Credit: Laura N-Tamara
Not all babies are born with fully functional hearts. Physicians, however, are working hard to improve surgical techniques with the hope of enabling these babies to live longer with a better quality of life.
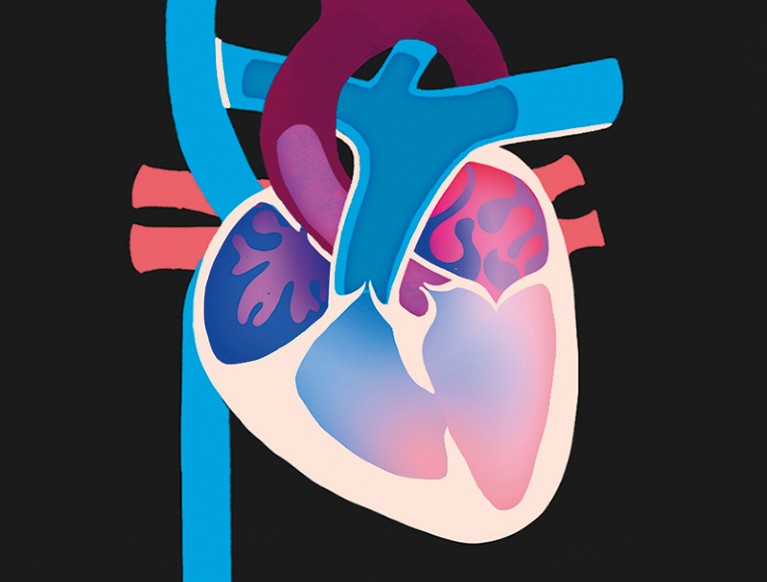
The human heart has four chambers: two atria, which receive blood; and two ventricles, which push blood from the heart to the rest of the body. In a healthy heart, the right ventricle pumps deoxygenated blood to the lungs and the larger, left ventricle pumps oxygenated blood received from the lungs out to the extremities and to other organs.
Part of Nature Outline: Single-ventricle heart defects
However, around 9 in every 100,000 people have a defect in one of their ventricles (Y. Liu et al. Int. J. Epidemiol. 48, 455–463; 2019). These single-ventricle defects (SVDs) encompass a broad spectrum of congenital heart problems. In some cases, a ventricle is missing altogether and in other cases, one of the ventricles is so small or malformed that it fails to function.
There are three main types of SVD. In hypoplastic left heart syndrome, the aorta and the left ventricle are small and underdeveloped. Pulmonary atresia is marked by two problems in the right ventricle, which is undersized and blocked off from the artery that should carry deoxygenated blood to the lungs. In the third form of SVD, called tricuspid atresia, the valve between the right atrium and ventricle is missing. Additionally, the wall between the left and right ventricles is either absent or perforated.
In all three of these SVDs, there is also usually a hole between the left and right atria. This extra defect causes oxygenated blood in the left atrium to mix with deoxygenated blood in the right atrium. As a result, a mix of blood flows to the lungs and the rest of the body. In the immediate term, this ensures that at least some blood is able to reach both the lungs and the body, enabling the baby to be born. However, in this situation, none of the organs get enough oxygen to be healthy; for the child to live a healthy life, the heart must be remodelled.
SVDs are treated through a sequence of surgeries, the first of which is performed soon after birth. Collectively, these operations are designed to redirect deoxygenated blood returning from the body away from the heart and straight to the lungs instead. With this reconfiguration, the heart’s only main remaining job is to pump oxygenated blood returning from the lungs out to the body — eliminating the problem of mixed blood.
Surgeons are also pioneering procedures to begin treatment from within the womb. Fetal balloon atrial septostomy, for example, is a technique designed to treat fetal hearts with an SVD but no crucial secondary defect, which is a relatively rare combination. Surgeons, guided by ultrasound, insert a small needle through the mother’s abdomen and into the baby’s heart, piercing the wall between the atria. This hole is enlarged by an inflating balloon and a tube is then installed to keep the hole open. Finally, the balloon is deflated and extracted along with the needle. This allows oxygenated and deoxygenated blood to mix, giving the baby a chance to survive long enough for corrective surgery. But this kind of intervention is still experimental, and only offered at a few hospitals.

 How to repair a baby’s broken heart
How to repair a baby’s broken heart
 Video: Babies with misshapen hearts
Video: Babies with misshapen hearts