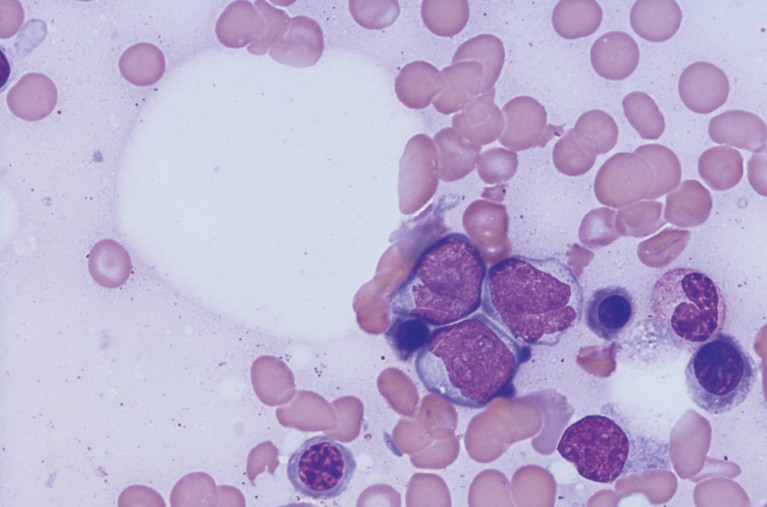
AML represents approximately 14% of all registered paediatric leukaemia cases in Saudi Arabia.© OGPHOTO/ ISTOCK / GETTY IMAGES PLUS
Acute myeloid leukaemia (AML) — a type of cancer characterized by the rapid growth of abnormal white blood cells in the bone marrow — accounts for roughly 15–20% of all leukaemia cases in children. With recent advances in treatment and supportive care, the survival rates of AML for children in developed nations, such as Ireland, the United Kingdom and the United States, have greatly improved to 60–70%. However, the status of AML for children in developing nations, particularly those in the Middle East, is unclear.
Wasil Jastaniah at the Princess Noorah Oncology Center, part of Saudi Arabia’s Ministry of National Guard—Health Affairs, and co-authors have now performed a retrospective study on the status of AML for children in the kingdom. They found that a risk–response strategy has boosted the survival outcomes in the kingdom to world-class standards.
Relapse — the recurrence of AML in patients — is currently the biggest obstacle to leukaemia treatment and recovery. The researchers followed the status of 175 AML patients aged 14 years or younger treated across nine medical institutions in Saudi Arabia over five years. They noted that of the 175 AML patients, treatment of 21 (12%) failed in the first phase, 67 (38.3%) experienced relapse and 66 (37.7%) died within the study period. The cumulative incidences of relapse and non-relapse mortality were determined to be 43.1% and 9.8% respectively.
Most significantly, the overall survival was estimated to be 58.8 ± 4%, which was comparable to that of North America (65.4 ± 4%) and those of United Kingdom, Ireland, Netherlands and New Zealand (61%). They attributed the unexpectedly high survival rate in Saudi Arabia to two things: hematopoietic stem cell transplantation and tailored treatment. The latter, in particular, utilises a risk- and response-based stratification system that optimises the selection of AML therapies for different patients.
Saudi Arabia is a high-income, resource-rich country that has been providing free cancer treatment to its nationals. The number of cancer centres in Saudi Arabia has increased over the past 20 years, resulting in improved access to treatment and supportive care.
The findings from this study suggest that tailored treatment for AML patients using a risk–response strategy has significant benefits and that, with the right implementation, developing countries can achieve comparable survival outcomes as those of developed countries.
“Future improvements in outcomes of childhood AML in Saudi Arabia would require further refinement of risk stratification and tailoring therapy based on risk and response,” says Jastaniah.


