Abstract
Background/Objectives:
Iron in high doses or when given to non-anaemic women may have adverse effects on pregnancy outcomes. This study aimed to estimate the supplemental iron intake in non-anaemic pregnant women attending an urban antenatal care setting in South India and examine the association of supplemental iron intake with birth outcomes.
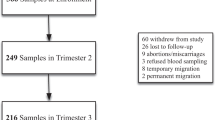
Subjects/Methods:
A cohort of 1196 non-anaemic pregnant women was studied. Daily supplemental iron intake was calculated as total supplemental iron consumed (mg) during pregnancy divided by the total number of days the supplement was recommended. Association of tertiles of supplemental iron intake with term low birth weight (tLBW), preterm delivery and small for gestational age (SGA) was examined using log-binomial regression, adjusting for maternal age, height, body mass index at recruitment, parity, education and type of delivery.
Results:
Mean haemoglobin in trimester 1 was 12.4±0.9 g/dl and mean supplemental iron intake was 37.7±4.0 mg/day. Women in the highest tertile (>39.2 mg/day) of supplemental iron intake had an increased risk of tLBW as compared with the lowest tertile (⩽36.6 mg/day) (adjusted risk ratio: 1.89; 95% confidence interval: 1.26, 2.83). Although supplemental iron intake was negatively correlated with gestational age (r=−0.20, P<0.001) and birth weight (r=−0.07, P=0.011), there was no association between preterm delivery or SGA and supplemental iron intake.
Conclusions:
It appears that iron supplementation in non-anaemic pregnant women may not be beneficial, as we have observed the adverse effects with a prescribed dose of 45 mg/day. This may warrant the consideration of an individualized approach for antenatal iron supplementation, especially in non-anaemic women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization Worldwide prevalence of anaemia 1993-2005: WHO global database on anaemia.. Geneva WHO, 2008, http://www.who.int/vmnis.
Ministry of Health and Family Welfare, Government of India: Guidelines for the control of iron deficiency anaemia: A national iron plus initiative. Ministry of Health and Family Welfare: Adolescent division 2013.
World Health Organization Guideline: Daily iron and folic acid supplementation in pregnant women. WHO Geneva, 2012.
Chang SC, O’Brien KO, Nathanson MS, Mancini J, Witter FR . Haemoglobin concentrations influence birth outcomes in pregnant African-American adolescents. J Nutr 2003; 133: 2348–2355.
Milman N . Oral iron prophylaxis in pregnancy: not too little and not too much!. J Pregnancy 2012; 2012: 514345.
Sharma JB, Jain S, Mallika V, Singh T, Kumar A, Arora R et al. A prospective, partially randomized study of pregnancy outcomes and hematologic responses to oral and intramuscular iron treatment in moderately anaemic pregnant women. Am J Clin Nutr 2004; 79: 116–122.
Chaturvedi S, Ranadive B . Are we really making motherhood safe? A study of provision of iron supplements and emergency obstetric care in rural Maharashtra. Natl Med J India 2007; 20: 294.
Casanueva E, Viteri FE . Iron and oxidative stress in pregnancy. J Nutr 2003; 133: 1700 S–1708 S.
Dresow B, Petersen D, Fischer R, Nielsen P . Non-transferrin-bound iron in plasma following administration of oral iron drugs. Biometals 2008; 21: 273–276.
Bhatla N, Kaul N, Lal N, Kriplani A, Agarwal N, Saxena R et al. Comparison of effect of daily versus weekly iron supplementation during pregnancy on lipid peroxidation. J Obstet Gynaecol Res 2009; 35: 438–445.
Beard JL . Effectiveness and strategies of iron supplementation during pregnancy. Am J Clin Nutr 2000; 71: 1288 s–1294 s.
Ribot B, Aranda N, Giralt M, Romeu M, Balaguer A, Arija V . Effect of different doses of iron supplementation during pregnancy on maternal and infant health. Ann Hematol 2013; 92: 221–229.
Ziaei S, Norrozi M, Faghihzadeh S, Jafarbegloo E . A randomised placebo-controlled trial to determine the effect of iron supplementation on pregnancy outcome in pregnant women with haemoglobin ≥13.2 g/dl. Br J Obstet Gynaecol 2007; 114: 684–688.
Dwarkanath P, Barzilay JR, Thomas T, Thomas A, Bhat S, Kurpad AV . High folate and low vitamin B-12 intakes during pregnancy are associated with small-for-gestational age infants in South Indian women: a prospective observational cohort study. Am J Clin Nutr 2013; 98: 1450–1458.
World Health Organization Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854: 1–452.
Peña-Rosas JP, De-Regil LM, Dowswell T, Viteri FE . Daily oral iron supplementation during pregnancy (review). Cochrane Database Syst Rev 2012; ((12)): CD004736.
Hall JE, Guyton AC . Textbook of medical physiology, 12th edn, Elsevier Saunders Inc.: Philadelphia, USA, 2011.
Brittenham GM, Andersson M, Egli I, Foman JT, Zeder C, Westerman ME et al. Circulating non–transferrin-bound iron after oral administration of supplemental and fortification doses of iron to healthy women: a randomized study. Am J Clin Nutr 2014; 100: 813–820.
Halliwell B, Gutteridge JMC . Oxygen, free radicals and iron in relation to biology and medicine: some problems and concepts. Arch Biochem Biophys 1986; 246: 501–514.
Burton GJ, Jauniaux E . Oxidative stress. Best Pract Res Clin Obstet Gynaecol 2011; 25: 287–299.
Aranda N, Ribot B, Viteri F, Cavalle P, Arija V . Predictors of hemoconcentration at delivery: association with low birth weight. Eur J Nutr 2012; 52: 1631–1639.
Steer P, Alam MA, Wadsworth J, Welch A . Relation between maternal haemoglobin concentration and birth weight in different ethnic groups. BMJ 1995; 310: 489–491.
Acknowledgements
We greatly appreciate the assistance of Nancy Nanditha M in the collection and entry of data. We thank the women and their infants who participated in this study and the doctors and nurses who made this study possible. LS, PEM, PD, TT and AVK took part in conceptualizing the study, analyzing data and writing the manuscript. PD and AT were involved in data collection. CD, RB and CMM were involved in analyzing data and writing the manuscript. AVK stands as guarantor of the study.
Registered at Clinical Trials Registry-India (www.ctri.nic.in) REF/2013/07/005342.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shastri, L., Mishra, P., Dwarkanath, P. et al. Association of oral iron supplementation with birth outcomes in non-anaemic South Indian pregnant women. Eur J Clin Nutr 69, 609–613 (2015). https://doi.org/10.1038/ejcn.2014.248
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.248
This article is cited by
-
The relationship between markers of antenatal iron stores and birth outcomes differs by malaria prevention regimen—a prospective cohort study
BMC Medicine (2021)
-
Iron supplementation during pregnancy – a cross-sectional study undertaken in four German states
BMC Pregnancy and Childbirth (2018)
-
Review of the Plausibility of Iron Deficiency Hypothesis of Autism
Review Journal of Autism and Developmental Disorders (2017)