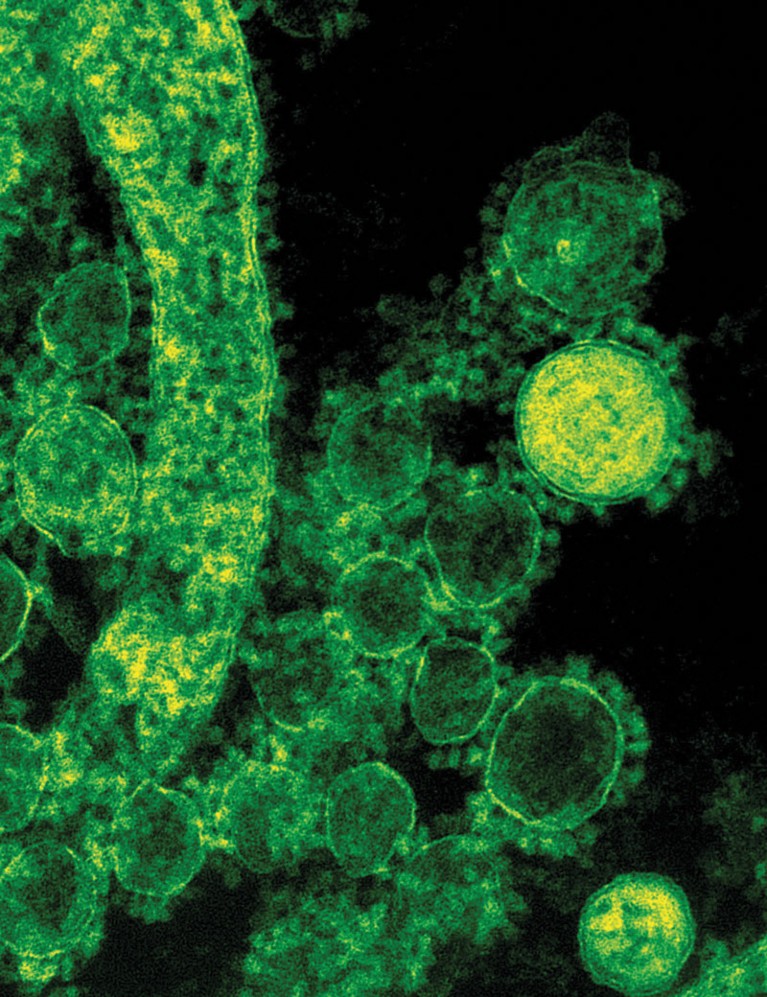
Electron microscopy image of the MERS-causing virus.NIAID / CC. BY 2.0
The blood plasma of people recovering from Middle East respiratory syndrome (MERS) could be a source of antibodies to treat patients in the grip of the disease. Researchers at KAIMRC reached this conclusion from a feasibility study conducted at Saudi Arabia’s Ministry of National Guard—Health Affairs (MNGHA) with co-workers elsewhere in Saudi Arabia and in the US, Canada and Europe. Their research did not involve trials of the proposed antibody therapy, but it did establish that collecting sufficient antibodies from patients may be a realistic proposition.
MERS is caused by a virus that was first identified in 2012 in a patient in Saudi Arabia. More than 36% of identified cases have proved fatal; and although the disease has been detected in many countries, 80% of cases have been in Saudi Arabia.
“No therapy options have been proven to be effective, so developing a treatment using donated plasma would be of great value,” says MNGHA’s Yaseen Arabi, who led the feasibility study. Administering donated blood plasma containing anti-viral antibodies is known to be an effective treatment for other serious viral diseases.
The researchers explored three possible sources of therapeutically useful plasma. These were 196 patients with acute respiratory illness and confirmed or suspected MERS virus infection, 230 healthcare workers who had been in contact with MERS patients, and 17 household contacts of patients. Blood samples from these three groups of potential donors were screened for the presence of antibodies able to bind to the MERS virus.
Significant amounts of antibody were detected in only a small number of the sample participants, with recently recovered MERS patients seeming to be the most suitable source. Although potentially useful amounts of antibody were detected in fewer than 3% of the study participants, Arabi remains positive, saying, “Our results do indicate it could be possible to obtain plasma, although with the small pool of potential donors, collecting large quantities to use in therapeutic studies may be challenging.”
Moving on to clinical trials of donated plasma is the obvious next step, but there are several challenges ahead before reaching that stage.
“We do need to explore other ways to obtain sufficient plasma with therapeutically useful amounts of antibody,” says Arabi. Possible options may be to use samples from patients who have just recovered from more severe disease. Also, strict criteria must be met to include potential plasma donors in clinical trials. With the feasibility of the approach demonstrated in principle, such issues can now be addressed.


