengo Pérez LM et al. A home enteral nutrition (HEN); spanish registry of NADYA-SENPE group; for the year 2013. Nutr Hosp 2015; 31: 2518–2522.
Hebuterne X, Bozzetti F, Moreno Villares JM, Pertkiewicz M, Shaffer J, Staun M et al. Home enteral nutrition in adults: a European multicentre survey. Clin Nutr 2003; 22: 261–266.
National Alliance for Caregiving and the American Association of Retired Person (AARP) Caregiver Profile. The typical caregiver. (Accessed 24 February 2016, availablr at http://www.caregiving.org/wp-content/uploads/2015/05/Caregiving-in-theUS2015_Typical_CGProfile.pdf).
Van Durme T, Macq J, Jeanmart C, Gobert M . Tools for measuring the impact of informal caregiving of the elderly: a literature review. Int J Nurs Stud 2012; 49: 490–504.
Hirono N, Kobayashi H, Mori E . Caregiver burden in dementia: evaluation with a japanese version of the Zarit caregiver burden interview. No To Shinkei 1998; 50: 561–567.
Do Muíño Joga M, Fernández Fernández MV, Rodríguez Rodríguez E, González Rodríguez C, Iglesias Cerqueiro RM . Sobrecarga del cuidador principal de pacientes inmovilizados en atención primaria. Cad Aten Primaria 2010; 17: 10–14.
Santiago Navarro P, López Mederos O, Lorenzo Riera A . Morbidity in the caregivers of patients confined to their homes. Aten Primaria 1999; 24: 404–410.
Campbell P, Wright J, Oyebode J, Job D, Crome P, Bentham P et al. Determinants of burden in those who care for someone with dementia. Int J Geriatr Psychiatry 2008; 23: 1078–1085.
Gort AM, Mingot M, Gomez X, Soler T, Torres G, Sacristán O et al. Use of the Zarit scale for assessing caregiver burden and collapse in caregiving at home in dementias. Int J Geriatr Psychiatry 2007; 22: 957–962.
Silver HJ, Wellman NS, Galindo-Ciocon D, Johnson P . Family caregivers of older adults on home enteral nutrition have multiple unmet task-related training needs and low overall preparedness for caregiving. J Am Diet Assoc 2004; 104: 43–50.
Bjuresäter K, Larsson M, Athlin E . Struggling in an inescapable life situation: being a close relative of a person dependent on home enteral tube feeding. J Clin Nurs 2012; 21: 1051–1059.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Villar-Taibo, R., Martínez-Olmos, M., Bellido-Guerrero, D. et al. Burden assessment in caregivers of patients with home artificial nutrition: a need and a challenge. Eur J Clin Nutr 71, 192–197 (2017). https://doi.org/10.1038/ejcn.2016.239
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.239
This article is cited by
-
Value co-creation with family caregivers to people with dementia through a tailor-made mHealth application: a qualitative study
BMC Health Services Research (2022)
-
Evidence on nutritional therapy practice guidelines and implementation in adult critically ill patients: a scoping review protocol
Systematic Reviews (2019)