Abstract
Background/Objectives:
Children with Crohn’s disease often demonstrate nutritional recovery during primary therapy at diagnosis, but long-term nutritional support is sometimes necessary. Evidence to inform best nutritional practice including energy and micronutrient requirements is limited. The principal objective of this study was to determine how energy expenditure and physical activity vary with disease activity over the first year following diagnosis.
Subjects/Methods:
Twenty children were studied at diagnosis with Crohn’s disease and were followed up over 1 year while receiving treatment according to national guidelines. The majority of children (13) were treated with exclusive enteral nutrition. At study visits, height, weight, bioelectrical impedance, resting energy expenditure by indirect calorimetry, tri-axial accelerometer and blood investigations were performed alongside clinical assessment.
Results:
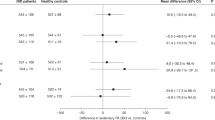
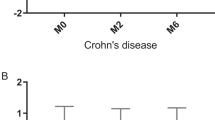
There was no significant effect of disease activity on resting energy expenditure (REE). Physical activity was greater after primary therapy (Z=3.31, P<0.01). Median wPCDAI fell from 58 at diagnosis to 7.5 after primary therapy and was 7.5 at 1 year. Weight s.d.s increased from −1.67 to −0.86 and lean index s.d.s increased from −2.93 to −1.64, although the increase was mostly in the first 2 months. Median height s.d.s was unchanged throughout this study. There was a significant association between dietary intake and weight gain (r=0.8 P<0.01) but not height gain. Persistent micronutrient deficits beyond diagnosis were seen for both iron and vitamin D.
Conclusions:
This study has demonstrated that REE does not change significantly through different phases of disease activity, but physical activity is low at diagnosis. Children with Crohn's disease should be screened for deficiencies of iron and vitamin D.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kelsen J, Baldassano RN . Inflammatory bowel disease: the difference between children and adults. Inflamm Bowel Dis 2008; 14 (Suppl 2), S9–S11.
Vasseur F, Gower-Rousseau C, Vernier-Massouille G, Dupas JL, Merle V, Merlin B et al. Nutritional status and growth in pediatric Crohn's disease: a population-based study. Am J Gastroenterol 2010; 105: 1893–1900.
Sylvester FA, Leopold S, Lincoln M, Hyams JS, Griffiths AM, Lerer T . A two-year longitudinal study of persistent lean tissue deficits in children with Crohn's disease. Clin Gastroenterol Hepatol 2009; 7: 452–455.
Pichard C, Kyle UG, Morabia A, Perrier A, Vermeulen B, Unger P . Nutritional assessment: lean body mass depletion at hospital admission is associated with an increased length of stay. Am J Clin Nutr 2004; 79: 613–618.
Hartman C, Eliakim R, Shamir R . Nutritional status and nutritional therapy in inflammatory bowel diseases. World J Gastroenterol 2009; 15: 2570–2578.
Wiskin AE, Wootton SA, Cornelius VR, Afzal NA, Elia M, Beattie RM . No relation between disease activity measured by multiple methods and REE in childhood Crohn disease. J Pediatr Gastroenterol Nutr 2012; 54: 271–276.
Gerasimidis K, Talwar D, Duncan A, Moyes P, Buchanan E, Hassan K et al. Impact of exclusive enteral nutrition on body composition and circulating micronutrients in plasma and erythrocytes of children with active Crohn's disease. Inflamm Bowel Dis 2012; 18: 1672–1681.
Bousvaros A, Zurakowski D, Duggan C, Law T, Rifai N, Goldberg NE et al. Vitamins A and E serum levels in children and young adults with inflammatory bowel disease: effect of disease activity. J Pediatr Gastroenterol Nutr 1998; 26: 129–135.
Filippi J, Al-Jaouni R, Wiroth JB, Hebuterne X, Schneider SM . Nutritional deficiencies in patients with Crohn's disease in remission. Inflamm Bowel Dis 2006; 12: 185–191.
IBD Working Group of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. Inflammatory bowel disease in children and adolescents: recommendations for diagnosis—the Porto criteria. J Pediatr Gastroenterol Nutr 2005; 41: 1–7.
DoH Dietary Reference Values for Food Energy and Nutrients for the United Kingdom. 13 ed. TSO: Norwich, 2004.
Sandhu BK, Fell JME, Beattie RM, Mitton SG, On Behalf of the IBD Working Group of the British Society of Paediatric Gastroenterology Hepatology and Nutrition. Guidelines for the Management of Inflammatory Bowel Disease in Children in the United Kingdom. 2008.
Turner D, Griffiths AM, Walters TD, Seah T, Markowitz J, Pfefferkorn M et al. Appraisal of the pediatric Crohn's disease activity index on four prospectively collected datasets: recommended cutoff values and clinimetric properties. Am J Gastroenterol 2010; 105: 2085–2092.
Freeman JV, Cole TJ, Chinn S, Jones PR, White EM, Preece MA . Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child 1995; 73: 17–24.
Sherriff A, Wright CM, Reilly JJ, McColl J, Ness A, Emmett P . Age- and sex-standardised lean and fat indices derived from bioelectrical impedance analysis for ages 7-11 years: functional associations with cardio-respiratory fitness and grip strength. Br J Nutr 2009; 101: 1753–1760.
Weir JB . New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 1949; 109: 1–9.
Schofield WN . Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 1985; 39 (Suppl 1), 5–41.
WHO, Iron Deficiency Anaemia Assessment, Prevention and Control: A guide for programme managers: WHO, 2001.
Gasche C, Berstad A, Befrits R, Beglinger C, Dignass A, Erichsen K et al. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm Bowel Dis 2007; 13: 1545–1553.
Levine A, Griffiths A, Markowitz J, Wilson DC, Turner D, Russell RK et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis 2011; 17: 1314–1321.
Azcue M, Rashid M, Griffiths A, Pencharz PB . Energy expenditure and body composition in children with Crohn's disease: effect of enteral nutrition and treatment with prednisolone. Gut 1997; 41: 203–208.
Zoli G, Katelaris PH, Garrow J, Gasbarrini G, Farthing MJ . Increased energy expenditure in growing adolescents with Crohn's disease. Dig Dis Sci 1996; 41: 1754–1759.
Steiner SJ, Pfefferkorn MD, Fitzgerald JF, Denne SC . Protein and energy metabolism response to the initial dose of infliximab in children with Crohn's disease. Inflamm Bowel Dis 2007; 13: 737–744.
Steiner SJ, Pfefferkorn MD, Fitzgerald JF, Denne SC . Carbohydrate and lipid metabolism following infliximab therapy in pediatric Crohn's disease. Pediatr Res 2008; 64: 673–676.
Burnham JM, Shults J, Semeao E, Foster BJ, Zemel BS, Stallings VA et al. Body-composition alterations consistent with cachexia in children and young adults with Crohn disease. Am J Clin Nutr 2005; 82: 413–420.
Thayu M, Denson LA, Shults J, Zemel BS, Burnham JM, Baldassano RN et al. Determinants of changes in linear growth and body composition in incident pediatric Crohn's disease. Gastroenterology 2010; 139: 430–438.
Acknowledgements
Thanks to Christine Glenn and Kesta Durkin within the Southampton Centre for Biomedical Research for their help in laboratory and anthropometric measurements. This study was funded by the NIHR Biomedical Research Unit, Nutrition, Diet & Lifestyle in Southampton. AEW was supported by a fellowship from Crohn’s in Childhood Research Association.
Author contributions
AEW, SAW and RMB conceived of the study, conducted analysis and wrote the final manuscript; AEW and RH collected data; and NAA and AB assisted with data collection and final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wiskin, A., Haggarty, R., Afzal, N. et al. Nutritional perspectives of children with Crohn’s disease: a single-centre cohort observation of disease activity, energy expenditure and dietary intake. Eur J Clin Nutr 70, 1132–1137 (2016). https://doi.org/10.1038/ejcn.2016.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.107