Abstract
Background/Objectives:
Non-alcoholic fatty liver disease (NAFLD) is considered an integral part of metabolic syndrome (MS). We aimed to explore the inter-relations of MS and dietary composition in subjects with and without hepatic steatosis and to identify the nutritional risk factors contributing to NAFLD.
Subjects/Methods:
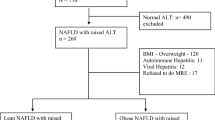
In all 98 subjects with steatosis and 102 controls were selected for the study after screening 260 consecutive healthy individuals. Anthropometric and nutritional information, biochemical data and clinical profile were analyzed. Prevalence of MS was determined based on the consensus statement for diagnosis of MS for Asian Indians. Multiple logistic regression analysis was done to predict the dietary risk factors in NAFLD.
Results:
Prevalence of MS was 44.9% among NAFLD cases and 25.5% among controls (P=0.003). Subjects with NAFLD had significantly higher values of body mass index (BMI), waist circumference (WC), percent body fat, total cholesterol, triglycerides and blood pressure than controls. The total calorie intake, percent of carbohydrate and fat intake of NAFLD cases was significantly higher than controls. Multiple logistic regression analysis showed BMI (odds ratio 6.03 (95% confidence interval 3.26–11.14)), WC (5.49 (2.59–11.57)) and percent dietary fat intake (2.51 (1.99–3.31)) as independent nutritional risk factors in NAFLD.
Conclusions:
In this study, there is a high prevalence of MS among subjects with steatosis and metabolic disorders were closely related to NAFLD. BMI, WC and percent fat intake are independent dietary risk factors in NAFLD. Decreased nutritional intake with restricted fat may constitute an important therapy in subjects with NAFLD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Angulo P (2002). Nonalcoholic fatty liver disease. N Engl J Med 346, 1221–1231.
Arora SK, McFarlane SI (2005). The case for low carbohydrate diets in diabetes management. Nutr Metab 2, 16–24.
Bajaj S, Nigam P, Luthra A, Pandey RM, Kondal D, Bhatt SP et al. (2009). A case-control study on insulin resistance, metabolic co-variants and prediction score in nonalcoholic fatty liver disease. Ind J Med Res 129, 285–292.
Carroll RJ, Freedman LS, Hartman AM (1996). Use of semiquantitative food frequency questionnaires to estimate the distribution of usual intake. Am J Epidemiol 143 (Suppl 4), 392–404.
CDC (1996). Physical Activity and Health: Report of the Surgeon General. US Department of Health and Human Services, CDC: Atlanta, Georgia.
Chitturi S, Farrell GC (2001). Etiopathogenesis of nonalcoholic steatohepatitis. Semin Liver Dis 21, 27–41.
Chitturi S, Farrell GC, Hashimoto E, Saibara T, Lau GKK, Soilano JD (2007). Non-alcoholic fatty liver disease in the Asia-Pacific region: definitions and overview of proposed guidelines. J Gastroenterol Hepatol 22, 778–787.
Clark JM, Brancati FL, Diehl AM (2003). The prevalence and etiology of elevated amionotransferace levels in United States. Am J Gastroenterol 98, 960–967.
Collantes R, Ong JP, Younossi ZM (2004). Nonalcoholic fatty liver disease and the epidemic of obesity. Cleveland Clin J Med 71, 657–663.
Dixon JR, Bathol PS, O’Brien PE (2001). Nonalcoholic fatty liver disease. Predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology 12, 91–100.
Eckel RH, Grundy SM, Zimmet PZ (2005). The metabolic syndrome. Lancet 365, 1415–1428.
Fan JG, Saibara T, Chitturi S, Kim BI, Sung JJ, Chutaputti A (2005). Fatty liver and the metabolic syndrome among Shanghai adults. J Gastroenterol Hepatol 20, 1825–1832.
Farrell GC (2003). Non-alcoholic steatohepatitis: what is it, and why is it important in the Asia-Pacific region? J Gastroenterol Hepatol 18, 124–138.
Farrell GC, Chitturi S, Lau GKK, Sollano J (2007). Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J Gastroenterol Hepatol 22, 775–777.
Farrell GC, Larter CZ (2006). Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology 43, S99–S112.
Fierbinteanu-Braticevici C, Andronescu D, Usvat R, Cretoiu D, Baicus C, Marinoschi G (2009). Acoustic radiation force imaging sonoelastography for noninvasive staging of liver fibrosis. W J Gastroenterol 15 (Suppl 44), 5525–5532.
Ford ES, Gile WH, Dietz WH (2002). Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 287, 356–359.
Gopalan C, Rama Sastri BV, Balasubramanian SC (2004). Nutritive Value of Indian Foods, 1st edn. National Institute of Nutrition; Indian Council of Medical Research, Hyderabad, India. pp 45–95.
Kang H, Greenson JK, Omo JT, Chao C, Peterman D, Anderson L et al. (2006). Metabolic syndrome is associated with greater histologic severity, higher carbohydrate, and lower fat diet in patients with NAFLD. Am J Gastroenterol 101 (Suppl 10), 2247–2253.
Larter CZ, Yeh MM, Van Rooyen DM, Teoh NC, Brooling J, Hou JY et al. (2009). Role of adipose restriction and metabolic factors in pregression of steatosis to steatohepatitis in obese, diabetic mice. J Gastroenterol Hepatol 24, 1658–1668.
Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R et al. (2003). Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 37, 917–923.
Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D et al. (2009). Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. JAPI 57, 163–170.
Misra A, Vikram NK (2002). Insulin resistance syndrome (metabolic syndrome) and Asian Indians. Curr Sci 83, 1483–1496.
Peterson KF, Dufour S, Feng J, Befroy D, Dziura J, Dall Man C et al. (2006). Increased prevalence of insulin resistance and nonalcoholic fatty liver disease in Asian-Indian men. Proc Natl Acad Sci USA 103, 18273–18277.
Peterson KF, Dufour S, Hariri A, Nelson-Williams C, Foo JN, Zhang X et al. (2010). Apolipoprotein C3 gene variants in non-alcoholic fatty liver disease. N Engl J Med 362 (Suppl 12), 1082–1088.
Sanyal AJ (2002). AGA technical review on nonalcoholic fatty liver disease. Gastroenterology 123, 1705–1725.
Sudha V, Radhika G, Mohan V (2004). Current dietary trends in type 2 diabetes. Ind J Med Res 120, 4–8.
Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, et al., American Heart Association Council on Clinical Cardiology Subcommittee on Exercise, Rehabilitation, and Prevention; American Heart Association Council on Nutrition, Physical Activity, and Metabolism Subcommittee on Physical Activity (2003). Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the American Heart Association Council on Clinical Cardiology (Subcommittee on Nutrition, Physical Activity and Metabolism (Subcommittee on Physical Activity). Circulation 107, 3109–3116.
Uchil D, Pipalia D, Chawla M, Patel R, Muniar S, Narayani et al. (2009). Nonalcoholic fatty liver disease (NAFLD)—the hepatic component of metabolic syndrome. JAPI 57, 201–204.
Vikram NK, Misra A, Pandey RM, Dwivedi M, Luthra K, Dhingra V et al. (2006). Association between subclinical inflammation & fasting insulin in urban young adult north Indian males. Ind J Med Res 124, 677–682.
Acknowledgements
We express our gratitude to all the subjects who consented to participate in this study. The help of K Shilpa Gupta, B Spoorthy, Meena Ramchandani and Saini Shinde in assistance in data collection is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sathiaraj, E., Chutke, M., Reddy, M. et al. A case-control study on nutritional risk factors in non-alcoholic fatty liver disease in Indian population. Eur J Clin Nutr 65, 533–537 (2011). https://doi.org/10.1038/ejcn.2011.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2011.3
Keywords
This article is cited by
-
Fatty liver index relationship with biomarkers and lifestyle: result from RaNCD cohort study
BMC Gastroenterology (2023)
-
Mouse models of nonalcoholic steatohepatitis and their application to new drug development
Archives of Pharmacal Research (2022)
-
The Genetics of Nonalcoholic Fatty Liver Disease: Role of Diet as a Modifying Factor
Current Nutrition Reports (2014)
-
Low Docosahexaenoic Acid Content in Plasma Phospholipids is Associated with Increased Non‐alcoholic Fatty Liver Disease in China
Lipids (2012)