Abstract
Background/Objectives:
A healthy diet is an integral component of successful diabetes management. However, the comparative importance of adopting a healthy diet for cardiovascular risk factor reduction over and above medication use among newly diagnosed diabetes patients remains unclear.
Subjects/Methods:
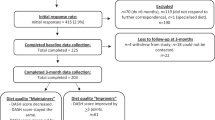
We computed a dietary score consistent with American Diabetes Association and Diabetes UK recommendations in 574 newly diagnosed diabetes patients by summing standardised values for the intake of total energy, saturated fat, sodium, fibre and plasma vitamin C. In linear regression analyses, stratified by cardio-protective medication use (yes/no), we quantified the comparative longitudinal associations of baseline diet and change in diet over 1 year with change in blood pressure, HbA1c and lipids.
Results:
Baseline diet was generally not predictive of change in cardiovascular risk factor levels at 1 year. In contrast, dietary change over 1 year among patients prescribed and not prescribed cardio-protective medication after baseline was associated with comparative (p-interaction all ⩾0.95) reductions in diastolic blood pressure (−2.38 vs −2.93 mm Hg, respectively) and triglycerides (−0.31 vs −0.21 mmol/l, respectively), independent of potential confounding factors and change from baseline to follow-up in physical activity and smoking status.
Conclusions:
Modest dietary change over the first year following diagnosis of diabetes was associated with reductions in blood pressure and triglycerides, over and above the effects of cardio-protective medication. Our findings support the notion that dietary change should be viewed as an integral component of successful diabetes self-management, irrespective of medication use.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care 2011; 34: S11–S61.
Manley SE, Stratton IM, Cull CA, Frighi V, Eeley EA, Matthews DR et al. UK Prospective Diabetes Study Group. Effects of three months' diet after diagnosis of Type 2 diabetes on plasma lipids and lipoproteins (UKPDS 45). Diabet Med 2000; 17: 518–523.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001; 344: 3–10.
American Diabetes Association. Standards of medical care in diabetes–2013. Diabetes Care 2013; 36: S11–S66.
Cerkoney KA, Hart LK . The relationship between the health belief model and compliance of persons with diabetes mellitus. Diabetes Care. 1980; 3: 594–598.
Rubin RR Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med 2005; 118((Suppl 5A)): 27S–34S.
Jin J, Sklar GE, Min Sen Oh V, Chuen LiS Factors affecting therapeutic compliance: a review from the patient's perspective. Ther Clin Risk Manag 2008; 4: 269–286.
Broadbent E, Donkin L, Stroh JC Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care 2011; 34: 338–340.
Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ 2007; 334: 299.
Diabetes UK Evidence-based nutrition guidelines for the prevention and management of diabetes. Diabetes UK 2011 [cited 2012 10th July]; available from http://www.diabetes.org.uk/Documents/Reports/Nutritional_guidelines200911.pdf.
Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2013; 36: 3821–3842.
Echouffo-Tcheugui JB, Simmons RK, Williams KM, Barling RS, Prevost AT, Kinmonth AL et al. The ADDITION-Cambridge trial protocol: a cluster — randomised controlled trial of screening for type 2 diabetes and intensive treatment for screen-detected patients. BMC Public Health 2009; 9: 136.
Griffin SJ, Little PS, Hales CN, Kinmonth AL, Wareham NJ Diabetes risk score: towards earlier detection of type 2 diabetes in general practice. Diabetes Metab Res Rev 2000; 16: 164–171.
Alberti KG, Zimmet PZ Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Med 1998; 15: 539–553.
McIntosh A, Hutchinson A, Home PD, Brown F, Bruce A, Damerell A et al. Clinical Guidelines and Evidence for Type 2 Diabetes: Management of Blood Pressure. School of Health and Related Research (ScHARR): Sheffield, 2002.
McIntosh A, Hutchinson A, Home PD, Brown F, Bruce A, Damerell A et al. Clinical Guidelines and Evidence for Type 2 Diabetes: Lipids Management. School of Health and Related Research (ScHAAR): Sheffield, 2002.
McIntosh A, Hutchinson A, Home PD, Brown F, Bruce A, Damerell A et al. Clinical Guidelines and Evidence Review for Type 2 Diabetes: Management of Blood Glucose. School of Health and Related Research (ScHAAR): Sheffield, 2001.
Griffin SJ, Borch-Johnsen K, Davies MJ, Khunti K, Rutten GE, Sandbaek A et al. Effect of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with type 2 diabetes detected by screening (ADDITION-Europe): a cluster-randomised trial. Lancet 2011; 378: 156–167.
Wareham NJ, Jakes RW, Rennie KL, Mitchell J, Hennings S, Day NE Validity and repeatability of the EPIC-Norfolk Physical Activity Questionnaire. Int J Epidemiol 2002; 31: 168–174.
Bingham SA, Gill C, Welch A, Cassidy A, Runswick SA, Oakes S et al. Validation of dietary assessment methods in the UK arm of EPIC using weighed records, and 24-hour urinary nitrogen and potassium and serum vitamin C and carotenoids as biomarkers. Int J Epidemiol 1997; 26: S137–S151.
Welch AA, Luben R, Khaw KT, Bingham SA The CAFE computer program for nutritional analysis of the EPIC-Norfolk food frequency questionnaire and identification of extreme nutrient values. J Hum Nutr Diet 2005; 18: 99–116.
Hu FB . Obesity Epidemiology. Oxford University Press Inc.: New York, 2008.
Michels KB, Welch AA, Luben R, Bingham SA, Day NE Measurement of fruit and vegetable consumption with diet questionnaires and implications for analyses and interpretation. Am J Epidemiol 2005; 161: 987–994.
Kristal AR, Beresford SA, Lazovich D Assessing change in diet-intervention research. Am J Clin Nutr 1994; 59: 185S–189SS.
Altman DG, Royston P . The cost of dichotomising continuous variables. BMJ 2006; 332: 1080.
Block G, Norkus E, Hudes M, Mandel S, Helzlsouer K Which plasma antioxidants are most related to fruit and vegetable consumption? Am J Epidemiol 2001; 154: 1113–1118.
Andrews RC, Cooper AR, Montgomery AA, Norcross AJ, Peters TJ, Sharp DJ et al. Diet or diet plus physical activity versus usual care in patients with newly diagnosed type 2 diabetes: the Early ACTID randomised controlled trial. Lancet 2011; 378: 129–139.
Coppell KJ, Kataoka M, Williams SM, Chisholm AW, Vorgers SM, Mann JI Nutritional intervention in patients with type 2 diabetes who are hyperglycaemic despite optimised drug treatment–Lifestyle Over and Above Drugs in Diabetes (LOADD) study: randomised controlled trial. BMJ 2010; 341: c3337.
Barnard RJ, Jung T, Inkeles SB . Diet and exercise in the treatment of NIDDM. The need for early emphasis. Diabetes Care 1994; 17: 1469–1472.
Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000; 321: 412–419.
Acknowledgements
ADDITION-Cambridge was supported by the Wellcome Trust (grant reference no.: G061895), the Medical Research Council (grant reference no.: G0001164), the NIHR Health Technology Assessment Programme (grant reference no.: 08/116/300), National Health Service R&D support funding (including the Primary Care Research and Diabetes Research Networks) and the National Institute for Health Research. SJG receives support from the Department of Health NIHR Programme Grant funding scheme [RP-PG-0606-1259]. The views expressed in this publication are those of the authors and not necessarily those of the UK Department of Health. Bio-Rad provided equipment for HbA1c testing during the screening phase. We are grateful to the ADDITION-Cambridge independent trial steering committee (Nigel Stott (Chair), John Weinman, Richard Himsworth and Paul Little). Aside from the authors, the ADDITION-Cambridge study team has included Rebecca Abbott, Amanda Adler, Judith Argles, Gisela Baker, Rebecca Bale, Roslyn Barling, Daniel Barnes, Mark Betts, Sue Boase, Clare Boothby, Sandra Bovan, Ryan Butler, Parinya Chamnan, Sean Dinneen, Pesheya Doubleday, Sue Emms, Mark Evans, Tom Fanshawe, Francis Finucane, Philippa Gash, Julie Grant, Wendy Hardeman, Robert Henderson, Susie Hennings, Muriel Hood, Garry King, Ann-Louise Kinmonth, Georgina Lewis, Christine May Hall, Joanna Mitchell, Richard Parker, Nicola Popplewell, A. Toby Prevost, Emanuella De Lucia Rolfe, Lincoln Sargeant, Megan Smith, Stephen Sutton, Nicholas Wareham, Liz White, Fiona Whittle and Kate Williams. We thank the Cambridge University Hospitals NHS Foundation Trust Department of Clinical Biochemistry and the NIHR Cambridge Biomedical Research Centre, Core Biochemical Assay Laboratory for carrying out the biochemical assays, and the following groups within the MRC Epidemiology Unit: data management (Adam Dickinson), information technology (Iain Morrison), technical (Matt Sims) and field epidemiology (Paul Roberts, Kim Mwanza and James Sylvester). ADDITION-Cambridge was supported by the Wellcome Trust (grant reference no.: G061895), the Medical Research Council (grant reference no.: G0001164), the NIHR Health Technology Assessment Programme (grant reference no.: 08/116/300), National Health Service R&D support funding (including the Primary Care Research and Diabetes Research Networks) and the National Institute for Health Research.
AUTHOR CONTRIBUTIONS
AJMC, RKS and SJG conceived and designed the study question. SJG and RKS acquired the data. AJMC analysed the data. AJMC, DS, GHL, SJG and RKS interpreted the data and wrote the paper. AJMC, RKS and SJG had primary responsibility for the final content of the paper. All authors critically revised the paper for important intellectual content and have approved the final version.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cooper, A., Schliemann, D., Long, G. et al. Do improvements in dietary behaviour contribute to cardiovascular risk factor reduction over and above cardio-protective medication in newly diagnosed diabetes patients?. Eur J Clin Nutr 68, 1113–1118 (2014). https://doi.org/10.1038/ejcn.2014.79
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.79