Abstract
Bcl-2 is an anti-apoptotic oncoprotein and its protein levels are inversely correlated with prognosis in many cancers. However, the role of Bcl-2 in the progression of prostate cancer is not clear. Here we report that Bcl-2 is required for the progression of LNCaP prostate cancer cells from an androgen-dependent to an androgen-independent growth stage. The mRNA and protein levels of Bcl-2 are significantly increased in androgen-independent prostate cancer cells. shRNA-mediated gene silencing of Bcl-2 in androgen-independent prostate cancer cells promotes UV-induced apoptosis and suppresses the growth of prostate tumors in vivo. Growing androgen-dependent cells under androgen-deprivation conditions results in formation of androgen-independent colonies; and the transition from androgen-dependent to androgen-independent growth is blocked by ectopic expression of the Bcl-2 antagonist Bax or Bcl-2 shRNA. Thus, our results demonstrate that Bcl-2 is not only critical for the survival of androgen-independent prostate cancer cells, but is also required for the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage.
Similar content being viewed by others
Introduction
Prostate cancer is a frequently diagnosed cancer in men. The growth of prostate cancer is initially androgen-dependent and androgen ablation is a leading therapeutic option for prostate cancer, especially metastatic cancer 1, 2. However, malignant prostate cancer eventually relapses and grows independently of androgen. The molecular mechanism by which androgen-dependent prostate cancer cells acquire the ability to grow under the conditions of androgen-deprivation is poorly understood.
Bcl-2 is an anti-apoptotic oncoprotein, whose oncogenic effects are mediated by preventing cell death, rather than promoting cell proliferation. Increased expression of Bcl-2 contributes to tumorigenicity, poor clinical prognosis and resistance to chemo- and radiation-therapy in many tumors. In vivo administration of antisense Bcl-2 oligodeoxynucleotides in combination with Taxol in castrated mice bearing Shionogi tumors significantly delays the development of androgen-independent, recurrent prostate tumors 3. In humans, androgen-independent prostate cancer cells often express high levels of Bcl-2 4, whereas normal prostatic secretory epithelial cells do not express Bcl-2 proteins 5. Interestingly, the expression level of Bcl-2 protein is significantly increased when prostate cancer progresses from an androgen-dependent to an androgen-independent growth stage 4. However, the role of Bcl-2 in the progression of prostate cancer is unclear.
The human prostate cancer cell line LNCaP is a widely used prostate cancer cell model, as LNCaP cells have functional androgen receptors and depend on androgen for proliferation 6. In addition, withdrawal of androgen induces the transition of LNCaP cells from an androgen-dependent to an androgen-independent growth stage 6. Various sublines of LNCaP cells have been derived from the original LNCaP cells [7, 8, 9], including androgen-dependent LNCaP 104-S, androgen-independent 104-R1, 104-R2, and CDXR cells, all of which have similar genetic background 6. These cell lines provide a useful model for studying the molecular mechanism(s) underlying the progression of prostate cancer. Using the LNCaP 104 cell model system, we investigated the role of the anti-apoptotic protein Bcl-2 in the transition of prostate cancer from an androgen-dependent to an androgen-independent growth stage. We found that Bcl-2 is required for the survival of androgen-independent 104-R cells but not for androgen-dependent 104-S cells. More importantly, Bcl-2 plays a critical role in the transition of androgen-dependent 104-S cells to androgen-independent 104-R1 cells. Thus, our results reveal a novel role of Bcl-2 in regulating the progression of prostate cancer.
Materials and Methods
Cell culture
Human prostate cancer cell LNCaP sublines 104-S, 104-R1, 104-R2, and CDXR were generated and maintained as described previously 6, 10. Androgen-dependent 104-S cells were grown in DMEM with 10% fetal bovine serum (FBS), supplemented with 1 nM DHT (5α-dihydrotestosterone). Androgen-independent 104-R1, 104-R2, and CDXR cells were cultured in DMEM with 10% dextran-coated charcoal-stripped fetal bovine serum (CS-FBS) 6.
Androgen-deprivation progression colony assay
The assay for the progression of androgen-dependent 104-S cells to androgen-independent Casodex-resistant CDXR cells has been described previously 10. The same method was used to analyze the growth of androgen-independent colonies. Briefly, cells were cultured in DMEM supplemented with 10% CS-FBS and 5 μM anti-androgen Casodex (Cdx) 11. Cell cultures were maintained for 4 to 6 weeks and the medium was changed every three days. Floating cells were washed away and attached cells and/or colonies were counted in duplicated plates.
Cell death assay
Apoptotic cell death was determined by staining nuclei with Hoechst 33258, followed by visualization by UV microscopy and quantification by counting condensed and fragmented nuclei in five randomly selected areas, as described previously 12. Caspase activity assays were carried out by using the fluorogenic caspase-3 substrates (DEVE-AFC), as described previously 12.
Immunoblotting analysis
Cells were lysed in buffer containing 50 mM Tris-HCl (pH 7.4), 2 mM MgCl2, 145 mM NaCl, 2 mM EGTA, 0.25% Nonidet P-40 (NP-40), 1 mM DTT, and a cocktail of protease inhibitors (2 mM PMSF, 5 μg/ml leupeptin, 5 μg/ml aprotinin). After removal of cell debris by centrifugation, equal amounts of proteins were separated by SDS-PAGE, transferred onto PVDF membrane, and analyzed by immunoblotting using antibodies against Bcl-2 (Pharmingen), Mcl-1 (Santa Cruz), Bax (Santa Cruz), and β-actin (Chemicon). The immune complexes were detected with appropriate secondary antibodies and chemiluminescence reagents (Pierce).
Generation of shRNA stable cell lines and IPTG-inducible Bax expression cell lines
To generate Bcl-2 shRNA stable 104-S and 104-R cell lines, complementary oligonucleotides corresponding to the 64-base short-hairpin RNA containing a 19-base Bcl-2 sequence in inverted repeat orientation were synthesized (Integrated DNA Technologies, Inc.). After annealing, the 64-mer duplex was inserted into BglII/HindIII-digested pH1RP RNAi expression vector 13. Two shRNA constructs were generated according to Bcl-2 open reading frame at position 31 (5′-CCG GGA GAT AGT GAT GAA G-3′) and 64 (5′-GCT GTC GCA GAG GGC TAC-3′). After transfecting LNCaP 104-R1 cells with a mixture of both shRNA constructs, G418-resistant colonies were selected and clones were screened for reduced Bcl-2 expression by immunoblotting analysis using anti-Bcl-2 antibody. For 104-S/Bcl-2 shRNA cells, the G418 resistant colonies were selected and screened for shRNA levels by real-time Quantitative PCR, since the Bcl-2 protein level in 104-S cells was too low to be detected by immunoblotting. The 5′ end of the probe was labeled with reporter-fluorescent dye FAM. The 3′ end of the probe was labeled with quencher dye TAMRA. The forward and reverse PCR primers were 5′-TGG CTG TGA GGG ACA GGG-3′ and 5′-GAT TTT CCC AGA ACA CAT AGC GAC-3′ respectively. To generate IPTG (Isopropyl β-D-1-thiogalactopyranoside)-inducible Bax expression cell lines, HA-tagged Bax was cloned into the LNXR02 vector 14. After co-transfection with lac-repressor-expressing vector p3'SS (Stratagene), the cells were selected with G418 for 3 weeks, the G418 resistant colonies were expanded, and expression of Bax proteins were induced by addition of 1 mM IPTG for 24 h. HA-Bax protein levels were detected by immunoblotting with anti-HA antibody.
Tumorigenic analysis in mice
In vivo experiments involving mice were approved by the University of Chicago Institutional Animal Care and Use Committee. Eight week-old male BALB/c nu / nu mice (National Cancer Institute, Frederick, MD) were subcutaneously injected in both flanks with 1 ×106 104-R1/vector or 104-R1/Bcl-2 shRNA cells suspended in 0.2 ml Matrigel (BD Biosciences) 14 d after castration. Tumor volumes were recorded every week using calipers and volume was calculated using the formula: volume = length × width × height × 0.52 15. Statistical analysis was done using a two-tailed paired Student's t test.
Results
Upregulation of Bcl-2 protein levels during the progression of androgen-dependent LNCaP cells to androgen-independent LNCaP cells.
While the growth of LNCaP 104-S cells depends on androgen, they can be “converted” to androgen-independent 104-R1 cells, after long-term androgen deprivation in vitro (Figure 1A) 6, 16. 104-R1 cells can further progress to 104-R2 cells, whose growth can even be suppressed by androgen 6, 16. The whole process takes about two years under the conditions of androgen-deprivation 6. However, androgen-independent LNCaP cells can also be generated in a few weeks after culturing 104-S cells under the conditions of androgen-deprivation plus treatment with anti-androgen Casodex (Cdx) 11. The resultant cells can be further cultured into a stable cell line, termed CDXR (Casodex-resistant cells) 6 (Figure 1A). The progression of 104-S cells to 104-R or CDXR cells closely mimics the progression of prostate cancer in patients who undergo anti-androgen treatment clinically 2, 17.
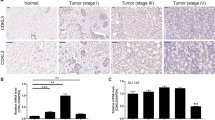
Bcl-2 protein levels are up-regulated in androgen-independent prostate cancer cells. (A) Schematic presentation of the cell model systems for studying the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage. 104-S is androgen-dependent, whereas 104-R and CDXR are androgen-independent LNCaP sublines. (B) Immunoblot analysis of different cell lines using antibodies against Bcl-2, Mcl-1, Bax, and β-actin. 104-R1 and 104-R2 are different stages of 104-R cells; CDXR1 and CDXR2 are two different Casodex-resistant clones. (C) RT-PCR analysis of Bcl-2 mRNA in 104-S and 104-R1 cells. GAPDH was used as internal control.
Using the LNCaP prostate cell model system, we examined the expression profile of Bcl-2 during the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage. Immunoblotting analysis revealed that there was no detectable Bcl-2 in androgen-dependent 104-S cells (Figure 1B). By contrast, Bcl-2 levels dramatically increased in androgen-independent 104-R1, 104-R2 and CDXR cells (Figure 1B). RT-PCR revealed that 104-R1 but not 104-S cells had detectable Bcl-2 mRNA (Figure 1C), suggesting that the up-regulation of Bcl-2 during the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage occurs at the transcription level. This observation is consistent with previous reports that in clinical specimens, Bcl-2 protein levels usually increase in androgen-independent prostate cancer 18. The up-regulation of Bcl-2 proteins is specific, since there were no significant changes in expression levels of other Bcl-2 family proteins, such as anti-apoptotic Mcl-1 and pro-apoptotic Bax (Figure 1B). These results suggest that in the absence of androgen, which is a major survival factor for androgen-dependent prostate cancer cells, Bcl-2 may become a major survival factor for androgen-independent prostate cancer cells.
Bcl-2 is required for the survival of androgen-independent prostate cancer cells
To determine whether Bcl-2 substitutes for androgen as a survival factor in androgen-independent prostate cancer cells, 104-R1 cells were stably transfected with pH1RP vector expressing shRNA of Bcl-2 (104-R1/Bcl-2 shRNA) or empty pH1RP vector (104-R1/vector). Immunoblotting analysis revealed that Bcl-2 protein levels were significantly reduced in several clones stably transfected with Bcl-2 shRNA (Figure 2A). shRNA-mediated knockdown of Bcl-2 proteins did not affect the growth properties of these stable clones (data not shown).
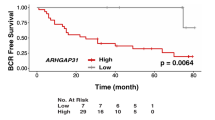
Bcl-2 is a survival factor for androgen-independent prostate cancer cells in vitro and in vivo. (A) Immunoblot analysis of Bcl-2 protein levels in 104-R1 cells stably transfected with either Bcl-2 shRNA (104-R1/Bcl-2 shRNA, four individual clones were shown) or the control empty vector (104-R1/vector). (B) Caspase assays of 104-R1/Bcl-2 shRNA or 104-R1/vector treated with UV irradiation (10 mJ/cm2). (C) Tumor formation in castrated adult male mice subcutaneously injected with human prostate cancer cells 104-R1/Bcl-2 shRNA or 104-R1/vector. Data represent the average volume of 8 tumors.
To test whether knockdown of Bcl-2 sensitizes the cells to apoptotic stimuli, 104-R1/Bcl-2 shRNA and the control 104-R1/vector cells were treated with UV (10 mJ/cm2) and then incubated for 15 h. Apoptotic cell death assays showed that 104-R1/Bcl-2 shRNA cells were much more sensitive to UV-induced apoptosis than the control, as measured by caspase 3 assays (Figure 2B). In contrast, knockdown of Bcl-2 did not affect the sensitivity of androgen-dependent 104-S cells to UV-induced apoptosis (data not shown).
To determine whether Bcl-2 regulates the tumorigenicity of 104-R1 cells in vivo, castrated male mice were subcutaneously injected with 104-R1/Bcl-2 shRNA or 104-R1/vector cells. Tumor number (frequency) and size (volume) were monitored weekly. Interestingly, the ability of 104-R1/Bcl-2 shRNA cells to form tumors (frequency) was not significantly affected by knockdown of Bcl-2 (data not shown), whereas knockdown of Bcl-2 significantly suppressed the growth of the tumor when compared to the control groups, as measured by tumor volume (Figure 2C). These results show that Bcl-2 is required for overriding the growth barrier caused by androgen withdrawal.
Ectopic expression of the Blc-2 antagonist Bax suppresses the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage
The pro-apoptotic Bcl-2 family protein Bax antagonizes the pro-survival function of Bcl-2 by forming the Bax/Bcl-2 heterodimer 19. The ratio of Bcl-2:Bax and level of free Bcl-2 is critical for cell survival 20. Androgen-dependent 104-S cells express little or no Bcl-2 and depend on androgen for survival. Androgen-independent 104-R1 cells depend on Bcl-2 for survival, therefore, an increase in the ratio of Bax/Bcl-2 should significantly affect the survival of 104-R1 cells but not 104-S cells. To test this scenario, we established 104-S cells stably expressing an IPTG-inducible HA-Bax. Immunoblotting analysis revealed that addition of IPTG significantly induced expression of HA-Bax in the 104-S HA-Bax cells (Figure 3A). In the absence of IPTG, there was low level expression of HA-Bax (Figure 3A), most likely due to the leakage of the IPTG expression system. This low level expression of HA-Bax did not affect the growth of 104-S cells in the presence of androgen (data not shown). In contrast, we were unable to obtain any colonies of 104-R1 cells under the same condition (data not shown), suggesting that 104-R1 cells are more sensitive to the anti-Bcl-2, pro-apoptotic protein Bax. This suggests that an increase in the ratio of Bax:Bcl-2 suppresses the growth of androgen-independent 104-R1 cells.
Ectopic expression of the Bcl-2 antagonist Bax inhibits the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage. (A) IPTG-inducible expression of HA-Bax. 104-S cells were stably transfected with an IPTG-inducible expression vector encoding HA-tagged Bax or the empty vector. Expression of HA-Bax was induced by the addition of IPTG (1 mM) for 24 h and HA-Bax proteins were detected by immunoblotting using anti-HA antibody. (B) Androgen-deprivation progression assay. 104-S/IPTG-inducible HA-Bax cells were seeded in 6-well plates in triplicate in regular DMEM medium. After 4 d, the culture medium was switched to androgen-deprivation condition (10% CS-FBS plus 5 μM Casodex). The cell viability was monitored up to 50 d. (C) Tumor formation assays. Castrated adult male mice were subcutaneously injected in both flanks with 104-S cells stably transfected with either the vector for IPTG-inducible HA-Bax or the empty vector. The tumor formation was measured at 12 weeks (8 mice per group).
To determine whether the Bcl-2 antagonist Bax is able to block the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage, 104-S/IPTG-HA-Bax cells were subjected to the androgen-deprivation progression assay. Cells were grown in the presence of androgen for 4 d, followed by androgen-deprivation plus 5 μM of anti-androgen Cdx. The cell viability was monitored over 50 d. The results revealed that 104-S/IPTG-vector cells underwent the crisis stage, but eventually grew back again in the absence of androgen (Figure 3B). Under the same conditions, 104-S/IPTG-HA-Bax cells underwent the “crisis” stage but were unable to grow again in the absence of androgen, with or without further induction of HA-Bax by IPTG (Figure 3B). Consistent with this finding, the tumor formation frequency of 104-S/IPTG-HA-Bax cells in castrated mice was significantly decreased, even in the absence of IPTG (Figure 3C). This suggests that even a low level of HA-Bax protein is sufficient to prevent the progression of androgen-dependent 104-S to androgen-independent cells in vivo.
Expression of Bcl-2 shRNA prevents the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage
Although ectopic expression of HA-Bax changes the ratio of Bax:Bcl-2, which is critical in determining the cell death threshold, Bax may induce cell death independently of Bcl-2 21. It is possible that ectopically expressed Bax may suppress the progression of androgen-dependent 104-S cells to androgen-independent cells independently of its inhibition on Bcl-2. To determine whether Bcl-2 itself is essential for the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage, 104-S cells were stably transfected with expression vectors encoding Bcl-2 shRNA. Since there was no detectable Bcl-2 protein in parental 104-S cells, 104-S/Bcl-2 shRNA stable clones were screened by their expression levels of Bcl-2 shRNA, using quantitative RT-PCR. The effectiveness of Bcl-2 shRNA in 104-S cells was estimated by comparing its expression levels with that in 104-R1/Bcl-2 shRNA cells, in which Bcl-2 shRNA significantly silences Bcl-2 expression (Figure 4A). Androgen-deprivation progression assays revealed that there was an inverse correlation between the expression levels of Bcl-2 shRNA and the formation of androgen-independent colonies. The more Bcl-2 shRNA that was present (Figure 4A), the fewer androgen-independent colonies that were formed (Figure 4B). Interestingly, ectopic expression of Bcl-2 in 104-S cells did not significantly increase androgen-independent colony formation in this assay (data not shown). This is perhaps not surprising, since the oncogenic role of Bcl-2 is to suppress cell death, rather than to promote cell proliferation. It is likely that up-regulation of endogenous Bcl-2 during androgen-deprivation progression is sufficient to suppress cell death and drive the formation of androgen-independent clones.
Ectopic expression of Bcl-2 shRNA in androgen-dependent 104-S cells inhibits their progression into androgen-independent growth stage. (A) The expression levels of Bcl-2 shRNA in 104-S/Bcl-2 shRNA cells (four different stable clones were tested) were measured by Quantitative Real-time PCR. Cells transfected with the empty vector were used as a negative control, whereas 104-R1/Bcl-2 shRNA cells were used as a positive control. (B) 104-S/vector (negative control) and 104-S/Bcl-2 shRNA cells were subjected to androgen-deprivation colony assay. Casodex-resistant colonies were quantified in triplicate.
Taken together, our results demonstrate that Bcl-2 is likely a key survival factor that regulates the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage.
Discussion
Our results suggest that Bcl-2 is required for the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage by substituting for androgen as a survival factor. This conclusion is based on the following evidence.
First, Bcl-2 protein levels were undetectable but were significantly up-regulated when androgen-dependent 104-S cells progressed to androgen-independent 104-R or CDXR cells (Fig. 1). Second, knockdown of Bcl-2 in androgen-independent 104-R cells sensitized the cells to apoptotic stimuli and blocked tumor progression in vivo (Figure 2). Third, ectopic expression of the Bcl-2 antagonist Bax suppressed the ability of androgen-dependent 104-S cells to grow under the conditions of androgen-deprivation and to form tumors in castrated mice (Figure 3). Finally, “pre-loading” of Bcl-2 shRNA in androgen-dependent 104-S cells blocked their transition to an androgen-independent growth stage (Figure 4). These results demonstrate that Bcl-2 is required for the progression of prostate cancer.
It has been reported that under the conditions of androgen deprivation, most of androgen-dependent 104-S cells undergo cell cycle arrest and eventually die during a “crisis” stage 22. The molecular mechanism by which the surviving androgen-dependent cells grow again in an androgen-independent manner has been controversial. It has been proposed that there is a “transition” stage, in which molecular changes convert the cells from androgen-dependent to androgen-independent growth. However, it has also been hypothesized that the growth of a small pre-existing population of androgen-independent cells among androgen-dependent cells is selected during androgen deprivation. Determination of the expression levels of Bcl-2 proteins in single prostate cancer cells may provide an answer to the controversy. Nevertheless, it is clear that Bcl-2 plays a critical role in regulation of the progression of prostate cancer from androgen-dependent to androgen-independent growth. Inactivation of Bcl-2 in androgen-dependent prostate cancer may be useful in combination with anti-androgen therapy to prevent the relapse of prostate cancer after anti-androgen therapy.
References
Huggins C, Hodges CV . Studies on prostatic cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. J Urol 1941; 168:9–12.
Miyamoto H, Messing EM, Chang C . Androgen deprivation therapy for prostate cancer: current status and future prospects. Prostate 2004; 61:332–353.
Gleave ME, Miayake H, Goldie J, Nelson C, Tolcher A . Targeting bcl-2 gene to delay androgen-independent progression and enhance chemosensitivity in prostate cancer using antisense bcl-2 oligodeoxynucleotides. Urology 1999; 54:36–46.
McDonnell TJ, Troncoso P, Brisbay SM, Logothetis C, Chung LW, Hsieh JT, Tu SM, Campbell ML . Expression of the protooncogene bcl-2 in the prostate and its association with emergence of androgen-independent prostate cancer. Cancer Res. 1992; 52:6940–6944.
Colombel M, Symmans F, Gil S, et al. Detection of the apoptosis-suppressing oncoprotein bc1-2 in hormone-refractory human prostate cancers. Am J Pathol 1993; 143:390–400.
Kokontis JM, Hay N, Liao S . Progression of LNCaP prostate tumor cells during androgen deprivation: hormone-independent growth, repression of proliferation by androgen, and role for p27Kip1 in androgen-induced cell cycle arrest. Mol Endocrinol 1998; 12:941–953.
van Steenbrugge GJ, van Uffelen CJ, Bolt J, Schroder FH, The human prostatic cancer cell line LNCaP and its derived sublines: an in vitro model for the study of androgen sensitivity. J Steroid Biochem Mol Biol 1991; 40:207–214.
Wu HC, Hsieh JT, Gleave ME, Brown NM, Pathak S, Chung LW . Derivation of androgen-independent human LNCaP prostatic cancer cell sublines: role of bone stromal cells. Int J Cancer 1994; 57:406–412.
Joly-Pharaboz MO, Soave MC, Nicolas B, Mebarki F, Renaud M, Foury O, Morel Y, Andre JG . Androgens inhibit the proliferation of a variant of the human prostate cancer cell line LNCaP. J Steroid Biochem Mol Biol 1995; 55:67–76.
Kokontis JM, Hsu S, Chuu CP, et al. Role of androgen receptor in the progression of human prostate tumor cells to androgen independence and insensitivity. Prostate. 2005; 65:287–298.
Waller AS, Sharrard RM, Berthon P, Maitland NJ . Androgen receptor localisation and turnover in human prostate epithelium treated with the antiandrogen, casodex. J Mol Endocrinol 2000; 24:339–351.
Xiang J, Chao DT, Korsmeyer SJ . BAX-induced cell death may not require interleukin 1 beta-converting enzyme-like proteases. Proc Natl Acad Sci U S A 1996; 93:14559–14563.
Fukuchi J, Hiipakka RA, Kokontis JM, et al. Androgenic suppression of ATP-binding cassette transporter A1 expression in LNCaP human prostate cancer cells. Cancer Res. 2004; 64:7682–7685.
Chang BD, Roninson IB . Inducible retroviral vectors regulated by lac repressor in mammalian cells. Gene 1996; 183:137–142.
Pretlow TG, Delmoro CM, Dilley GG, Spadafora CG, Pretlow TP . Transplantation of human prostatic carcinoma into nude mice in Matrigel. Cancer Res 1991; 51:3814–3817.
Kokontis J, Takakura K, Hay N, Liao S . Increased androgen receptor activity and altered c-myc expression in prostate cancer cells after long-term androgen deprivation. Cancer Res 1994; 54:1566–1573.
Hurtado-Coll A, Goldenberg SL, Gleave ME, Klotz L . Intermittent androgen suppression in prostate cancer: the Canadian experience. Urology 2002; 60:52–56; discussion 56.
Catz SD, Johnson JL . BCL-2 in prostate cancer: a minireview. Apoptosis 2003; 8:29–37.
Korsmeyer SJ, Shutter JR, Veis DJ, Merry DE, Oltvai ZN . Bcl-2/Bax: a rheostat that regulates an anti-oxidant pathway and cell death. Semin Cancer Biol 1993; 4:327–332.
Korsmeyer SJ Bcl-2: an antidote to programmed cell death. Cancer Surv 1992; 15:105–118.
Knudson CM, Korsmeyer SJ . Bcl-2 and Bax function independently to regulate cell death. Nat Genet 1997; 16:358–363.
Denmeade SR, Lin XS, Isaacs JT . Role of programmed (apoptotic) cell death during the progression and therapy for prostate cancer. Prostate 1996; 28:251–265.
Acknowledgements
This work was partially supported by NIH K01 award CA090516 and the Funding from Illinois Institute of Technology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, Y., Fukuchi, J., Hiipakka, R. et al. Up-regulation of Bcl-2 is required for the progression of prostate cancer cells from an androgen-dependent to an androgen-independent growth stage. Cell Res 17, 531–536 (2007). https://doi.org/10.1038/cr.2007.12
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cr.2007.12
Keywords
This article is cited by
-
CRISPR/Cas9-mediated deletion of Interleukin-30 suppresses IGF1 and CXCL5 and boosts SOCS3 reducing prostate cancer growth and mortality
Journal of Hematology & Oncology (2022)
-
Combination treatment of docetaxel with caffeic acid phenethyl ester suppresses the survival and the proliferation of docetaxel-resistant prostate cancer cells via induction of apoptosis and metabolism interference
Journal of Biomedical Science (2022)
-
Pharmacological inhibition of androgen receptor expression induces cell death in prostate cancer cells
Cellular and Molecular Life Sciences (2020)
-
FAM3B/PANDER inhibits cell death and increases prostate tumor growth by modulating the expression of Bcl-2 and Bcl-XL cell survival genes
BMC Cancer (2018)
-
A common effect of angiotensin II and relaxin 2 on the PNT1A normal prostate epithelial cell line
Journal of Physiology and Biochemistry (2016)