Abstract
Hypoxia-inducible factor-1α is found frequently overexpressed in solid tumors cells, exerting an important role in angiogenesis, glucose metabolism, cell proliferation, survival and invasion. In thyroid carcinomas, hypoxia-inducible factor-1α expression was found increased in differentiated, poorly differentiated, medullary and anaplastic variants. Hypoxia represents the principal stimulus responsible for hypoxia-inducible factor-1α induction. Other nonhypoxic stimuli increase hypoxia-inducible factor-1α synthesis through the activation of phosphatidylinositol 3-kinase and mitogen-activated protein kinase pathways in a cell-type-specific manner. We have previously shown the role of BRAFV600E mutation in papillary thyroid cancer cells as a factor that facilitates tumor cell growth and progression. In this study, we tested the hypothesis that BRAFV600E mutation influences hypoxia-inducible factor-1α expression in papillary thyroid carcinoma cells. We analyzed 27 papillary thyroid carcinomas, 13 of which presented BRAFV600E mutation. In tumor tissues, immunoreactivity for hypoxia-inducible factor-1α was detected in the majority of analyzed BRAFV600E mutated cases. Transcriptional analyses revealed elevated hypoxia-inducible factor-1α levels with significant differences between wild-type and mutated group. A BRAF wild-type papillary thyroid carcinoma cell line and a BRAFV600E mutated papillary thyroid carcinoma cell line were selected to study the effects of BRAF mutation on hypoxia-inducible factor-1α expression in vitro. Knockdown of mutant BRAFV600E or both the wild type and the BRAFV600E by RNA interference induced a significant reduction of hypoxia-inducible factor-1α expression at mRNA and protein levels. Pharmacological inhibition of BRAF significantly reduces hypoxia-inducible factor-1α expression levels in papillary thyroid carcinoma cell line harboring BRAFV600E mutation. Our results suggest that hypoxia-inducible factor-1α is expressed in papillary thyroid carcinomas and is regulated not only by hypoxia but also by BRAFV600E-mediated signaling pathway.
Similar content being viewed by others
Main
Genetic alteration leading to aberrant activation of the RAS/RAF mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (ERK) signal transduction pathway has long been seen in many human cancers. Several studies report B-type Raf kinase (BRAF) mutation as a potent activator of MAPK pathway.1 BRAFV600E mutation is the most common mutation identified in the BRAF gene and represents a novel indicator of poorer prognosis in a broad range of human cancers especially in thyroid cancers.2, 3, 4, 5
Papillary thyroid carcinoma is the most frequent thyroid cancer accounting for 85–90% of all thyroid malignancies.6
BRAFV600E mutation was found exclusively in papillary thyroid carcinoma and in papillary thyroid carcinoma-derived anaplastic thyroid carcinoma; in papillary thyroid carcinoma the overall prevalence of BRAFV600E mutation is relatively high, around 45% on average, influencing the expression levels of several molecular markers through constitutive activation of the MAPK/ERK pathway, providing a potent promitogenic force that drives malignant transformation.7, 8
Recent evidence has implicated the BRAF/MAPK MEK/ERK pathways as regulators of the transcriptional enhancer hypoxia-inducible factor-1 (HIF-1).9 HIF-1 consists of a heterodimer of two proteins (HIF-1α and HIF-1β), which mediates the transcription of several genes involved in angiogenesis, glucose metabolism, cell proliferation, survival and tumor metastases.10
Intratumoral hypoxia and genetic alterations selectively regulate HIF-1α subunit through different mechanisms. Hypoxia ubiquitous induces HIF-1α in all cells tested, decreasing its degradation by the ubiquitin–proteasome system.11 Other nonhypoxic stimuli, such as growth factors, cytokines and oncogenic signals, increase HIF-1α synthesis through the activation of Akt/phosphatidylinositol 3-kinase and MAPK pathways in a cell-type-specific manner.12 HIF-1α is generally overexpressed in solid tumors including lung, prostate, breast and colon carcinoma;13 BRAFV600E mutation increases HIF-1α expression in melanoma cells, exerting an important role in melanoma cell survival under hypoxic conditions.14
HIF-1α expression was found increased at transcripts and protein levels in differentiated, poorly differentiated, medullary and anaplastic carcinoma of the thyroid.15, 16, 17
In this study, we tested the hypothesis that BRAFV600E mutation influences HIF-1α expression levels in papillary thyroid carcinoma cells, using RNA interference targeting BRAF and the RAF-1 kinase inhibitor (sorafenib), which target both the wild-type and the V600E mutant BRAF in vitro.1, 18, 19, 20
Materials and methods
Case Selection
In our previous work, BRAFV600E mutation was evaluated in a series consecutive of patients by a real-time, allele-specific amplification essentially as described by Jarry et al.21, 22 Here we randomly selected 27 patients from the described group. Age of the 27 patients who underwent surgery for the classical variant of papillary thyroid carcinoma ranged from 17 to 76 years (median age was 48 years), and there was a strong predominance of female patients (81%). For each case, all histological slides were reviewed by two pathologists (AM and VR), and histological diagnoses were reassessed according to the World Health Organization Classification of Tumours.23 All primary tumors included in this study were classified as classical variants of papillary thyroid carcinoma; tumors with morphological features of the follicular or others variants of papillary carcinoma were not included.
BRAFV600E mutation was present in 13 (48%) of the 27 tumors examined. This retrospective study was performed in accordance with the rules of the institutional review board at the Faculty of Medicine (University of Palermo).
Immunohistochemistry
Tissue samples were fixed in 10% buffered formalin, dehydrated in ethanol and paraffin-embedded according to the routine technique. Immunohistochemical analyses were performed on 3-μm-thick paraffin-embedded sections of thyroid tumors. Dewaxed sections were heated for antigen unmasking in Tris/EDTA solution (pH 9) in a water bath for 30 min at 98°C. After rinsing in distilled H2O, we inhibited endogenous peroxidase with 3% H2O2 for 5 min. Unspecific staining was blocked with protein block (Novolink Polymer Detection System; Novocastra Laboratories, Newcastle, UK). Sections were subsequently exposed to rabbit polyclonal anti-HIF-1α (1:100) (Novus Biologicals, Littleton, CO, USA) or unconjugated rabbit immunoglobulins (negative control) overnight at 4°C. Staining was detected using Novolink Polymer Detection System, (Novocastra Laboratories) according to manufacturer's instructions and counterstained with aqueous hematoxylin. Human melanoma tissues from our archives were used as HIF-1α antibody-positive control (data not shown).
The non-neoplastic tissue present on the same slides was considered as a healthy control.
Immunohistochemical Evaluation
For the evaluation of HIF-1α immunoreactions, we examined tissues for evidence of staining. For each case a minimum of 103 cells was counted under high-powered fields (final magnification × 400) and reported as the percentage of expressing cells among the total number of counted cancer cells and regarded as a labeling index. Cases were evaluated separately by two different pathologists (AM and VR); because the variation was less than 5%, the first pathologist's data were used.
Cell Lines and Culture Conditions
Human papillary thyroid cell lines, BCPAP and FB2, were kindly provided by Dr F Frasca, University of Catania, Italy. BCPAP cell line, harboring the BRAFV600E mutation in hemizygous,24 was cultured in RPMI 1640 medium containing 10% heat-inactivated fetal bovine serum in 5% CO2. FB2 cell line was cultured in DMEM medium containing 10% fetal bovine serum in 5% CO2. CoCl2 is a hypoxia mimic and is known to stabilize HIF-1α in the cells. For CoCl2 treatment, thyroid cells were subjected to 100 μmol/l CoCl2 for 24 h in a CO2 incubator.
Thyroid cancer cell lines were cultured, respectively, in the presence of sorafenib (LKT Laboratories, St Paul, MN, USA) 5 μmol/l in dimethyl sulfoxide (DMSO) or DMSO as control for 24 h; after exposures, cells were detached with trypsin/EDTA for HIF-1α mRNA analyses.
Immunofluorescence
Cells were cultured on chamber slides (Labtek, Nunc, Naperville, IL, USA) in RPMI 1640 medium containing 10% fetal bovine serum fixed in 2% paraformaldehyde/phosphate-buffered saline, permeabilized in phosphate-buffered saline containing Triton X-100 for 3 min at room temperature, and stained with rabbit polyclonal antibody anti-HIF-1α (Upstate, Millipore, Billerica, MA, USA) antibody overnight at 4°C. Cells were then incubated with Alexa Fluor 488 goat anti-rabbit IgG (Invitrogen, Carlsbad, CA, USA) antibody for 1 h in the dark. Slides were mounted with UltraCruz mounting medium containing 4′,6-diamidino-2-phenylindole used to counterstain nuclei (Santa Cruz Biotechnology, Heidelberg, Germany). Images were captured with a fluorescence microscope (DM4000B; Leica Microsystems, Wetzlar, Germany).
Generation of siRNA for Transfection
Small-interference duplex RNA (siRNA) targeting human BRAF were purchased (synthesized) from MWG as described by Wellbrock et al.25 These siRNAs target both the sequence outside and inside the V600E mutation site and thus abrogates the expression of BRAFV600E and BRAF wild-type specifically. A nonspecific siRNA (scrambled) was also synthesized. BCPAP cells were plated in six-well plates at 3 × 105 per well. After 24 h of plating, we transfected cells with scrambled, BRAFV600E siRNA (Mu-A) or BRAF wild-type siRNA (Com-4) using Interferin siRNA transfection reagent (Polyplus-transfection SA, Illkirch, France) according to the manufacturer's instructions. After 72 h of transfection, we detached cells with trypsin/EDTA, and harvested them. Knockdown efficiency was evaluated by qRT-PCR and western blot analysis.
Isolation of Total RNA and qRT-PCR
Total RNA was extracted from formalin-fixed paraffin-embedded 10 μm sections of cancer thyroid tissues using High Pure RNA Paraffin Kit (Roche Diagnostic, Mannheim, Germany). Total RNA was extracted and purified from BCPAP and FB2 cell lines using the RNeasy Mini kit (Qiagen Italia, Milan, Italy), including a digestion step with DNase I set. RNA quantity and quality were assessed by UV spectrophotometry.
Total RNA (2 μg) was reverse transcribed in a volume of 20 μl with Oligo dT primers (Applied Biosystems, Darmstadt, Germany) and ImpromII RT (Promega Italia, Milan, Italy), according to the manufacturer's protocol.
BRAF and HIF-1α expression was analyzed by real-time quantitative PCR (qRT-PCR) in individual samples. Two microgram of total RNA was used to measure mRNA levels relative to β-actin mRNA expression. PCR primers and probes were purchased from Qiagen (Quantitect Primer BRAF and HIF α). All reactions were performed in a final volume of 20 μl with 2 μl cDNA template using a LightCycler (Roche Diagnostics). Data analysis was performed with qBASE Browser that uses a Δ-Ct relative quantification model with PCR efficiency correction and single reference gene normalization (β-actin: 5′-GGACTTCGAGCAAGAGATGG-3′ and 5′-AGCACTGTGTTGGCGTACAG-3′).26
Western Blotting
Human papillary thyroid cell lines BCPAP and FB2 were resuspended in ice-cold NP-40 lysis buffer (50 mM Tris-HCl (pH 7.6), 150 mM NaCl, 1% NP-40, 1% SDS, 0.5 sodium deoxycolate, 2 mM NaF, 2 mM sodium orthovanadate (Na3VO4)) and protease inhibitors (Complete Roche Diagnostic). Cells were incubated for 30 min on ice and lysates were cleared at 14 000 r.p.m. for 30 min. A 30 μg aliquot of each sample was mixed with reduce Laemmli sample buffer and electrophoresed on a 4–12% SDS–PAGE (NuPage Novex 4–12% Bis-Tris Gel; Invitrogen) before transfer to PVDF membrane. Membrane staining was assessed using specific antibodies for β-actin (1:5000) (monoclonal mouse anti-human β-actin, clone AC-15; Sigma-Aldrich), HIF-1α (1:1000) (Novus Biologicals) and BRAF (1:1000) (monoclonal mouse anti-human B-raf, clone F-7; Santa Cruz Biotechnology, Santa Cruz, CA, USA). Peroxidase-conjugated anti-mouse or anti-rabbit antibodies (Santa Cruz Biotechnology) and SuperSignal (Pierce, Rockford, IL, USA) were used for detection with a Bio-Rad Chemidoc XRS Imager.
Statistical Analyses
Continuous variables were analyzed as median and interquartile range. As continuous variables were without normal distribution, we used nonparametric tests and analyzed differences by the Mann–Whitney U-test. P<0.05 was considered statistically significant. All analyses were performed with Statistical Package for Social Science (SPSS for Windows, version 11.0; ©SPSS, Chicago, IL, USA).
Results
The clinicopathological characteristics of the 27 patients who underwent surgery for the classic variant of papillary thyroid carcinomas (PTCs) are shown in Table 1.
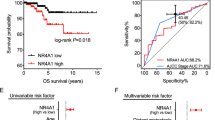
HIF-1α Expression Is Increased in PTCs with BRAFV600E Mutation
On the basis of the presence of BRAFV600E mutation, we divided human tumor specimens in two subgroups, 13 cases with BRAFV600E mutation and 14 without BRAFV600E mutation. Immunohistochemical staining was performed to identify the presence of the HIF-1α protein; immunoreaction was revealed in all cases but two of the wild-type group.
In the mutated group, we found a median value of labeling index of 60.4% (53.45–70.25%), whereas in the wild-type group the median labeling index was 18.55% (11.36–26.10%); these differences proved to be significant (P<0.001). Generally, immunoreactivity for HIF-1α was detected with intense cytoplasmatic and nuclear positivity in tumor cells of cases with BRAFV600E mutation, whereas a weak cytoplasmatic expression was found in tumor cells of the wild-type group (Figure 1a and b). In our specimens HIF-1α positivity was detected throughout the analyzed fields, not associated with areas of necrosis, and also observed in cells immediately adjacent to blood vessels. Adjacent non-neoplastic tissue, the stromal and follicular cells did not show immunoreactivity for HIF-1α (data not shown).
HIF-1α mRNA expression levels were analyzed in all samples considered. We found that in the mutated group HIF-1α mRNA expression showed the median value of 73.25 (45.18–91.09) relative levels, whereas in the wild-type group the median was 23.47 (16.23–31.67); these differences proved to be significant (P<0.001) (Figure 2).
PTC Cell Lines Express HIF-1α
To study the effects of BRAF mutation on HIF-1α expression, we selected a BRAF wild-type papillary thyroid carcinoma cell line (FB2) and a BRAFV600E mutated papillary thyroid carcinoma cell line (BCPAP). To analyze the expression pattern and the intracellular localization of HIF-1α in thyroid cancer cell lines, we conducted an immunofluorescence staining with an antibody specific to HIF-1α (Figure 3, green). Nuclei were counterstained with 4′,6-diamidino-2-phenylindole (Figure 3, blue). The results showed that HIF-1α was barely expressed on the cytoplasm of FB2 cell line (Figure 3, upper panel, merge), whereas a strong nuclear localization was revealed on BCPAP cells (Figure 3, lower panel, merge).
HIF-1α gene expression evaluated by qRT-PCR was found 14-fold increased in papillary thyroid carcinoma cell line harboring BRAFV600E mutation comparing with papillary thyroid carcinoma cell line with wild-type BRAF (Figure 4).
Expression of HIF-1α mRNA in cultured BCPAP and FB2 cell lines as assessed by quantitative PCR. mRNA expression in the mutated group is lower than that in the wild-type group. The results are shown relative to mRNA levels from the corresponding control cells, assigned the value 1. One representative of three experiments in total of each cell type is shown in the figure. β-Actin was used as internal control.
BRAF Knockdown Decreases HIF-1α Expression Levels
To evaluate the role of the BRAF mutation in the regulation of HIF-1α transcription and expression, we knocked down BRAF with siRNA duplexes. Two well-characterized RNA interference constructs were used that selectively knockdown the mutant V600E BRAF (Mu-A) or both the wild-type and the mutated form (Com-4). The effective block of BRAF was verified by evaluating BRAF expression at mRNA and protein levels. Exposure of BCPAP cells to Mu-A or to Com-4 siRNA constructs was associated with a marked downregulation of BRAF expression at RNA level (Figure 5, left panel). Remarkably, western blot analysis revealed a significant reduction of BRAF protein in silenced cells. In contrast, there was no detectable downregulation of BRAF in BCPAP cells exposed to unspecific siRNA (Figure 6).
BRAF expression in thyroid cancer cell lines after silencing. Western blot analysis revealed a significant reduction of BRAF protein in silenced cells. No detectable downregulation of BRAF in BCPAP cells exposed to scrambled (upper panel). One representative of three experiments is showed. Densitometric analysis relative to BRAF protein levels vs β-actin expressed as percentage of optical density (OD) (lower panel).
Moreover, FB2 cells exposed only to Com-4 showed a significant reduction of BRAF expression at transcription level (Figure 5, right panel).
Therefore, analysis of HIF-1α expression levels in BRAF silenced cells by real-time PCR revealed a significant reduction of HIF-1α transcription (Figure 7a). Knockdown of both wild-type and mutated V600E BRAF decreased HIF-1α with a comparable effect. No differences in HIF-1α mRNA expression level were detected in FB2 BRAF knockdown cells compared with untreated or scrambled siRNA treated cells (Figure 7b). Remarkably, as shown by western blot analysis and its relative densitometric analysis, BRAF knockdown has a significant effect in attenuating HIF-1α expression at protein level in BCPAP cells (Figure 8, upper and lower panels).
(a) Expression of HIF-1α mRNA in BRAF silenced BCPAP cell lines assessed by quantitative PCR. (b) Expression of HIF-1α mRNA in BRAF silenced FB2 cell lines assessed by quantitative PCR. The results are shown relative to mRNA levels from the corresponding control cells, assigned the value 1. One representative of three experiments in total of each cell type is shown in the figure. Normalization was carried out by using the gene β-actin as housekeeping control.
Western blot analysis revealed a strong reduction of HIF-1α protein in BCPAP silenced cells. No detectable downregulation of HIF-1α in BCPAP cells exposed to scrambled (upper panel). One representative of three experiments is showed. Densitometric analysis relative to BRAF protein levels vs β-actin expressed as percentage of optical density (OD; lower panel).
Pharmacological Inhibition of BRAF Reduces HIF-1α Expression
To confirm BRAF knockdown experiments, we next study the pharmacological inhibition of BRAF. Treatment with sorafenib induced a ∼2-fold reduction of HIF-1α mRNA levels in BCPAP in comparison with untreated cells. No differences were seen in FB2-treated cells comparing with DMSO control (Figure 9).
Discussion
BRAF serine/threonine kinase regulates the expression levels of several molecular markers through the activation of the MAPK/ERK pathway. BRAF mutations are known to alter the biological status of cancer cells, promoting tumor progression in a range of cancers such as melanoma, colon carcinoma and thyroid carcinoma.3, 25, 27 BRAFV600E is the most common mutation identified in thyroid papillary carcinoma, representing a novel indicator of poorer prognosis.28 Several proteins have been shown to be targeted by BRAFV600E-mediated activation. Recent studies indicate that in melanoma and in thyroid cancer cell lines, harboring BRAFV600E mutation, the activation of oncogenic pathways was observed, which have been reported to influence HIF-1α expression.14, 15, 29
In this study, we report that BRAFV600E mutation increased HIF-1α expression levels in papillary thyroid carcinoma cells. Moreover, molecular and pharmacological targeting of BRAF results in significant reduction of HIF-1α expression in thyroid tumor cells.
In several human cancers, HIF-1α is generally found overexpressed in solid tumors, including lung, prostate, breast and colon carcinoma, as a result of intratumoral hypoxia or genetic alteration due to the upregulation of oncogenes or downregulation of tumor suppressor genes.13 HIF-1α overexpression has been positively associated with tumor aggressiveness and poorer prognosis.9, 30, 31
Burrows et al15 reported that HIF-1α protein is regulated by a combination of tumor genotype and microenvironment with a highest expression and a diffuse distribution of positivity in the aggressive dedifferentiated, anaplastic thyroid tumors and a focal expression in differentiated papillary and follicular tumors.
In our specimens, HIF-1α positivity was detected throughout the analyzed fields, not associated with areas of necrosis and also observed in cells immediately adjacent to blood vessels, suggesting an O2-independent regulatory mechanism, such as genetic alteration, that could influence HIF-1α expression levels.
More than 60 putative direct HIF-1α target genes have been identified involved in angiogenesis, glucose metabolism, cell proliferation, survival and invasion, including vascular endothelial growth factor, erythropoietin, nitric oxide synthase, heme oxygenase 1 and glucose transporters.10
It is well known that vascular endothelial growth factor exerts a key role in tumor aggressiveness, becoming a target in cancer therapy.32 Jo et al7 reported that vascular endothelial growth factor was significantly higher in PTCs harboring BRAFV600E mutation, thus suggesting that HIF-1α could increase the expression of vascular endothelial growth factor in BRAFV600E-mutated PTCs.
Recent literature indicated that modulation of HIF-1α expression influences the sensitivity to chemotherapy and more importantly for thyroid tumors, to radiotherapy.15, 33 Here we have shown that silencing BRAF by the two well-characterized RNA interference constructs used, which selectively knockdown the mutant V600E BRAF (Mu-A) or both the wild-type and the mutated form (Com-4), leads to a significant reduction of HIF-1α expression in papillary thyroid cell line harboring BRAFV600E mutation even in hypoxia-mimetic conditions, indicating a predominant role BRAFV600E oncogenic activation.
Recent studies reported that sorafenib exerts a significant antitumor activity in advanced thyroid cancer, particularly in thyroid tumors harboring BRAF mutation, inhibiting cancer cell proliferation and inducing apoptosis.19, 34 Accordingly, our results showed that sorafenib significantly reduces HIF-1α expression levels in papillary thyroid cancer cells line only with V600E-mutated BRAF, suggesting a BRAFV600E-dependent mechanism for sorafenib in the regulation of HIF-1α expression.
In summary, our results showed that HIF-1α is expressed in PTCs and in the considered cell lines, and that it is also regulated by BRAFV600E oncogenic activation.
This work aims to give new insights into mechanisms responsible for upregulation of HIF-1α in the classical variant of papillary thyroid cancers.
Therefore, we believe that HIF-1α downregulation could be considered to increase the effectiveness of conventional treatment of thyroid cancer.
References
Wan PT, Garnett MJ, Roe SM, et al. Mechanism of activation of the RAF-ERK signaling pathway by oncogenic mutations of B-RAF. Cell 2004;116:855–867.
Cohen Y, Xing M, Mambo E, et al. BRAF mutation in papillary thyroid carcinoma. J Natl Cancer Inst 2003;95:625–627.
Frasca F, Nucera C, Pellegriti G, et al. BRAF(V600E) mutation and the biology of papillary thyroid cancer. Endocr Relat Cancer 2008;15:191–205.
Liu D, Liu Z, Condouris S, et al. BRAF V600E maintains proliferation, transformation, and tumorigenicity of BRAF-mutant papillary thyroid cancer cells. J Clin Endocrinol Metab 2007;92:2264–2271.
Xing M . BRAF mutation in thyroid cancer. Endocr Relat Cancer 2005;12:245–262.
Hundahl SA, Fleming ID, Fremgen AM, et al. A National Cancer Data Base report on 53 856 cases of thyroid carcinoma treated in the U.S. 1985–1995. [see comments]. Cancer 1998;83:2638–2648.
Jo YS, Li S, Song JH, et al. Influence of the BRAF V600E mutation on expression of vascular endothelial growth factor in papillary thyroid cancer. J Clin Endocrinol Metab 2006;91:3667–3670.
Xing M . BRAF mutation in papillary thyroid cancer: pathogenic role, molecular bases, and clinical implications. Endocr Rev 2007;28:742–762.
Lim JH, Lee ES, You HJ, et al. Ras-dependent induction of HIF-1alpha785 via the Raf/MEK/ERK pathway: a novel mechanism of Ras-mediated tumor promotion. Oncogene 2004;23:9427–9431.
Semenza GL . Targeting HIF-1 for cancer therapy. Nat Rev Cancer 2003;3:721–732.
Kunz M, Ibrahim SM . Molecular responses to hypoxia in tumor cells. Mol Cancer 2003;2:23.
Dery MA, Michaud MD, Richard DE . Hypoxia-inducible factor 1: regulation by hypoxic and non-hypoxic activators. Int J Biochem Cell Biol 2005;37:535–540.
Zhong H, De Marzo AM, Laughner E, et al. Overexpression of hypoxia-inducible factor 1alpha in common human cancers and their metastases. Cancer Res 1999;59:5830–5835.
Kumar SM, Yu H, Edwards R, et al. Mutant V600E BRAF increases hypoxia inducible factor-1alpha expression in melanoma. Cancer Res 2007;67:3177–3184.
Burrows N, Resch J, Cowen R, et al. Expression of hypoxia inducible factor 1{alpha} in thyroid carcinomas. Endocr Relat Cancer 2010;17:61–72.
Jubb A, Hillan K . Expression of HIF-1 alpha in human tumours. J Clin Pathol 2005;58:1344.
Scarpino S, Cancellario d’Alena F, Di Napoli A, et al. Increased expression of Met protein is associated with up-regulation of hypoxia inducible factor-1 (HIF-1) in tumour cells in papillary carcinoma of the thyroid. J Pathol 2004;202:352–358.
Lyons JF, Wilhelm S, Hibner B, et al. Discovery of a novel Raf kinase inhibitor. Endocr Relat Cancer 2001;8:219–225.
Preto A, Goncalves J, Rebocho AP, et al. Proliferation and survival molecules implicated in the inhibition of BRAF pathway in thyroid cancer cells harbouring different genetic mutations. BMC Cancer 2009;9:387.
Wilhelm S, Carter C, Lynch M, et al. Discovery and development of sorafenib: a multikinase inhibitor for treating cancer. Nat Rev Drug Discov 2006;5:835–844.
Jarry A, Masson D, Cassagnau E, et al. Real-time allele-specific amplification for sensitive detection of the BRAF mutation V600E. Mol Cell Probes 2004;18:349–352.
Rodolico V, Cabibi D, Pizzolanti G, et al. BRAF V600E mutation and p27 kip1 expression in papillary carcinomas of the thyroid < or=1 cm and their paired lymph node metastases. Cancer 2007;110:1218–1226.
DeLellis RA, Lloyd RV, Heitz PU, et al. (eds). World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Endocrine Organs. IARC Press: Lyon, France, 2004, pp 50–57.
Fabien N, Fusco A, Santoro M, et al. Description of a human papillary thyroid carcinoma cell line. Morphologic study and expression of tumoral markers. Cancer 1994;73:2206–2212.
Wellbrock C, Ogilvie L, Hedley D, et al. V599EB-RAF is an oncogene in melanocytes. Cancer Res 2004;64:2338–2342.
Hellemans J, Mortier G, De Paepe A, et al. qBase relative quantification framework and software for management and automated analysis of real-time quantitative PCR data. Genome Biol 2007;8:19.
Li WQ, Kawakami K, Ruszkiewicz A, et al. BRAF mutations are associated with distinctive clinical, pathological and molecular features of colorectal cancer independently of microsatellite instability status. Mol Cancer 2006;5:2.
Salvatore G, De Falco V, Salerno P, et al. BRAF is a therapeutic target in aggressive thyroid carcinoma. Clin Cancer Res 2006;12:1623–1629.
Bardos JI, Ashcroft M . Hypoxia-inducible factor-1 and oncogenic signalling. Bioessays 2004;26:262–269.
Semenza G . Signal transduction to hypoxia-inducible factor 1. Biochem Pharmacol 2002;64:993–998.
Semenza GL . HIF-1 and tumor progression: pathophysiology and therapeutics. Trends Mol Med 2002;8:S62–S67.
Ahmed SI, Thomas AL, Steward WP . Vascular endothelial growth factor (VEGF) inhibition by small molecules. J Chemother 2004;16:59–63.
Moeller BJ, Dewhirst MW . Raising the bar: how HIF-1 helps determine tumor radiosensitivity. Cell Cycle 2004;3:1107–1110.
Gupta-Abramson V, Troxel AB, Nellore A, et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 2008;26:4714–4719.
Acknowledgements
This work was in part supported by grants from the Ministero dell’Istruzione dell’Università e della Ricerca (MIUR) 60% (VR). We are grateful to Dr Anna Claudia Bommarito for expert technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zerilli, M., Zito, G., Martorana, A. et al. BRAFV600E mutation influences hypoxia-inducible factor-1α expression levels in papillary thyroid cancer. Mod Pathol 23, 1052–1060 (2010). https://doi.org/10.1038/modpathol.2010.86
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.86
Keywords
This article is cited by
-
Association Between 18F-FDG Avidity and the BRAF Mutation in Papillary Thyroid Carcinoma
Nuclear Medicine and Molecular Imaging (2016)
-
Current Standards in Treatment of Radioiodine Refractory Thyroid Cancer
Current Treatment Options in Oncology (2016)
-
Molecular pathogenesis and mechanisms of thyroid cancer
Nature Reviews Cancer (2013)
-
Oncogenes and angiogenesis: a way to personalize anti-angiogenic therapy?
Cellular and Molecular Life Sciences (2013)
-
In papillary thyroid carcinoma, TIMP-1 expression correlates with BRAF V600E mutation status and together with hypoxia-related proteins predicts aggressive behavior
Virchows Archiv (2013)