
A pharmaceutical factory in Syria stockpiles hydroxychloroquine. Researchers do not yet know whether it works against COVID-19.Credit: Louai Beshara/AFP/Getty
Researchers have rallied in unprecedented ways to defeat the coronavirus pandemic. They are retooling laboratories to focus on the virus; helping with testing efforts; and, in the case of clinician–researchers, working feverishly to carry out research studies while also treating patients in overwhelmed health-care systems.
Some clinical trials — such as the World Health Organization’s Solidarity trial of four potential COVID-19 therapies — are large and collaborative. They involve teams working together across many sites to test drug candidates against COVID-19. However, in the urgency to find treatments, other trials are smaller, do not always include a control group and don’t test medicines on enough patients to provide statistically meaningful results.
In the midst of a pandemic, there is a place for such initial exploration of potential treatments for those who are seriously ill. They can be quick to organize and do not need extensive resources — allowing clinicians in smaller hospitals and those with lower budgets to conduct research. But, in the end, the search for a successful drug needs the power of scale and the learning that comes from collaboration. More trials must, moreover, include control groups and ensure transparency with data.
Coronavirus and COVID-19: Keep up to date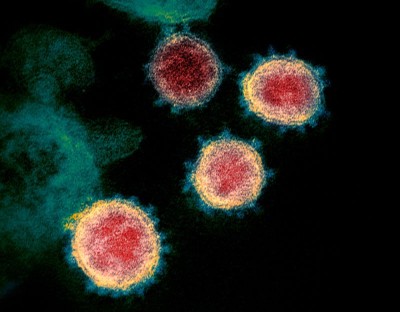
Studies of the experimental antiviral drug remdesivir provide an example of the clinical chaos that can ensue when trials are not well designed. Remdesivir is widely considered to be among the best candidates for a drug against SARS-CoV-2, the virus that causes COVID-19. Over the past four months, a series of studies have been launched to investigate remdesivir’s effectiveness against COVID-19, but they have produced conflicting results.
Hopes were first raised by an early analysis of 53 people seriously ill with COVID-19 in the United States, Europe, Canada and Japan who were given remdesivir. Sixty-eight per cent showed a clinical improvement when given the drug (J. Grein et al. N. Engl. J. Med. http://doi.org/ggrm99; 2020). However, the study lacked a control group and was not an organized clinical trial — instead, it comprised observations of patients who had been given the drug in a last-ditch effort to save their lives.
By contrast, a randomized placebo-controlled trial of remdesivir conducted in China that started with 236 patients with COVID-19 found no significant benefit (Y. Wang et al. Lancet http://doi.org/ggtgvt; 2020). But enrolment in this trial was halted early when the outbreak in China subsided, leaving the trial without enough participants to be able to detect relatively mild effects with statistical rigour.
Hopes rise for coronavirus drug remdesivir
Hopes were also raised when Gilead Sciences in Foster City, California — the company that makes remdesivir and holds the patent — released results on 29 April from a study of 397 people. It reported that patients can be treated as well with a five-day course of the drug as with a ten-day course, but because the study lacked a control group it was impossible to conclude with any certainty whether the drug had worked.
On the same day, the US National Institute of Allergy and Infectious Diseases in Bethesda, Maryland, announced preliminary results from a randomized placebo-controlled trial with 1,063 participants. According to these preliminary results, those who received the drug were discharged from hospital or returned “to normal activity levels” after a median of 11 days in hospital, compared with 15 days for those given a placebo. But the results were announced at a press conference and the full data have not yet been released. So we do not know, for example, how often participants experienced unwanted side effects, or how well matched those in the control and treatment groups were in terms of age and other medical conditions.
Trials and tribulations
Two other medicines — hydroxychloroquine and chloroquine — provide another case study in the pitfalls of small and uncontrolled trials. After early studies in laboratory-grown cells suggested that the drugs might be effective against SARS-CoV-2 (M. Wang et al. Cell Res. 30, 269–271; 2020), clinical trials were launched around the world. But in the wake of multiple trials — many of them small and uncontrolled — researchers still do not have a clear answer as to whether the drugs work against COVID-19 in people. Despite this — and despite their known effects on the heart — world leaders such as US President Donald Trump have fuelled a rush to take these drugs.
There is a different way. The REMAP-CAP study, for example, is a large study testing a variety of treatments against COVID-19, including hydroxychloroquine. It will include participants from more than 160 sites across 14 countries. The study takes advantage of sophisticated clinical-trial designs that allow researchers to add treatment groups to the trial as it is running — and to remove those that preliminary data indicate are not performing well. REMAP-CAP had the benefit of preparation time: it was originally designed to study pneumonia, and has since switched its focus to concentrate on COVID-19.
A pandemic emergency is a reason to work faster, but researchers must not lose sight of the fact that experimental interventions carry an inherent risk to the patient. To balance this risk, clinical trials must be as robustly designed as possible. Some trials need to be small, initial explorations of potential treatments; but, after that, researchers must think big. It’s important to move quickly to larger, collaborative trials — ones that span borders and share expertise — that have a greater chance of showing what really works.

 Coronavirus and COVID-19: Keep up to date
Coronavirus and COVID-19: Keep up to date
 Hopes rise for coronavirus drug remdesivir
Hopes rise for coronavirus drug remdesivir
 Chloroquine hype is derailing the search for coronavirus treatments
Chloroquine hype is derailing the search for coronavirus treatments
 Hundreds of people volunteer to be infected with coronavirus
Hundreds of people volunteer to be infected with coronavirus








