Abstract
Vesicular stomatitis virus (VSV) is being developed for cancer therapy. We created a recombinant replicating VSV (rrVSV) that preferentially infected Her2/neu expressing breast cancer cells. We now used this rrVSV to treat macroscopic peritoneal tumor implants of a mouse mammary tumor cell line stably transfected to express Her2/neu. rrVSV therapy alone prolonged survival but did not cure any animals. rrVSV therapy combined with antibody to TGFb or antibody to IL-10 receptor (IL-10R) each produced cure in one of six animals. Strikingly, rrVSV therapy combined with anti-CTLA4 monoclonal antibody (MAb) produced cure in four of five animals. Anti-CTLA4 MAb was only effective when administered within one day of rrVSV therapy. Cure required CD4 T-cells early (<7 days) and late (>7 days) after rrVSV therapy whereas CD8 T-cells were required only late (>7 days) after rrVSV therapy. Surviving animals were resistant to re-challenge with D2F2/E2 suggesting a memory immune response. Histopathologic analysis demonstrated a dense inflammatory infiltrate of tumor nodules within days of therapy and foamy histiocytes replacing the tumor nodules 2 weeks following therapy. These studies demonstrate that targeted rrVSV combined with anti-CTLA4 MAb can eliminate established macroscopic tumor implants by eliciting an anti-tumor CD4 and CD8 T-cell immunologic response.
Similar content being viewed by others
Introduction
Viruses and viral vectors are being designed for cancer therapy.1 Studies are ongoing using adenovirus,2, 3 herpes simplex virus,4 reovirus,5 Newcastle disease virus,6 vaccinia virus,7 poliovirus,8 VSV and measles virus.9, 10 Efficacy and safety are the crucial issues. VSV is an excellent candidate for development as an oncolytic virus because it is an efficient cell killer that does not produce serious human disease.11 Normal tissues are protected from the virus by IFN production but most human tumors are insensitive to the effects of IFN and susceptible to killing by VSV.12, 13 Therapeutic effects in animal models have been observed using wt VSV, VSV modified with cytokines and VSV in combination with chemotherapy.14, 15, 16, 17 A theoretic safety concern is whether the virus will be tolerated by cancer patients who are immunologically compromised. Several approaches to address this issue are being developed such as creating an rVSV expressing IFNβ,13 creating a VSV M-protein mutant that induced 20–50 times more IFNα than wt VSV or administering IFN systemically during VSV infection.12 We are attempting to improve the therapeutic index of VSV by restricting binding and infection to cancer cells. We have previously created a recombinant replicating VSV (rrVSV) with an altered surface glycoprotein (gp) that targeted preferentially to breast cancer cells. The key change was replacing the native G gp gene in VSV with a modified gp gene from Sindbis Virus (SV).18 The surface gp of Sindbis consists of an E1 fusion protein and an E2 binding protein. Deletion of amino acids 72 and 73 within E2 reduces binding and infectivity of the virus >90%.18 Others had shown that targeted Sindbis Virus and retroviral vectors could be created by placing an Fc-binding domain of protein A within this site and adding exogenous antibody.19, 20 We placed a gene segment coding for a single-chain antibody (SCA) domain in this site within the E2 protein.21 The SCA domain recognizes the Her2/neu receptor, erbb2, that is overexpressed on many breast cancer cells and expressed little or not at all on normal cells. The viral genome was also modified by the inclusion of genes expressing mouse GM-CSF and green fluorescent protein. We showed that this rrVSV selectively infected, replicated and killed cells expressing erbb2.21, 22 rrVSV therapy was able to eliminate 1-day-old microscopic peritoneal tumor implants of D2F2/E2 cells, a BALB/c mouse mammary tumor cell line which was stably transfected to express Her2/neu.23 We now attempted to treat macroscopic nodules of compact tumor because the structural and immunological challenges preventing successful therapy are fundamentally greater than those posed by small loose collections of tumor cells.24, 25 Immune modifiers in addition to rrVSV were required to achieve cure of tumor.
Materials and methods
Cells, antibodies, chemicals and animals
D2F2/E2 cells, a mouse mammary tumor line that has been stably transfected with a vector expressing the human Her2/neu gene and its parent cell line, D2F2 were a generous gift from Dr Wei-Zen Wei, Karmanos Cancer Institute, Wayne State University, Detroit, MI. A comparison of Her2/neu expression in these cell lines with a highly overexpressing Her2/neu human breast cancer cell line, SKBR3, showed that the mean fluorescence on cells stained with the humanized anti-erbb2 monoclonal antibody Herceptin was 401 on SKBR3 cells, 186 on D2F2/E2 cells and 12 on D2F2 cells.21 Absence of mycoplasma contamination in cell lines was confirmed by the MycoAlert Mycoplasma Detection Kit (Cambrex Bioscience, Rockland ME). Anti-CD8 (2.43)26 and anti-CD4 (GK1.5)27 ascites were prepared from hybridomas obtained from the American Type Culture Collection (Rockville, MD). Anti-CTLA4 (9H10)28 ascites was prepared from a hybridoma generously supplied by Dr James P Allison, Memorial Sloan Kettering Cancer Center, New York, NY. Anti-TGFβ MAb was generously supplied by Dr Ellen Filvaroff and Genentech Inc. (South San Francisco, CA).29 Purified anti-mouse CD210 (IL-10R) MAb, Clone 1B1.3a, was purchased from Biolegend (San Diego, CA). CpG, ODN 1668 with phosphorothioate bonds (5-T*C*C*A*G*G*A*C*G*G*T*C*C*T*G*A*T*G*C*T-3), was purchased from IDT (Integrated DNA Technologies, Coralville, IA) and diluted in sterile 0.9% NaCl to a concentration of 1 mg ml−1. All animal studies were conducted using female BALB/c mice, 6–20 weeks of age, weighing 12–20 g, obtained from the National Cancer Institute (Frederick, MD). These animal studies were approved by the Institutional Animal Research and Care Committee.
Depletion in vivo of T-cells
CD8+ T cells were depleted using the 2.43 antibody, and CD4+ T cells were depleted using the GK1.5 antibody by administering 0.1 mg of ascites antibody IP daily for 3 days and then 0.3 mg two times per week.23 Ascites was estimated to contain 3 mg ml−1 of MAb protein. Depletion was >90% as verified in control BALB/c mice by flow cytometric analysis of spleen cells.
rrVSV
rrVSV targeted to cells expressing Her2/neu was created from vector components as previously described.21 In brief, vectors expressing the VSV genome and the individual VSV genes P, L, N and G (pBS-P, L, N and G respectively) on a T7 promoter were a very generous gift of Dr John K Rose, Yale University School of Medicine. Vectors expressing Sindbis glycoprotein (gp) and Sindbis gp modified between amino acids 71 and 74 to express two IgG-binding domains (Sindbis-ZZ) were generously supplied by Dr Irvin SY Chen, University of California, Los Angeles Medical School. A vector expressing a SCA based on the 4D5 anti-erbb2 antibody was a generous gift by Genentech Inc. As previously described, we used PCR to create a chimeric Sindbis gp which consisted of the first 71 amino acids of the Sindbis E2 gp followed in order by a poly-glycine linker, SCA to erbb2, CH1 linker, the remainder of the E2 gp and the entire E1 Sindbis gp.23 The gene for the native VSV-G gp was removed from the VSV genome and replaced with a gene coding for the chimeric Sindbis gp. In addition, genes coding for enhanced green fluorescent protein and mouse GM-CSF were added to the VSV genome producing a genome of 14 838 bases. Replicating recombinant VSV was created using standard techniques21, 30 that expressed only the chimeric Sindbis gp on its surface and also expressed enhanced green fluorescent protein and GM-CSF. This rrVSV was then adapted to grow well on D2F2/E2 cells by serial passage in vitro on this cell line.31 rrVSV for animal trials was made by infecting D2F2/E2 cells at a multiplicity of infection (MOI)=0.001 in 168 cm2 tissue culture flask (Corning/CoStar, Corning, NY) and harvesting supernatant 48 h later. Titers of rrVSV in the supernatant were typically 1–3 × 108 ml−1 on D2F2/E2 cells assayed by counting green cells as previously described.21 Conditioned media was obtained from uninfected D2F2/E2 cells. Inactivated virus was made by exposing rrVSV to UV irradiation from a Phillips TUV36T5 SP Ultraviolet bulb at 30 cm for 5 min. Absence of active virus was confirmed by titering.
Treatment trials
Female BALB/c mice were implanted intraperitoneally (i.p.) with 2 × 106 D2F2/E2 cells in 500 μl PBS. All rrVSV and antibody treatments were administered i.p. Animals were assessed three times per week for ascites and signs of poor health such as low activity, poor grooming, rough coat, hunched posture and dehydration, and weighed once per week. They were killed when they developed ascites. The mesentery, omentum and retroperitoneal tissues were harvested in a single bloc, fixed in 10% formalin and embedded in paraffin for histopathologic analysis. Photomicrographs were imaged with an Olympus SC 35 camera attached to an OM phototube (magnification × 10) and connected to an Olympus BH-2 microscope with Olympus objectives of × 2, × 4, × 10, × 20 and × 40. Statistical analysis was performed using the log rank statistic to compare survival among the treatment groups. The animals were considered cured if they survived for 100 days after tumor implantation because we did not have any animals that developed recurrences after this time.
Results
We had previously demonstrated that rrVSV therapy was able to eliminate 1-day-old microscopic peritoneal tumor implants of D2F2/E2 cells and elicit an anti-tumor T-cell immunologic response. We wanted to extend our results with 1-day tumors to more established, clinically relevant, tumors. There was a limited window of time to begin therapy because mice began to die from peritoneal tumors as early as 14 days after implantation.23 We chose to treat 3 days following implantation because by this time the tumors were macroscopically visible solid established collections of compact tumor cells.
In-vivo therapeutic trials using rrVSV
D2F2/E2, a BALB/c mouse breast cancer cell line stably transfected to express the Her2/neu receptor, was implanted into the peritoneum of BALB/c mice. Histopathologic examination of the mesentery 3 days after implantation showed multiple established tumor nodules 1–2 mm in size. Treatment of 3-day tumors with rrVSV at 1 × 108 ID i.p., a dose which showed therapeutic efficacy against 1-day tumors, was not significantly effective (median survival 26 days in the rrVSV-treated group and 20 days in the controls; n=10 for each group; log rank statistic P=0.3543). Tumors were then treated with higher doses of rrVSV to see if this would compensate for larger tumor size. Treatment with rrVSV at 1 × 109 ID (log rank statistic P=0.0025) or 3 × 108 ID for three doses (log rank statistic P=0.0015) produced significantly prolonged survival, from 20 to 32 days in both cases, but no cures (Figures 1 and 2). Treatment with rrVSV at 1 × 109 ID for two doses produced no additional benefit. It was clear that larger doses of rrVSV could not compensate for increased tumor size. Solid tumor nodules were structurally and immunologically different from small collections of tumor cells and could not be eradicated by rrVSV alone.
Survival curves of D2F2/E2 implants treated with replicating VSV (rrVSV). Three-day-old peritoneal D2F2/E2 implants were treated IP with either rrVSV, 1 × 109 ID or conditioned media. Median survival was 32 days for the rrVSV-treated group and 20 days for the controls; n=5 for each group; log rank statistic P=0.0025.
Survival curves of D2F2/E2 implants treated with replicating VSV (rrVSV). Three-day-old peritoneal D2F2/E2 implants were treated IP with either rrVSV, 3 × 108 ID on days 3, 5 and 7 following tumor implantation or conditioned media. Median survival was 32 days for the rrVSV-treated group and 20 days for the controls; n=5 for each group; log rank statistic P=0.0015.
rrVSV treatment combined with either anti-IL-10R or anti-TGFβ antibody
Our previous work showed that rrVSV therapy elicited an anti-tumor T-cell response23 and we therefore attempted to augment this response. Recent work32 had demonstrated that the combination of the toll-like receptor 9 ligand CpG, anti-IL-10R and an inflammatory reaction could stimulate an immunologic response that eliminated established subcutaneous tumor. We now initiated a therapeutic trial in 3-day tumors that combined treatment with rrVSV, anti-IL-10R antibody and CpG. This combination improved survival from a median of 17.5 days in animals treated with CpG alone to 49 days in animals treated with rrVSV, aIL-10R and CpG (log rank statistic P=0.001) (Figures 3a and b). In addition, we achieved our first cure of these established tumors. The animals were considered cured because they survived for 100 days after tumor implantation and we did not have any animals that developed recurrences after this time. This trial augmented the immune response both by positive and negative stimulation. CpG stimulated a positive inflammatory response. Antibody to IL-10R inhibited the immune dampening effect of IL-10. We decided to concentrate on inhibiting the inhibitors of T-cell activation. rrVSV infection was already creating a pro-inflammatory environment at the tumor site and therefore administering an inflammatory mediator systemically would most likely add little to the local inflammatory response and produce unacceptable systemic side effects. We therefore attempted treatment of 3-day tumors with rrVSV in combination with antibody to TGFβ. This combination also improved survival from a median of 17 days in animals treated with anti-TGFβ alone to 31 days in animals treated with rrVSV and anti-TGFβ (log rank statistic P=0.0082) (Figure 4). One out of six animals receiving combined therapy was cured. Although cures were achieved with these immune modifiers, the low rate was unsatisfactory.
Survival curves of D2F2/E2 implants treated with replicating VSV (rrVSV). Peritoneal D2F2/E2 implants were treated IP with rrVSV, 3 × 108 ID on day 3 and with CpG 5 μg and anti-IL-10R MAb 200 μg on day 4 following tumor implantation and compared with various control treatments as marked. n=6 for each group except CpG alone and aIL-10R alone which had n=4; (log rank statistic P=0.001 comparing full treatment with CpG alone). (a) Full treatment compared with CpG controls. (b) Full treatment compared with anti-IL-10R MAb controls.
Survival curves of D2F2/E2 implants treated with replicating VSV (rrVSV). Peritoneal D2F2/E2 implants were treated IP with rrVSV, 3 × 108 ID on day 3 and with anti-TGFβ MAb 200 μg on day 4 following tumor implantation (n=6) and compared with treatment with anti-TGFβ MAb alone (n=2). Median survival was 31 days for the rrVSV-treated group and 17 days for the controls; log rank statistic P=0.0082.
rrVSV treatment combined with anti-CTLA4 antibody
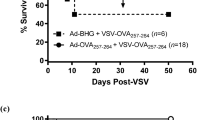
Another option was to inhibit the activity of CTLA4 which is a strong negative regulator of T-cell activation.33 Previous work in animals and humans has shown powerful anti-tumor immunological responses elicited by inhibition of CTLA4.33 The combination of rrVSV therapy with anti-CTLA4 antibody achieved dramatically positive therapeutic effects. Survival was significantly prolonged (log rank statistic P=0.0018 comparing animals treated with aCTLA4 MAb alone to animals treated with rrVSV and aCTLA4 MAb) and cure was achieved in 4 of 5 rrVSV-treated animals (P=0.024, Fisher's exact test) (Figure 5). One rrVSV-treated animal died 49 days after implantation. We predicted that the timing of anti-CTLA4 MAb administration would be critical because CTLA4 expression peaks 48 h after T-cell activation.34 Early administration of anti-CTLA4 MAb would block the inhibitory effect of CTLA4 but late administration after inhibition commenced would have little effect. As expected, administering anti-CTLA4 MAb was most effective 1 day after rrVSV therapy (4 days after tumor implantation), much less effective 3 days after rrVSV therapy and ineffective 7 days after rrVSV therapy (Figure 5).
Survival curves of D2F2/E2 implants treated with replicating VSV (rrVSV). Peritoneal D2F2/E2 implants were treated IP with rrVSV, 3 × 108 ID on day 3 and with anti-CTLA4 MAb 200 μg on various days following tumor implantation and compared with treatment with anti-CTLA4 MAb alone. n=5 for each group; (log rank statistic P=0.0018 comparing animals treated with aCTLA4 MAb alone to animals treated with rrVSV and aCTLA4 MAb on day 4).
Both CD4 and CD8 T-cells are required for therapeutic effect
T-cells are known to be potent therapeutic agents against cancer in humans.35, 36 and T cells were necessary for therapeutic success in our previous 1 day model.23 In those experiments, depletion of both CD4 and CD8 T-cells prior to rrVSV therapy abrogated the therapeutic effect. In the current project, we studied the effects of elimination of either CD4 or CD8 T-cells both before and after rrVSV therapy. We found that both CD4 and CD8 T-cells were necessary to achieve tumor cure but survival was most dramatically reduced by early elimination of CD4 T-cells (Figure 6a). Median survival in animals receiving rrVSV plus anti-CTLA4 MAb and who were depleted of CD4 cells prior to rrVSV was only 23 days whereas median survival in mice depleted of CD8 cells prior to rrVSV was 52 days. We then asked whether late depletion of CD4 or CD8 T-cells affected outcome (Figure 6b). We found that both CD4 and CD8 T-cells were required to cure tumor but the time course of their activity was very different. If a cell type was active early, then having it available early and only depleting it later should have less effect on outcome. In fact, late depletion of CD4 cells 7 days after rrVSV therapy had less effect on outcome than early depletion reinforcing the importance of CD4 cells early in the therapeutic response (median survival of 23 days with early depletion and 35 days with late depletion; P=0.04) (Figure 6b). CD4 T-cells were, however, still required late after rrVSV therapy to achieve tumor cure. Surprisingly, we could not demonstrate that CD8 cells were necessary within 1 week of rrVSV therapy because animals depleted late had the same or worse outcome than those depleted early (median survival of 52 days with early depletion and 45 days with late depletion; P=0.06). CD8 T-cells were required, however, 1 week and more after rrVSV treatment to ensure complete tumor elimination. In summary, CD4 T-cells were necessary early and late for the anti-tumor response but CD8 T-cells were only necessary late.
Survival curves of D2F2/E2 implants treated with replicating VSV (rrVSV). CD4 or CD8 T-cells were depleted either early, prior to tumor implantation or late, after rrVSV therapy. Animals were treated with IP rrVSV, 3 × 108 ID on day 3 following tumor implantation and with anti-CTLA4 MAb 200 μg on day 4. n=5 for each group. (a) Early depletion of T-cells prior to tumor implantation. (b) Late depletion of T-cells 10 days after tumor implantation.
T-cells, however, were not required permanently to protect against tumor recurrence. We simultaneously depleted both CD4 and CD8 T-cells in three long-term survivors to determine whether these animals still harbored tumor cells whose growth was suppressed by the immune system. None of these animals developed tumors indicating that animals surviving for >100 days were truly cured of tumor. Our earlier work had shown that surviving animals challenged with tumor after depleting CD4 and CD8 T-cells rapidly succumbed to massive peritoneal tumor indicating that viable tumor cells would exhibit uncontrolled growth in the absence of T-cells.23
Pathology
Animals were killed 3, 4, 5, 6, 7, 10 and 14 days following tumor implantation. rrVSV was administered on day 3 and anti-CTLA4 MAb on day 4. On day 3, prior to rrVSV therapy, multiple tumor nodules, 1–2 mm in size were evident. On day 4, prior to anti-CTLA4 MAb and 1 day following rrVSV treatment, nodules contained small areas of tumor necrosis with an inflammatory infiltrate of eosinophils and lymphocytes consistent with viral infection (Figures 7a and b). Tumors on days 5 through 10 were heavy infiltrated with inflammatory cells including eosinophils and lymphocytes and showed a mixture of healthy, dead and dying tumor cells (Figure 7c). On day 14, there were fewer tumor nodules. Figures 7d and e shows one large nodule consisted predominantly of lipid laden histiocytes with a small cluster of tumor cells and an inflammatory infiltrate of eosinophils, lymphocytes and macrophages. Control untreated animals showed tumor nodules without inflammatory cells at these same time points.
Histopathological examination of peritoneal tumor nodules at various times after treatment with replicating VSV (rrVSV) showing increasing infiltration with inflammatory cells and finally replacement of tumor with lipid-laden histiocytes. All animals received implants on day 0 and rrVSV treatment on day 3. (a, b) Animal killed on day 4. (c) Animal received anti-CTLA4 MAb on day 4 and was killed on day 10. (d, e) Animal received anti-CTLA4 MAb on day 4 and was killed on day 14. (a) Tumor nodule with central focus of inflammatory cells. H&E × 200. (b) Tumor nodule with lymphocytes infiltrating from blood vessel to the periphery of the tumor. H&E × 400. (c) Tumor nodule diffusely infiltrated with inflammatory cells including lymphocytes and eosinophils. H&E × 200. (d, e) Tumor nodule almost entirely replaced by lipid-laden histiocytes and smaller collections of macrophages, lymphocytes and eosinophils. H&E × 40 and × 200, respectively.
Re-challenge of survivors with D2F2/E2 tumor
To determine whether surviving animals had developed anti-tumor immunity, five long-term survivors of D2F2/E2 implantation who had been treated with rrVSV and aCTLA4 MAb were re-challenged with D2F2/E2 cells. These mice did not receive any therapy. All survived >100 days indicating the presence of immunity to this tumor cell line. It was important to determine whether this was immunity only to the foreign Her2/neu receptor protein, which had been introduced into the D2F2/E2 cells or whether the immunity extended to the parent D2F2 cells. Three of these animals were then challenged with D2F2 cells. One animal died 34 days after challenge with uncontrolled tumor growth in the peritoneum. Two never developed tumor thereby demonstrating that rrVSV therapy had resulted in immunity to the fully syngeneic D2F2 cells.
Discussion
Oncolytic viruses are being explored as a therapy for cancer because they offer a potential cure using a treatment with greater potency and less toxicity than chemotherapy or radiation. Viruses can be targeted such that they selectively infect or replicate only in tumor cells, and will not affect all dividing cells in the body like conventional chemotherapy. Targeted viral therapy is unique among biologic and chemotherapies in having the ability to multiply exponentially at the site of the tumor until controlled by the natural host defenses. Oncolytic virus may attack the tumor both directly and indirectly. The targeted virus infects and kills tumor cells directly. Tumor destruction induced by direct infection is likely to markedly reduce tumor burden especially in IFN-insensitive tumors. However, it is possible that the more significant function of oncolytic virus is to activate the immune system. Viral lysis of tumor cells releases tumor antigens in the context of an inflammatory response setting the stage for a tumor-specific T cell response that can be therapeutically manipulated and amplified.
We have previously created a recombinant replicating VSV (rrVSV) that targeted preferentially to breast cancer cells and selectively infected, replicated and killed cells expressing erbb2.21, 22 We have concentrated on developing this targeted rrVSV to improve the already excellent safety profile of wild-type VSV. rrVSV therapy was able to eliminate 1-day-old microscopic peritoneal tumor implants.23 However, high dose rrVSV therapy alone could prolong survival but not cure 3-day-old tumor implants because the structural and immunological challenges preventing successful therapy of macroscopic nodules of compact tumor are fundamentally greater than those posed by small loose collections of tumor cells.24, 25 Therefore, in the current study, we added anti-CTLA4 MAb to rrVSV therapy and were able to amplify an antitumor T-cell immunologic response which eliminated established macroscopic tumor implants. In spite of the limitations inherent in any transplantable tumor model, these conclusions are warranted based on the study design and the consistent pattern of the findings. Tumor growth was virulent despite the presence of the human Her2/neu protein and all animals treated with conditioned media died rapidly with a median survival of 20 days (Figure 2). In contrast, animals treated with high doses of rrVSV had significantly prolonged survival. Reproducible, statistically significant, cure, however, was only achieved when anti-CTLA4 MAb was added to rrVSV therapy. The timing of anti-CTLA4 MAb treatment was critical as expected if the effect was dependent on amplifying a T-cell response. CTLA4 expression peaks 48 h after T-cell activation and downregulates activation.34 Predictably therefore, administering anti-CTLA4 MAb 1 day after rrVSV therapy produced a cure in four of five treated animals whereas aCTLA MAb given 3 days after rrVSV therapy resulted in a cure in only one of five treated animals and anti-CTLA4 MAb given 7 days after rrVSV therapy had no benefit (Figure 5). The central importance of CD4 T-cell activation was most convincingly demonstrated in therapeutic trials conducted in animals depleted of CD4 T-cells. All therapeutic benefit of rrVSV or anti-CTLA4 MAb therapy was abrogated (Figure 6). The immune response appears far more important to achieve tumor elimination than the direct oncolytic effect of the virus. Further indirect evidence for an anti-tumor T-cell response comes from studies showing resistance of survivors to re-challenge with tumor. Resistance suggests a memory immune response, which is likely to reside in the T-cells and not B-cells because the antibody response did not differ between treated and control animals (data not shown). We hypothesize that rrVSV-mediated destruction of tumor releases tumor antigens in the context of an inflammatory response. The appropriate costimulatory molecules are induced on dendritic cells, which then initiate an antitumor T-cell response. This response is too weak or too temporary to be therapeutically effective unless it is amplified and prolonged by simultaneous administration of anti-CTLA4 MAb.
This study suggests that CD4 T-cells initiate and direct the antitumor response because CD4 T-cells were required early (<7 days) in the immune response to achieve tumor cure and outcome results were no better than control when CD4 T-cells were eliminated (Figure 6). In contrast, CD8 T-cells were not required until later (>7 days) in the response. These findings fit classic models of immunology in which CD4 T-cells activate and direct the immune response and CD8 T-cells are cytolytic effector cells. CD4 T-cells, however, continue to be required late in the response as multiple cell types remain engaged in the battle for tumor eradication. Histopathologic analysis of tumors 1 week after rrVSV therapy showed the ongoing presence of apparently healthy tumor cells still heavily infiltrated with inflammatory cells including eosinophils and lymphocytes. We postulate that at this stage CD4 T-cells continue to activate an immune response and CD8 cytolytic T-cells are required to find and destroy all remaining tumor cells to achieve a cure. Other potentially cytotoxic inflammatory cells such as macrophages, neutrophils and NK cells are likely to be important in the anti-tumor response but were not explored in this study. By 100 days however, all tumor cells are eradicated because elimination of both CD4 and CD8 T-cells at this time did not result in recurrence of tumor.
Our previous work showed that the duration of rrVSV replication in vivo was 2–3 days23 and the current study demonstrates the requirement for immune stimulation in addition to rrVSV therapy to achieve cure of solid established tumors. In this experimental system, anti-CTLA4 MAb was the most therapeutic immune modifier in addition to GM-CSF, which was produced by the rrVSV. These two potent immune activators have shown clinical efficacy in human trials.33, 37 However, a serious concern regarding the use of anti-CTLA4 MAb in humans is the development of autoimmune colitis. To minimize that danger, it is desirable to target the agent directly to the tumor. Future plans include development of a targeted rrVSV that expresses a secreted single-chain antibody to CTLA4. This will limit the expression of the anti-CTLA4 activity to tumor cells and focus the highest concentration of this immune modifier in the location of the tumor. We have already shown that GMCSF expressed by the rrVSV is only active locally at the tumor site and is not detectable in the blood.23 In the current study, occasional tumor cures were achieved by immune stimulation using antibody to IL-10R or TGFβ. Powerful inhibitors of the immune response are CTLA4, IL-10 and TGFβ, and blocking their action promotes immune activation.38, 39 This method of augmenting the immune response is likely to be more selective and less toxic than using non-specific immune activators such as IL-2 or TNFα because immune stimulation is limited to the site that is receiving inflammatory signals from the targeted virus infection. Our future plans are to test the therapy with rrVSV and anti-CTLA4 MAb in a fully syngeneic tumor model. If anti-CTLA4 MAb provides insufficient immune stimulation in this more stringent model, then we will attempt to further augment immune stimulation by combining current therapy with antibodies to IL-10R and TGFβ. From this study, we cannot conclude that anti-CTLA4 treatment more fundamentally activates a T-cell response than anti-IL-10R or anti-TGFβ treatment because we did not test whether the antibody to CTLA4 more effectively inhibited this molecule than the antibody to TGFβ or the antibody to IL-10R inhibited their antigens.
It is probable that rrVSV therapy will be more potent but not more toxic in humans than mice. rrVSV should persist longer and directly eradicate a greater percentage of tumor following therapy in patients because most human cancers are unresponsive to IFN12 whereas D2F2, the mouse tumor used in the present studies, is IFN responsive (data not shown). VSV infection in the current studies was probably curtailed by IFN production, which is detectable in the blood of rrVSV-treated animals 1 day following rrVSV therapy.23 Toxicity from rrVSV is unlikely because normal human cells and tissues are highly IFN-responsive and do not support a clinically significant VSV infection.13 We have demonstrated in a prior study23 and in this one that rrVSV therapy trains the immune system to recognize and destroy tumor cells. The immune system is then capable of eliminating re-challenges of tumor without further viral therapy. This trained immune system is likely then to be able to find, recognize and eliminate deposits of tumor metastases, which represent the greatest challenge in cancer therapy today.
References
Liu TC, Kirn D, Liu TC, Kirn D . Systemic efficacy with oncolytic virus therapeutics: clinical proof-of-concept and future directions. Cancer Res 2007; 67: 429–432.
Nemunaitis J, Ganly I, Khuri F, Arseneau J, Kuhn J, McCarty T et al. Selective replication and oncolysis in p53 mutant tumors with ONYX-015, an E1B-55kD gene-deleted adenovirus, in patients with advanced head and neck cancer: a phase II trial. Cancer Res 2000; 60: 6359–6366.
Kruyt FA, Curiel DT . Toward a new generation of conditionally replicating adenoviruses: pairing tumor selectivity with maximal oncolysis. Hum Gene Ther 2002; 13: 485–495.
Woo Y, Adusumilli PS, Fong Y . Advances in oncolytic viral therapy. Curr Opin Investig Drugs 2006; 7: 549–559.
Norman KL, Coffey MC, Hirasawa K, Demetrick DJ, Nishikawa SG, DiFrancesco LM et al. Reovirus oncolysis of human breast cancer. Hum Gene Ther 2002; 13: 641–652.
Schirrmacher V, Haas C, Bonifer R, Ahlert T, Gerhards R, Ertel C . Human tumor cell modification by virus infection: an efficient and safe way to produce cancer vaccine with pleiotropic immune stimulatory properties when using Newcastle disease virus. Gene Therapy 1999; 6: 63–73.
Gomella LG, Mastrangelo MJ, McCue PA, Maguire Jr HC, Mulholland SG, Lattime EC . Phase 1 study of intravesical vaccinia virus as a vector for gene therapy of bladder cancer. J Urol 2001; 166: 1291–1295.
Gromeier M, Lachmann S, Rosenfeld MR, Gutin PH, Wimmer E . Intergeneric poliovirus recombinants for the treatment of malignant glioma. Proc Natl Acad Sci USA 2000; 97: 6803–6808.
Hammond AL, Plemper RK, Zhang J, Schneider U, Russell SJ, Cattaneo R . Single-chain antibody displayed on a recombinant measles virus confers entry through the tumor-associated carcinoembryonic antigen. J Virol 2001; 75: 2087–2096.
Schneider U, Bullough F, Vongpunsawad S, Russell SJ, Cattaneo R . Recombinant measles viruses efficiently entering cells through targeted receptors. J Virol 2000; 74: 9928–9936.
de Mattos CA, de Mattos CC, Rupprecht CE . Rhabdoviruses. In: Knipe D, Howley P (eds). Fundamental Virology, 4th edn, Lippincott Williams & Wilkins: Philadelphia, 2001, pp 1245–1277.
Stojdl DF, Lichty B, Knowles S, Marius R, Atkins H, Sonenberg N et al. Exploiting tumor-specific defects in the interferon pathway with a previously unknown oncolytic virus. Nat Med 2000; 6: 821–825.
Obuchi M, Fernandez M, Barber GN . Development of recombinant vesicular stomatitis viruses that exploit defects in host defense to augment specific oncolytic activity. J Virol 2003; 77: 8843–8856.
Fernandez M, Porosnicu M, Markovic D, Barber GN . Genetically engineered vesicular stomatitis virus in gene therapy: application for treatment of malignant disease. J Virol 2002; 76: 895–904.
Diaz RM, Galivo F, Kottke T, Wongthida P, Qiao J, Thompson J et al. Oncolytic immunovirotherapy for melanoma using vesicular stomatitis virus. Cancer Res 2007; 67: 2840–2848.
Porosnicu M, Mian A, Barber GN . The oncolytic effect of recombinant vesicular stomatitis virus is enhanced by expression of the fusion cytosine deaminase/uracil phosphoribosyltransferase suicide gene. Cancer Res 2003; 63: 8366–8376.
Ebert O, Shinozaki K, Huang TG, Savontaus MJ, Garcia-Sastre A, Woo SL . Oncolytic vesicular stomatitis virus for treatment of orthotopic hepatocellular carcinoma in immune-competent rats. Cancer Res 2003; 63: 3605–3611.
Dubuisson J, Rice CM . Sindbis virus attachment: isolation and characterization of mutants with impaired binding to vertebrate cells. J Virol 1993; 67: 3363–3374.
Morizono K, Bristol G, Xie YM, Kung SK, Chen IS . Antibody-directed targeting of retroviral vectors via cell surface antigens. J Virol 2001; 75: 8016–8020.
Ohno K, Sawai K, Iijima Y, Levin B, Meruelo D . Cell-specific targeting of Sindbis virus vectors displaying IgG-binding domains of protein A. Nat Biotechnol 1997; 15: 763–767.
Bergman I, Whitaker-Dowling P, Gao Y, Griffin JA . Preferential targeting of vesicular stomatitis virus to breast cancer cells. Virology 2004; 330: 24–33.
Pilon SA, Kelly C, Wei WZ . Broadening of epitope recognition during immune rejection of ErbB-2-positive tumor prevents growth of ErbB-2-negative tumor. J Immunol 2003; 170: 1202–1208.
Bergman I, Griffin JA, Gao Y, Whitaker-Dowling P . Treatment of implanted mammary tumors with recombinant vesicular stomatitis virus targeted to Her2/neu. Int J Cancer 2007; 121: 425–430.
Stohrer M, Boucher Y, Stangassinger M, Jain RK . Oncotic pressure in solid tumors is elevated. Cancer Res 2000; 60: 4251–4255.
Campoli M, Ferrone S, Zea AH, Rodriguez PC, Ochoa AC . Mechanisms of tumor evasion. Cancer Treat Res 2005; 123: 61–88.
Sarmiento M, Glasebrook AL, Fitch FW . IgG or IgM monoclonal antibodies reactive with different determinants on the molecular complex bearing Lyt 2 antigen block T cell-mediated cytolysis in the absence of complement. J Immunol 1980; 125: 2665–2672.
Dialynas DP, Quan ZS, Wall KA, Pierres A, Quintans J, Loken MR et al. Characterization of the murine T cell surface molecule, designated L3T4, identified by monoclonal antibody GK1.5: similarity of L3T4 to the human Leu-3/T4 molecule. J Immunol 1983; 131: 2445–2451.
Demaria S, Kawashima N, Yang AM, Devitt ML, Babb JS, Allison JP et al. Immune-mediated inhibition of metastases after treatment with local radiation and CTLA-4 blockade in a mouse model of breast cancer. Clin Cancer Res 2005; 11: 728–734.
Carano R, Li Y, Bao M, Li J, Berry L, Ross J et al. Effect of anti-TGF-beta antibodies in syngeneic mouse models of metastasis. J Musculoskelet Neuronal Interact 2004; 4: 377–378.
Lawson ND, Stillman EA, Whitt MA, Rose JK . Recombinant vesicular stomatitis viruses from DNA. Proc Natl Acad Sci USA 1995; 92: 4477–4481.
Gao Y, Whitaker-Dowling P, Watkins SC, Griffin JA, Bergman I . Rapid adaptation of a recombinant vesicular stomatitis virus to a targeted cell line. J Virol 2006; 80: 8603–8612.
Guiducci C, Vicari AP, Sangaletti S, Trinchieri G, Colombo MP . Redirecting in vivo elicited tumor infiltrating macrophages and dendritic cells towards tumor rejection. Cancer Res 2005; 65: 3437–3446.
Korman A, Yellin M, Keler T, Korman A, Yellin M, Keler T . Tumor immunotherapy: preclinical and clinical activity of anti-CTLA4 antibodies. Curr Opin Investig Drugs 2005; 6: 582–591.
Metzler B, Burkhart C, Wraith DC, Metzler B, Burkhart C, Wraith DC . Phenotypic analysis of CTLA-4 and CD28 expression during transient peptide-induced T cell activation in vivo. Int Immunol 1999; 11: 667–675.
Mapara MY, Sykes M, Mapara MY, Sykes M . Tolerance and cancer: mechanisms of tumor evasion and strategies for breaking tolerance. J Clin Oncol 2004; 22: 1136–1151.
Dudley ME, Wunderlich JR, Yang JC, Sherry RM, Topalian SL, Restifo NP et al. Adoptive cell transfer therapy following non-myeloablative but lymphodepleting chemotherapy for the treatment of patients with refractory metastatic melanoma. J Clin Oncol 2005; 23: 2346–2357.
Liu TC, Kirn D, Liu TC, Kirn D . Systemic efficacy with oncolytic virus therapeutics: clinical proof-of-concept and future directions. Cancer Res 2007; 67: 429–432.
Pestka S, Krause CD, Sarkar D, Walter MR, Shi Y, Fisher PB . Interleukin-10 and related cytokines and receptors. Annu Rev Immunol 2004; 22: 929–979.
Letterio JJ, Roberts AB . Regulation of immune responses by TGF-beta. Annu Rev Immunol 1998; 16: 137–161.
Acknowledgements
This study was supported in part by NIH Grant number RO1 CA104404. The contents of this study are solely the responsibility of the authors and do not necessarily represent the official views of the granting institution. We thank Drs Massimo Trucco, William A Rudert and Neal DeLuca for invaluable intellectual and material assistance. Drs Wei-Zen Wei, John K Rose, Irvin SY Chen, Ellen H Filvaroff and Genentech Inc. very generously supplied materials as noted in the text.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gao, Y., Whitaker-Dowling, P., Griffin, J. et al. Recombinant vesicular stomatitis virus targeted to Her2/neu combined with anti-CTLA4 antibody eliminates implanted mammary tumors. Cancer Gene Ther 16, 44–52 (2009). https://doi.org/10.1038/cgt.2008.55
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cgt.2008.55
Keywords
This article is cited by
-
HER2-Positive Breast Cancer Immunotherapy: A Focus on Vaccine Development
Archivum Immunologiae et Therapiae Experimentalis (2020)
-
Cancer DNA vaccines: current preclinical and clinical developments and future perspectives
Journal of Experimental & Clinical Cancer Research (2019)
-
Oncolytic Viruses: Priming Time for Cancer Immunotherapy
BioDrugs (2019)
-
Oncolytic viruses and checkpoint inhibitors: combination therapy in clinical trials
Clinical and Translational Medicine (2018)
-
Recombinant viruses with other anti-cancer therapeutics: a step towards advancement of oncolytic virotherapy
Cancer Gene Therapy (2018)