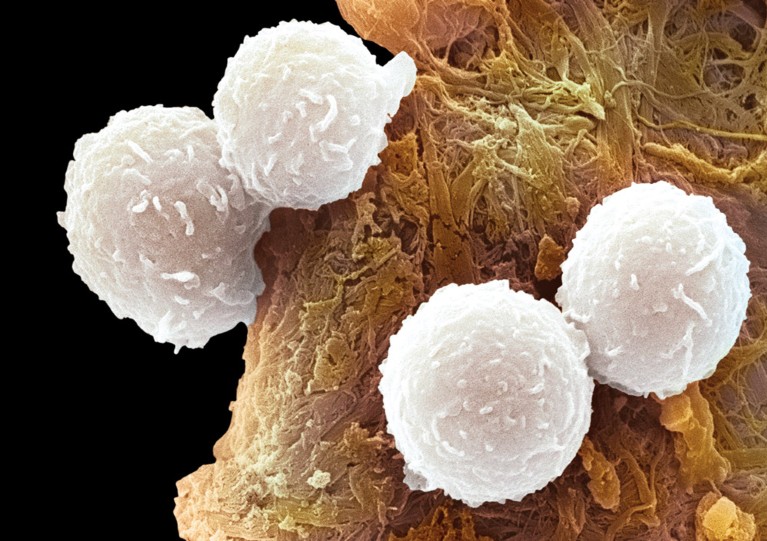
B cell from a patient with leukaemia.© STEVE GSCHMEISSNER / SCIENCE PHOTO LIBRARY / GETTY IMAGES
Pakistani children affected by B cell acute lymphoblastic leukaemia (B-ALL), a common type, show poor survival compared to children in other parts of the world.A study conducted by KAIMRC in collaboration with hospitals and universities in Pakistan found that some genetic abnormalities normally associated with more aggressive types of cancer are common in B-ALL patients from the India- Pakistan region.
B-ALL is the most prevalent type of cancer in children. It develops in blood-forming cells and is characterised by the overproduction of immature white blood cells. One of its causes is the presence of fusion oncogenes (FOs), which are genes that form when two previously separate genes unite.
Scientists analysed 188 blood samples from 2- to 15-year-old Pakistani children with B-ALL who were being treated at oncology centres in Lahore, Faisalabad, Islamabad and Peshawar. They found that 87.2% of the patients had FOs. In particular, the study investigated how four types of FOs were correlated to disease biology and treatment outcome.
Similar to previous studies conducted in Pakistan and India, the fusion oncogene BCR-ABL was found to be the most common, detected in almost half of the patients. This mutation seems to be rare (2-5%) in B-ALL paediatric patients in Europe, the US, Saudi Arabia, Korea and Japan, but overrepresented in the India-Pakistan region. It is associated with older children (7 to 15 years old), lower remission (meaning temporary recovery) rates and poor survival. BCR-ABL codes for a mutant protein called tyrosine kinase, which causes unregulated cell division. Similarly, the FO MLL-AF4 was found to be relatively higher in the Pakistani patients (18%) compared to B-ALL patients in other parts of the world (1 to 17% depending on location) and it is correlated with short survival (52 weeks on average).
“Pakistani children with B-ALL have uniquely high frequencies of the FOs BCR-ABL and MLL-AF4. This, together with delays in diagnosis as well as shortage of specialised health professionals and treatment facilities may be some of the most important reasons for the overall poor outcome of paediatric B-ALL patients in Pakistan. We recommend the mandatory use of molecular testing for diagnosis and prognosis, the provision of tyrosine kinase inhibitorsfor treatment and the construction of more hematopoietic stem cell transplantation facilities at cancer centres,” says KAIMRC geneticist Zafar Iqbal, the leading author of this study.
The reason some FOs are more abundant among Pakistanis is not clear. “Further studies with comprehensive genetic analyses are necessary to deepen our understanding of the genetic basis of the patients’ poor prognosis,” he says.


