Abstract
Mesenchymal stem cells (MSCs) have immunomodulatory functions such as the suppression of T and B cells. MSCs suppress immunoglobulin (Ig) production by B cells via cell–cell contact as well as via secretion of soluble factors. Our study showed that the conditioned medium (CM) of MSCs infected with a mycoplasma strain, Mycoplasma arginini, has marked inhibitory effects on Ig production by lipopolysaccharide/interleukin-4-induced B cells compared with mycoplasma-free MSC-CM. We analyzed mycoplasma-infected MSC-CM by fast protein liquid chromatography and liquid chromatography to screen the molecules responsible for Ig inhibition. Complement C3 (C3) was the most critical molecule among the candidates identified. C3 was shown to be involved in the suppression of the Ig production of B cells. C3 was secreted by mycoplasma-infected MSCs, but not by mycoplasma-free MSCs or B cells. It was able to directly inhibit Ig production by B cells. In the presence of a C3 inhibitor, Ig inhibition by MSC-CM was abrogated. This inhibitory effect was concomitant with the downregulation of B-cell-induced maturation protein-1, which is a regulator of the differentiation of antibody-secreting plasma cells. These results suggest that C3 secreted from mycoplasma-infected MSCs has an important role in the immunomodulatory functions of MSCs. However, its role in vivo needs to be explored.
Similar content being viewed by others
Main
Mesenchymal stem cells (MSCs) are adult stem cells that have developmental lineage-restricted differentiation potential. They can differentiate into mesenchymal tissues such as bone, fat, and cartilage and can be isolated from various tissues, including bone marrow, adipose tissue, and umbilical cord.1 Although their differentiation potential is not as great as that of embryonic stem cells or induced pluripotent stem cells, MSCs are considered the most promising candidates for clinical applications.2, 3 A characteristic property of MSCs is their immunomodulatory activity.4 Unlike other pluripotent stem cells, MSCs are not immunogenic when administered in vivo.5 Instead, they can alleviate host immune responses by suppressing inflammation in instances of inflammatory abnormalities. This immunomodulatory or immunosuppressive property of MSCs has accelerated the research and development of their clinical use. In fact, accumulating evidence indicate that MSCs regulate various types of immune cells.6, 7 MSCs inhibit T-cell proliferation, dendritic cell differentiation, and natural killer cell activation, whereas they promote the generation of regulatory T cells.8, 9, 10, 11 In addition, few studies have focused on the effect of MSCs on B cells but the results are contradictory. Some studies reported that MSCs could suppress the activation, proliferation, and differentiation of B cells.12, 13, 14, 15, 16, 17, 18, 19 Other studies showed that MSCs induce B-cell expansion and differentiation.20, 21, 22 Furthermore, most of them reported that soluble factor(s) might have an important role in B-cell immunomodulation. However, the molecular mechanism of how MSCs regulate B cells is not fully understood yet.
Mycoplasmas are very small bacteria lacking cell walls and are the smallest free-living organisms capable of self-replication.23 Mycoplasma contamination tends to be ignored in many laboratories without a stringent quality control. Many researchers fail to notice mycoplasma contamination owing to the absence of visible signs in routine culture.24 As a result, some mycoplasma-contaminated cultures have been used unknowingly in research for years. However, mycoplasmas can affect the key characteristics and functions of cells. For example, mycoplasma-derived macrophage-activating lipoprotein 2 induces inflammatory cytokines in myeloid dendritic cells and macrophages.20 Mycoplasma arginini produces a lipid-associated membrane lipopeptide that is an agonist of toll-like receptor-2/6.25 This lipopeptide regulates the production of several cytokines via nuclear factor-κ B in infected cells.21
Before conducting this study, we had investigated the biological mechanism of MSC-mediated B-cell regulation. Unfortunately, some of our MSC cultures were found to be contaminated with mycoplasmas by our routine quality control program. Interestingly, these MSCs were still found to effectively suppress T and B-cell functions despite the mycoplasma infection. They did not lose their stem cell properties such as differentiation potential and stem cell marker expression. Recently, mycoplasma-contaminated MSCs were reported to enhance the inhibition of T-cell proliferation in vitro.26 Thus, the accidentally detected mycoplasma contamination in our laboratory prompted us to examine whether mycoplasmas affect the MSC-mediated regulation of B-cell functions.
In this study, we showed that a mycoplasma infection allows MSCs to significantly regulate B-cell functions. We demonstrated that MSCs are significantly altered by mycoplasma infection to differentially express various soluble protein factors that are not present in uninfected cells. In particular, complement C3 (C3) was identified as a potent soluble factor responsible for the negative regulation of Ig production in B cells in vitro. Here, we describe our observation and present evidence that mycoplasma contamination has a great influence on MSCs to modulate B-cell functions.
Results
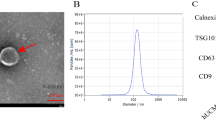
B-cell immunoregulatory activity of MSC-secreted factors was possibly correlated with their mycoplasma infection
It has been suggested that soluble factors secreted from MSCs have an important role in inhibiting antibody-producing B cells.18 Thus, we attempted to evaluate the regulatory activity of conditioned medium (CM) of MSCs (MSC-CM) harvested from our clonal MSCs on the Ig production by B cells. When splenic B cells isolated from Balb/c mice were stimulated with lipopolysaccharide (LPS)/interleukin-4 (IL-4), IgE production was observed (Figure 1a). Co-culture of B cells with MSCs almost completely suppressed IgE production by B cells. Similarly, MSCs suppressed the IgE production in transwell cultures as effective as in co-cultures, suggesting that a soluble factor(s) is responsible for the IgE downregulation. When CM harvested from MSCs normally cultured for 3 days was applied to LPS/IL-4-stimulated B cells, it still potently suppressed IgE production, comparable to co-cultures or transwell cultures. Surprisingly, significant IgE downregulation by MSC-CM was observed even at a dilution of 25 600-fold, suggesting that an unknown powerful B-cell inhibitor(s) may be present in the MSC-CM (Figure 1b). In addition, inhibition of Ig production by MSC-CM appeared to be general rather than isotype-specific because the production of other Ig isotypes, including IgG1 and IgM, was also substantially inhibited by MSC-CM (Figures 2a and b). Our next goal was to identify the soluble factors that are responsible for the IgE downregulation in B cells. During the process, it was unexpectedly found by our routine quality control program that this MSC-CM was contaminated with mycoplasma (Supplementary Figure 1). Because a recent study reported that T-cell inhibition by MSCs is markedly affected by mycoplasma infection,27 we then tried to examine whether B-cell inhibition by MSC-CM is also influenced by mycoplasma infection. In order to eradicate mycoplasmas from infected MSCs, the cells were treated with a commercial antimycotic reagent according to the manufacturer’s instruction. Mycoplasma eradication from MSCs was verified by the negative result of the mycoplasma PCR (Figure 2b). Surprisingly, CM harvested from antimycotic-treated MSCs did not downregulate IgE production by B cells. Furthermore, the production of other immunoglobulins, including IgM and IgG1, was not inhibited by the same antimycotic-treated MSC-CM (Figure 2a). These results strongly suggest that MSC-CM-mediated Ig downregulation in B cells is possibly correlated with mycoplasma contamination.
MSCs inhibited IgE production in B cells. (a) Purified B cells secreted IgE in the presence of LPS (10 μg/ml) and IL-4 (30 ng/ml). When MSCs were co-cultured, IgE secretion from B cells was significantly decreased. IgE downregulation was observed in the absence of cell–cell contact between MSCs and B cells in a transwell system. CM harvested from MSCs after 3-day cultivation also markedly inhibited IgE production. Extracellular protein levels of IgE were quantitatively measured by ELISA. (b) LPS-IL-4-mediated IgE induction was significantly suppressed by serial dilution of MSC-CM. NC, negative control with no stimulus; CC, co-culture; TW, transwell system; CM, MSC-CM
CM harvested from mycoplasma-free MSCs did not inhibit IgE production in B cells. (a) In addition to IgE, production of other Ig isotypes including IgM and IgG1 was also decreased by mycoplasma-contaminated MSC-CM in LPS/IL-4-stimulated B cells. However, Ig production (IgE, IgG1, and IgM) was not observed when mycoplasma-free MSC-CM was added. (b) Mycoplasma infection was determined by PCR. myco(+), CM from mycoplasma-infected MSCs; myco(−), CM from mycoplasma-free MSCs
M. arginini was responsible for Ig downregulation by MSC-CM
Next, we analyzed the DNA present in mycoplasma-infected MSC-CM to identify the infecting mycoplasma strain. DNA sequence analysis strongly indicated that M. arginini is the infecting strain (Supplementary Figures 1a and b; Supplementary Table 1). To determine whether this strain is specifically responsible for Ig downregulation by MSC-CM, we purchased the identified strain from American Type Culture Collection (ATCC, Manassas, VA, USA). Our approach was to evaluate whether mycoplasma infection explains the MSC-CM-mediated Ig downregulation in B cells by directly infecting healthy MSCs with cultured microbes. Mycoplasma-free MSCs were directly infected with different titers of the mycoplasma strain and PCR analysis was then performed for its detection. M. arginini-specific PCR detection was verified (Supplementary Figure 1b). On the basis of semi-quantitative PCR results, we estimated that there are ∼20 colony-forming units per milliliter (cfu/ml) of M. arginini in MSC-CM (Supplementary Figure 1c).
We then determined the minimal number of M. arginini required to infect two different cell types, mouse dermal fibroblasts (MDFs) and MSCs. Mycoplasma-free MSCs and MDFs were inoculated with several cfu/ml of M. arginini and cultured. On the basis of the results of M. arginini-specific PCR, the minimal numbers of microbes required for successful infection were 20 cfu/ml for MDFs and 40 cfu/ml for MSCs (Figure 3a). When CMs harvested from mycoplasma-free or -infected cells were evaluated for their effect on the IgE production in B cells, only CMs from M. arginini-infected cells inhibited the IgE production in B cells, regardless of the cell type (Figure 3b). CMs from M. arginini-free MSCs or MDFs did not influence the IgE production in B cells. On the other hand, we wondered whether M. arginini itself affects the IgE production in B cells. When M. arginini was added to LPS/IL-4-stimulated B cells, the IgE production was significantly reduced (Figure 3c). It appeared that just 2 cfu/ml of M. arginini were sufficient for IgE downregulation (Figure 3c). In addition, other Ig isotypes such as IgG1 and IgM were also significantly downregulated by M. arginini (Figure 3d). These results suggest that the inhibition of the Ig production in B cells is specifically correlated with the presence of M. arginini.
M. arginini specifically downregulated IgE production in B cells. (a) To estimate the minimal numbers of infecting mycoplasma required to infect host cells, two cell types including MDF and MSC were infected with 10–80 cfu/ml of cultured M. arginini. MDF was included because it is a type of fibroblast without stem cell properties. M. arginini-specific PCR was performed for validity of infection. (b) IgE levels in LPS/IL-4-stimulated B cells were measured after incubation with CMs harvested from mycoplasma-free cells or from M. arginini-infected cells. In parallel, M. arginini infection to MDF or MSC was determined by PCR. (c) Several numbers of M. arginini (1, 2, 4, and 20 cfu/ml) were directly added to LPS/IL-4-stimulated B cells and then secreted IgE concentration was measured by ELISA. Significant existence of M. argininiin CM was determined by PCR. (d) After M. arginini (20 cfu/ml) was added to LPS/IL-4-stimulated B cells, IgG1 and IgM levels were determined by ELISA. myco(+), CM from mycoplasma-infected MDFs or MSCs; myco(−), CM from mycoplasma-free MDFs or MSCs, Ma, M. arginini
Cellular soluble factors secreted from M. arginini-infected MSCs contributed to Ig downregulation in B cells
Intriguingly, we noticed that a highly diluted MSC-CM sample could inhibit IgE production, although mycoplasma was not detectable by PCR (sample 5; 25 600-fold dilution, Figure 4a). This observation implied the existence of a secreted cellular factor(s) other than mycoplasma particles. Therefore, we hypothesized that a soluble factor(s) secreted from mycoplasma-infected MSCs may mediate Ig downregulation in B cells. To investigate whether a soluble factor(s) present in mycoplasma-contaminated MSC-CM is involved in Ig downregulation, we simply removed mycoplasma particles from MSC-CM by passing through a 0.22-μm filter and then used the filtered CM to assay its effect on IgE production. The filtrate inhibited the IgE production in B cells to the same extent as non-filtered CM did (Figure 4b). The absence of mycoplasma in this filtrate was confirmed by PCR as shown in Figure 4b. These results indicate that not only mycoplasma particles but also an unknown soluble cellular factor(s) secreted from mycoplasma-infected MSCs contributes to the immunoregulatory functions of B cells.
MSC-CM lacking M. arginini still inhibited IgE production in B cells. (a) CM harvested from M. arginini-infected MSCs was serially diluted up to 25 600-fold and added to LPS/ IL-4-stimulated B cells. Each dilution in hexaplicates was subjected to IgE measurement. Relative IgE concentrations over 90% and under 40% to positive control (IgE in LPS/IL-4-stimulated B cells with no CM) were shown in white (○) and black (●) circles, respectively. Existence of M. arginini was determined by M. arginini-specific PCR reactions. (b) Mycoplasma-infected MSC-CM was filtrated through a 0.22-μm syringe filter. The filtrate and non-filtered MSC-CM were added to LPS/IL-4-stimulated B cells and then IgE was measured by ELISA. M. arginini-specific PCR was performed. myco(+), CM from mycoplasma-infected MSCs
Next, in order to confirm and characterize a soluble factor(s) that inhibits the IgE production in B cells, the MSC-CM was subjected to heat inactivation, protein transport inhibition, and size fractionation. First, we measured the inhibitory activity of the CM after boiling (or heat inactivation) to examine whether the soluble factor(s) is a protein. Boiling abrogated the inhibitory activity of MSC-CM on IgE production, indicating that the soluble factor(s) is a protein (Figure 5a). Second, we examined the effect of monensin, a protein transport inhibitor, on the inhibitory activity of MSC-CM. IgE downregulation was not observed when monensin-treated MSC-CM was used, suggesting that the soluble protein factor(s) is synthesized intracellularly and secreted extracellularly through a cellular protein transport process (Figure 5b). This result was also consistent with the result from the heat inactivation experiment. Third, we tried to approximate the size of the molecule by fractionating MSC-CM according to the molecular weight. The size of the putative soluble factor(s) was estimated to be over 50 kDa (Figure 5c). Next, we performed fast protein liquid chromatography (FPLC) to separate the putative soluble factor(s) from MSC-CM according to the molecular weight (Figure 5d). IgE downregulation in B cells was evident in only three fractions (fractions 12, 13, and 14) (Figure 5e). The other fractions were excluded because their effect on IgE inhibition was unclear. No inhibition was observed in MDF-CM fractions or the culture medium (Figure 5f). Therefore, these results suggest that M. arginini-infected MSCs secrete a soluble protein molecule(s) that is able to inhibit the IgE production in B cells.
M. arginini-infected MSCs secreted soluble factors inhibiting IgE production in B cells. (a) Mycoplasma-infected MSC-CM was heat-inactivated by boiling for 5 min (boiled CM). The effect of boiled CM on IgE production in B cells was assessed by ELISA. (b) MSCs were treated with 2 μM monensin (Mon) or vehicle for 24 h and then CMs were harvested. Each CM was added to LPS/IL-4-stimulated B cells followed by IgE measurement. (c) Mycoplasma-infected MSC-CM was size-fractionated and then added to LPS/IL-4-induced B cells. Secreted IgE levels were determined by ELISA. (d) FPLC was performed with 200-fold concentrated M. arginini-infected MSC-CM, MDF-CM, and medium control. (e) After FPLC fractions (from fraction numbers 8 to 25) were added to LPS/IL-4-stimulated B cells, the effect of each fraction on IgE downregulation was examined. (f) ELISA was conducted to assess the effects of M. arginini-infected MSC-CM fractions (11–14), MDF-CM fractions (11–14), and medium fractions on IgE downregulation
C3 secreted from M. arginini-infected MSCs was identified to negatively regulate Ig production in B cells
To identify the soluble factor secreted from mycoplasma-infected MSCs responsible for the downregulation of IgE in B cells, we performed liquid chromatography (LC) analysis with fraction 13 of MSC-CM, MDF-CM, and medium. Among the top 100 proteins identified according to peptide score and coverage percentage (Supplementary Table 2), we selected 12 candidate molecules of which the expression was exclusive in MSC-CM according to their potential role in B-cell regulation (Table 1). We further selected four proteins, including C3, haptoglobin, translationally-controlled tumor protein (TCTP), and cathepsin L; the protein expression of each molecule in MSC-CM was confirmed by either an enzyme-linked immunosorbent assay (ELISA) or western blot analysis (Supplementary Figure 2). Among these four candidate proteins, we investigated the effect of C3, the most potential candidate with the highest peptide score in the LC analysis. When MSCs were infected with M. arginini, C3 was detected in the CM (Figure 6a). However, it was not detected in CM harvested from B cells after mycoplasma infection (Figure 6a), indicating that M. arginini infection specifically affects MSCs to secrete C3. Mouse C3 protein by itself downregulated IgE as well as IgG1 and IgM in B cells (Figures 6b and c). As expected, heat-inactivated C3 treatment of B cells did not reduce the IgE production (Figure 6b). To obtain further evidence of C3 involvement, the downregulation of IgE by mycoplasma-infected MSC-CM was evaluated in the presence of the C3 inhibitor compstatin. Treatment with compstatin reversed the MSC-CM-mediated downregulation of IgE in a dose-dependent manner (Figure 6d). In the presence of compstatin, mycoplasma-infected MSC-CM did not reduce the production of IgG1 and IgM (Figure 6f). The inhibition of IgE production with a size-fractionated sample (fraction 13) of mycoplasma-infected MSC-CM was also abrogated by compstatin treatment (Figure 6e). Taken together, these results suggest that C3 secreted from mycoplasma-infected MSCs may inhibit Ig production in B cells by hampering B-cell differentiation into antibody-producing plasma cells. To investigate this possibility, we examined whether B-cell expression of B-cell-induced maturation protein-1 (Blimp-1), one of the most important regulators in plasma cell differentiation, was influenced by C3 treatment. Blimp-1 expression in B cells was enhanced by LPS/IL-4 stimulation, whereas its expression was completely blocked by either mycoplasma-infected MSC-CM or C3 protein (Figure 6g). Compstatin treatment restored the MSC-CM-induced inhibition of the Blimp-1 expression (Figure 6g). Furthermore, C3, inactivated by boiling, did not block the Blimp-1 expression (Figure 6g). Although it remains unclear at present whether C3 suppresses the Blimp-1 expression directly or indirectly, it is evident that mycoplasma infection-associated abnormal C3 expression from MSCs negatively regulates B-cell differentiation. Collectively, our results showed that mycoplasma infection enhances the MSC-mediated B-cell immunosuppression by altering MSCs to secrete C3, thereby mediating the inhibition of B-cell differentiation.
C3 secreted from M. arginini-infected MSC-CM was responsible for Ig downregulation in B cells. (a) Secreted C3 level in M. arginini-infected MSC-CM was quantitatively measured by ELISA. C3 secretion was apparent only in mycoplasma-infeced MSCs. C3 was not detected in B-cell-CM (B-CM) regardless of mycoplasma infection. (b) When mouse C3 (10 ng/ml) was added to LPS/IL-4-stimulated B cells, it significantly inhibited IgE production as mycoplasma-infected MSC-CM. IgE downregulation was abrogated when boiled C3 was added to the culture. (c) Elevated production of IgG1 and IgM in LPS/IL-4-stimulated B cells was also reduced with C3 treatment (10 ng/ml). (d) Compstatin suppressed IgE downregulation by mycoplasma-infected MSC-CM in a dose-dependent manner. (e) IgE production inhibited by a FPLC fraction number 13 was restored by compstatin. (f) Compstatin treatment restored the reduced production of IgG1 and IgM by mycoplasma-infected MSC-CM. (g) Blimp-1 expression in LPS/IL-4-stimulated B cells was examined by semi-quantitative RT-PCR. In B cells, Blimp-1 expression induced by LPS/IL-4 stimulation was not observed by addition of mycoplasma-infected MSC-CM or by C3 treatment. In the presence of compstatin, Blimp-1 downregulation by the MSC-CM was restored. It is likely that boiled C3 treatment does not downregulate Blimp-1 expression. myco(+), CM from mycoplasma-infected MSCs or B cells; myco(−), CM from mycoplasma-free MSCs or B cells. Significance was *P<0.01, **P<0.001, or ***P<0.01
Discussion
Over the past decade, the finding that ex vivo-expanded MSCs can modulate immune responses has promoted the clinical translation of stem cell therapy. The MSC-mediated immunomodulation of T cells has been largely investigated, whereas relatively less attention has been paid to B-cell regulation by MSCs. Only few studies reported the effects of MSCs on B cells, showing contradictory results. Some works showed that MSCs induce antibody production in the presence of splenocytes or a TLR9 ligand.20, 21, 22 In particular, antibody-producing plasma cells were induced via cell–cell contact in the presence of MSCs, when B cells from patients with systemic lupus erythematosus were stimulated with a TLR9 ligand.21 Similar results were observed in mice; MSCs inhibited the antibody production by B cells in the presence of LPS, splenocytes, or a TLR9 ligand,16, 17, 18, 19 whereas MSCs increased the in vivo production of IgM and IgG in both T-cell-dependent and -independent manners.22 Contrarily, other studies showed that MSCs suppress the antibody production by human B cells in the presence of activated T cells, plasmacytoid dendritic cells, or a TLR9 ligand.12, 13, 14, 15 It has been demonstrated that MSCs inhibit the antibody production by B cells in transwell systems as well as in co-culture systems.12, 14, 15, 18, 19 Considering these results, soluble factors secreted from splenocytes, peripheral blood mononuclear cells, or B cells probably activate MSCs and the activated MSCs inhibit B-cell functions subsequently. However, Rafei et al.17 reported that MSC-CM alone is sufficient to decrease the number of antibody-producing splenocytes from ovalbumin-immunized mice. The authors suggested that the soluble factors secreted from MSCs are matrix metalloproteinases and chemokine (C-C motif) ligand 2, which suppress the antibody production in B cells.17 This discrepancy between MSC activation by neighboring cell-secreted soluble factors and MSC-secreted molecules themselves may be owing to different stimulators and conditions, different MSCs, or undefined factors.
In this study, we showed for the first time how an unexpected mycoplasma contamination in MSC cultures can affect B-cell functions. Mycoplasma contamination is a well-known problem in cell culture laboratories. The most common contaminants in cell cultures include M. arginini, M. fermentans, M. orale, M. hyorhinis, and Acholeplasma. laidlawii.24 However, little has been reported on the effects of mycoplasma contamination in MSCs. Zinocker et al.26 showed that mycoplasma-contaminated MSCs enhance the inhibition of T-cell proliferation in vitro. Their MSCs were found to be contaminated with M. hyorhinis. In our study, M. arginini was identified as MSC-infecting mycoplasma strain (Supplementary Figure1) and found to be significantly correlated with antibody downregulation. Intriguingly, we found that M. arginini not only directly suppressed the Ig production in B cells but also indirectly downregulated Ig production without affecting the activation status of B cells (Supplementary Figures 3a and b). The direct downregulation by M. arginini appeared to be different from the indirect mechanism with no influence on B-cell activation. Although IgE production was downregulated by direct addition of M. arginini to B-cell cultures, the mycoplasma rather increased B-cell proliferation (unpublished data). We speculate that hyperactivation of B cells by M. arginini likely suppressed IgE production.28 On the other hand, the indirect downregulation occurred through C3, which is induced by M. arginini-infected MSCs (Figure 6a). In addition, C3 alone could suppress the Ig production in B cells (Figures 6b and c).
C3 has a central role in the activation of the complement system and contributes to innate immunity. C3 convertase catalyzes the proteolytic cleavage of C3 into C3a and C3b during activation.29 In humans, complement receptor 1 (CR1 or CD35) and 2 (CR2 or CD21) are expressed on B cells. CR1 binds to C3b and prevents B-cell differentiation to plasmablasts and their Ig production, whereas CR2 binds to iC3b, C3dg, or C3d and transduces a positive activation signal upon colligation with surface IgM.30, 31, 32 The mouse complement system is quite different from the human system. In mice, CR1 and CR2 are generated by alternative splicing of Cr2. In Cr2 (CD21-CD35)-deficient mice, B cells exhibited a reduction in Blimp-1 expression and impaired antibody persistence paralleled by a strongly reduced development of bone marrow plasma cells.33 These findings suggest that complement receptors maintain antibody responses by delivering differentiation and survival signals to bone marrow plasma cell precursors. Unlike in vivo findings, our study showed that C3 directly inhibits Ig production in LPS/IL-4-induced mouse B cells in vitro. This inhibition was rescued by compstatin, a peptide inhibitor of the complement system (Figures 6d–f). Compstatin binds directly to C3 and prevents the cleavage of C3 into C3a and C3b by the C3 convertase.34 It seems that the cleaved C3 product C3b is required for Ig downregulation in B cells. However, it remains unknown whether mouse CR1 negatively regulates B-cell differentiation, as demonstrated in human B cells. Pappworth et al.35 generated human CR1 (hCR1) transgenic mice in the presence of mouse CR1/2. In these mice, the number of CD138-positive plasma cells was reduced in spleens of antigen-immunized mice compared with negative control mice, suggesting that hCR1 overexpression may alter B-cell differentiation in mice.35 On the basis of these data and our results, we speculate that C3 from M. arginini-infected MSCs can bind to CR1 and inhibit B-cell differentiation via inhibition of Blimp-1 expression. However, the molecular mechanism by which C3/C3b regulates Blimp-1 expression needs to be elucidated.
M. arginini is a mammalian parasite found in a number of animal species. Accumulating evidence in the case reports suggests the pathogenic role of M. arginini as a new human zoonosis. M. arginini was first reported to cause a fatal septicemia with pneumonia in a 64-year-old patient with advanced non-Hodgkin’s lymphoma.36 A recent case report provided another evidence of eosinophilic fasciitis associated with M. arginini infection in a 23-year-old man.37M. arginini was also reported to be isolated from an open femur fracture by an African lion attackin a 56-year-old hunter and from the blood of an immunocompromised Japanese patient with advanced non-Hodgkin’s lymphoma.27, 38 Therefore, these findings suggest the pathogenicity of M. arginini in humans.
The results of our study speculate a potentially new mechanism of the immunomodulatory function of infused MSCs in vivo, which is difficult to observe in vitro. For example, MSCs transplanted into a patient can encounter pathogens in the blood stream and then get stimulated and secret immunomodulatory factors, such as C3 as demonstrated in this study, to regulate the transcription of genes in immune cells. If this is true, the response of MSC treatment to patients may vary depending on the pre-existing condition of each patient, which may require a pre-examination of patients before MSC transplantation. However, the relationship between a host pathogen and MSCs remains elusive. The immunomodulatory effects of MSCs are being exploited in clinical settings, for example, in patients with autoimmune diseases such as graft-versus-host disease, rheumatoid arthritis, type I diabetes, and Crohn’s disease, after allogeneic stem cell transplantation. The findings of this study may initiate the unfolding of unknown mechanisms of immunomodulatory functions of MSCs and provide a scientific basis of why MSCs have different outcomes on a wide range of immune diseases.
It is unlikely that mycoplasma contamination deprives MSCs of their stem cell properties, including differentiation potential, proliferation, cytokine secretion, and stem cell marker expression. Thus, mycoplasma contamination in MSC cultures may not be recognized. Because mycoplasma-infected MSCs show remarkably enhanced immunomodulatory activity, more attention and routine examination is required, especially in investigations on the immunomodulation of MSCs.
Our present study suggests that C3 secreted from M. arginini-infected MSCs has an important role in Ig production of B cells via regulation of Blimp-1. However, its role in vivo needs to be explored. In addition, further study is required as to whether C3 treatment itself has the same effects in vivo as it has in M. arginini-infected MSCs.
Materials and Methods
Cell culture
MSCs were isolated from C3H HeN (Orient, Seongnam, Korea) bone marrow according to the subfractionation culturing method.39 MDFs were isolated from C3H HeN dermal tissue. These two cell lines were incubated using Dulbecco’s modified Eagle’s medium with low glucose (Gibco, Carlsbad, CA, USA) and supplemented with 10% fetal bovine serum (Gibco) and 1 × antibiotic-antimycotic solution (Gibco) at 37 °C in 5% CO2. B cells were isolated from Balb/c splenocytes using the EasySep Mouse B Cell Enrichment Kit (StemCell Technologies, Vancouver, BC, Canada) and cultured in RPMI 1640 (Hyclone, South Logan, UT, USA) supplemented with 10% fetal bovine serum (Gibco), 2-mercaptoethanol (Gibco), and 1 × antibiotic-antimycotic solution (Gibco).
CM preparation
MSC- or MDF-derived CM was harvested 3 days post incubation. For some experiments, CM was subjected to some modifications; CM was filtered using a 0.22-μm syringe filter (Pall Corporation, Port Washington, NY, USA); filtered CM was heat-inactivated at 100 °C for 5 min; CM was treated with different doses (15–60 μM) of compstatin (TOCRIS, Bristol, UK), which is a C3 inhibitor; CM was separated using filter units with a molecular weight cutoff size of 50 or 100 kDa (Millipore, Billerica, MA, USA). For FPLC separation and western blot analysis, 200 ml of filtered CM, which was harvested 3 days post incubation in the absence of serum, were concentrated (200 × ) using filter units with a molecular weight cutoff size of 50 kDa. For ER/Golgi block, cells were incubated for 24 h with 2 μM of monensin (Sigma, St. Louis, MO, USA), which blocks the protein transport from the endoplasmic reticulum to the Golgi apparatus. Then, CM was harvested and filtered by using a 0.22-μm syringe filter.
Co-culture and B-cell treatment
The experiments were set up using 24-well culture plates (1 ml culture medium per well). Briefly, 105 cells of MSCs in 100 μl of MSC culture medium were mixed with 106 B cells for co-culture experiments. For transwell experiments, cells were seeded on the upper side of a transwell chamber (Corning, Tewksbury, MA, USA) on a membrane with a 5.0-μm pore size. CM was added at a 1 : 10 (v/v) ratio to B cells (unmodified and filtered, boiled, or size-fractionated, respectively). B cells were stimulated with 10 μg/ml LPS (Sigma) and 30 ng/ml mouse IL-4 (Prospec-TanyTechnogene, Rehovot, Israel). Mouse C3 (Kamiya Biomedical Co., Seattle, WA, USA) was treated with B cells at a concentration of 10 ng/ml.
ELISA and western blot analysis
The titers of IgE, IgM, and IgG1 in culture medium of B cells were measured by using ELISA (BD Pharmingen, San Diego, CA, USA). Levels of C3 and haptoglobin in CM were measured by using the C3 ELISA kit (Kamiya Biomedical Co.) and the Haptoglobin ELISA kit (Abnova, Taipei, Taiwan). TCTP and cathepsin L in the CMs were detected by performing a western blot analysis using the following antibodies; purified mouse anti-TCTP (BD Biosciences, San Jose, CA, USA), mouse anti-cathepsin L (Pierce, Rockford, IL, USA), and horseradish peroxidase-conjugated anti-mouse IgG (Santa Cruz Biotechnology, Dallas, TX, USA).
Mycoplasma
Mycoplasmas in CM and cell lysates were detected by using a mycoplasma detection kit (e-Myco, iNtRON, Sungnam, Korea) and M. arginini-detecting PCR using the following primer sequences: Forward: 5′-GATTCCGTTGTGAAAGGAGC-3′, Reverse: 5′-TCAAGCTTTCGCTC ATTGTG-3′. The 16S ribosomal DNA region of the strain with which the cell lines were infected was amplified by PCR and sequenced. These sequences were then compared with those in the NCBI databases using BLAST version 2.2.28+. M. arginini (ATCC 23243) was obtained from ATCC and propagated in mycoplasma medium.26 For mycoplasma eradication, mycoplasma-contaminated MSCs were treated with a commercial antimycotic reagent MycoGONE (Genlantis, San Diego, CA, USA) according to the manufacturer’s instruction. Mycoplasma eradication was evaluated by PCR. Mycoplasma infection was done by inoculating mycoplasma-free MSCs or MDFs with M. arginini and cultured for 3 days. Successful infection of the cells was confirmed by PCR (Bio-Rad, Hercules, CA, USA).
FPLC purification
FPLC was performed on an ÄKTA Prime plus system (GE Healthcare Life Sciences, London, UK). The concentrated CM was loaded onto a superose 12 10/300 GL column (GE Healthcare Life Sciences) equilibrated in phosphate-buffered saline. The column was eluted with two-column volumes of buffer. The fractions were filtered with a 0.22-μm syringe filter before using them for treatment of B cells.
LC
The FPLC fractions that had an effect on the IgE production of B cells were digested with trypsin (Promega, Madison, WI, USA). Nano-LC-tandem mass spectroscopy (MS/MS) analysis was performed on an Agilent 1100 series nano-LC and LTQ-mass spectrometer (Agilent, Santa Clara, CA, USA). The capillary column used for LC-MS/MS analysis (150 × 0.075 mm) was obtained from Proxeon (Odense M, Denmark) and slurry-packed in house with Magic C18 stationary phase (5 μm particle size, 100 Å pore size; MichromBioResources, Auburn, CA, USA). The mobile phase A for LC separation was 0.1% formic acid in deionized water and mobile phase B was 0.1% formic acid in acetonitrile. The chromatography gradient was set up to give a linear increase from 5 B to 35% B in 100 min, from 40 B to 60% B in 10 min, and from 60 B to 80% B in 20 min. The flow rate was maintained at 300 nl/min after splitting. Mass spectra were acquired using data-dependent acquisition with full mass scan (400–1800 m/z) followed by MS/MS scans. Each acquired MS/MS scan was an average of three microscans on the LTQ. The temperature of the ion transfer tube was controlled at 200 °C and the spray voltage was in the range 1.5–2.0 kV. The normalized collision energy was set at 35% for MS/MS. Mass tolerances of 1.2 and 0.6 Da were used for precursor and fragment ions, respectively. Peptides were allowed to be variably oxidized at methionine residues and to be variably carboxyamidomethylated at cysteine residues.
Reverse transcription (RT)-PCR
Total RNA was isolated from LPS/IL-4-induced B cells using a total RNA extraction kit, easy-BLUE (iNtRON). RNA was reverse-transcribed using AccuPower RT PreMix (Bioneer, Daejeon, Korea) and OligodT (Bioneer). Blimp-1 and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) were detected by PCR using the following primer sequences: Blimp-1-F: 5′-TGGTATTGTCGGGACTTTGC-3′, Blimp-1-R: 5′-TGGGGACACTCTTTGGGTAG-3′, GAPDH-F: 5′-CCACTGGCGTCTTCACCAC-3′, GAPDH-R: 5′-CCTGCTTCA CCACCTTCTTC-3′. GAPDH was used for loading the control.
Abbreviations
- Blimp-1:
-
B-lymphocyte-induced maturation protein-1
- CM:
-
conditioned medium
- C3:
-
complement C3
- FPLC:
-
fast protein liquid chromatography
- Ig:
-
immunoglobulin
- IL-4:
-
interleukin-4
- LC:
-
liquid chromatography
- LPS:
-
lipopolysaccharide
- MDF:
-
mouse dermal fibroblasts
- MSCs:
-
mesenchymal stem cells
- TLR:
-
Toll-like receptor
References
Porada CD, Zanjani ED, Almeida-Porad G . Adult mesenchymal stem cells: a pluripotent population with multiple applications. Curr Stem Cell Res Ther 2006; 1: 365–369.
Le Blanc K, Ringden O . Mesenchymal stem cells: properties and role in clinical bone marrow transplantation. Curr Opin Immunol 2006; 18: 586–591.
Ozawa K, Sato K, Oh I, Ozaki K, Uchibori R, Obara Y et al. Cell and gene therapy using mesenchymal stem cells (MSCs). J Autoimmun 2008; 30: 121–127.
Ramasamy R, Tong CK, Seow HF, Vidyadaran S, Dazzi F . The immunosuppressive effects of human bone marrow-derived mesenchymal stem cells target T cell proliferation but not its effector function. Cell Immunol 2008; 251: 131–136.
Le Blanc K . Immunomodulatory effects of fetal and adult mesenchymal stem cells. Cytotherapy 2003; 5: 485–489.
Uccelli A, Moretta L, Pistoia V . Mesenchymal stem cells in health and disease. Nat Rev Immunol 2008; 8: 726–736.
Yi T, Song SU . Immunomodulatory properties of mesenchymal stem cells and their therapeutic applications. Arch Pharm Res 2012; 35: 213–221.
Bartholomew A, Sturgeon C, Siatskas M, Ferrer K, McIntosh K, Patil S et al. Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo. Exp Hematol 2002; 30: 42–48.
Nauta AJ, Kruisselbrink AB, Lurvink E, Willemze R, Fibbe WE . Mesenchymal stem cells inhibit generation and function of both CD34+-derived and monocyte-derived dendritic cells. J Immunol 2006; 177: 2080–2087.
Aggarwal S, Pittenger MF . Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood 2005; 105: 1815–1822.
Maccario R, Podesta M, Moretta A, Cometa A, Comoli P, Montagna D et al. Interaction of human mesenchymal stem cells with cells involved in alloantigen-specific immune response favors the differentiation of CD4+ T-cell subsets expressing a regulatory/suppressive phenotype. Haematologica 2005; 90: 516–525.
Corcione A, Benvenuto F, Ferretti E, Giunti D, Cappiello V, Cazzanti F et al. Human mesenchymal stem cells modulate B-cell functions. Blood 2006; 107: 367–372.
Bochev I, Elmadjian G, Kyurkchiev D, Tzvetanov L, Altankova I, Tivchev P et al. Mesenchymal stem cells from human bone marrow or adipose tissue differently modulate mitogen-stimulated B-cell immunoglobulin production in vitro. Cell Biol Int 2008; 32: 384–393.
Comoli P, Ginevri F, Maccario R, Avanzini MA, Marconi M, Groff A et al. Human mesenchymal stem cells inhibit antibody production induced in vitro by allostimulation. Nephrol Dial Transplant 2008; 23: 1196–1202.
Tabera S, Perez-Simon JA, Diez-Campelo M, Sanchez-Abarca LI, Blanco B, Lopez A et al. The effect of mesenchymal stem cells on the viability, proliferation and differentiation of B-lymphocytes. Haematologica 2008; 93: 1301–1309.
Deng W, Han Q, Liao L, Li C, Ge W, Zhao Z et al. Engrafted bone marrow-derived flk-(1+) mesenchymal stem cells regenerate skin tissue. Tissue Eng 2005; 11: 110–119.
Rafei M, Hsieh J, Fortier S, Li M, Yuan S, Birman E et al. Mesenchymal stromal cell-derived CCL2 suppresses plasma cell immunoglobulin production via STAT3 inactivation and PAX5 induction. Blood 2008; 112: 4991–4998.
Asari S, Itakura S, Ferreri K, Liu CP, Kuroda Y, Kandeel F et al. Mesenchymal stem cells suppress B-cell terminal differentiation. Exp Hematol 2009; 37: 604–615.
Che N, Li X, Zhou S, Liu R, Shi D, Lu L et al. Umbilical cord mesenchymal stem cells suppress B-cell proliferation and differentiation. Cell Immunol 2012; 274: 46–53.
Rasmusson I, Le Blanc K, Sundberg B, Ringden O . Mesenchymal stem cells stimulate antibody secretion in human B cells. Scand J Immunol 2007; 65: 336–343.
Traggiai E, Volpi S, Schena F, Gattorno M, Ferlito F, Moretta L et al. Bone marrow-derived mesenchymal stem cells induce both polyclonal expansion and differentiation of B cells isolated from healthy donors and systemic lupus erythematosus patients. Stem Cells 2008; 26: 562–569.
Ji YR, Yang ZX, Han ZB, Meng L, Liang L, Feng XM et al. Mesenchymal stem cells support proliferation and terminal differentiation of B cells. Cell Physiol Biochem 2012; 30: 1526–1537.
Citti C, Blanchard A . Mycoplasmas and their host: emerging and re-emerging minimal pathogens. Trends Microbiol 2013; 21: 196–203.
Drexler HG, Uphoff CC . Mycoplasma contamination of cell cultures: Incidence, sources, effects, detection, elimination, prevention. Cytotechnology 2002; 39: 75–90.
Logunov D, Shchebliakov DV, Zubkova OV, Shmarov MM, Rakovskaia IV, Gintsburg LA et al. Lipid-associated membrane lipopeptides of M. arginini activate NF-kB by interacting with TLR2/1, TLR2/6, and TLR2/CD14. Mol Gen Mikrobiol Virusol 2009; 2: 25–28.
Zinocker S, Wang MY, Gaustad P, Kvalheim G, Rolstad B, Vaage JT . Mycoplasma contamination revisited: mesenchymal stromal cells harboring Mycoplasma hyorhinis potently inhibit lymphocyte proliferation in vitro. PloS One 2011; 6: e16005.
Prayson MJ, Venkatarayappa I, Srivastava M, Northern I, Burdette SD . Deep infection with Mycoplasma Arginini in an open femur fracture secondary to an African lion bite: a case report. Injury Extra 2008; 39: 243–246.
Jabara HH, Chaudhuri J, Dutt S, Dedeoqlu F, Weng Y, Murphy MM et al. B-cell receptor cross-linking delays activation-induced cytidine deaminase induction and inhibits class-switch recombination to IgE. J Allergy Clin Immunol 2008; 121: 191–196.
Wagner E, Frank MM . Therapeutic potential of complement modulation. Nat Rev Drug Discov 2010; 9: 43–56.
Rickert RC . Regulation of B lymphocyte activation by complement C3 and the B cell coreceptor complex. Curr Opin Immunol 2005; 17: 237–243.
Kremlitzka M, Polgar A, Fulop L, Kiss E, Poor G, Erdei A . Complement receptor type 1 (CR1, CD35) is a potent inhibitor of B-cell functions in rheumatoid arthritis patients. Int Immunol 2013; 25: 25–33.
Carroll MC . CD21/CD35 in B cell activation. Semin Immunol 1998; 10: 279–286.
Gatto D, Pfister T, Jegerlehner A, Martin SW, Kopf M, Bachmann MF . Complement receptors regulate differentiation of bone marrow plasma cell precursors expressing transcription factors Blimp-1 and XBP-1. J Exp Med 2005; 201: 993–1005.
Soulika AM, Holland MC, Sfyroera G, Sahu A, Lambris JD . Compstatin inhibits complement activation by binding to the beta-chain of complement factor 3. Mol Immunol 2006; 43: 2023–2029.
Pappworth IY, Hayes C, Dimmick J, Morgan BP, Holers VM, Marchbank KJ . Mice expressing human CR1/CD35 have an enhanced humoral immune response to T-dependent antigens but fail to correct the effect of premature human CR2 expression. Immunobiology 2012; 217: 147–157.
Yechouron A, Lefebvre J, Robson HG, Rose DL, Tully JG . Fatal septicemia due to Mycoplasma arginini: a new human zoonosis. Clin Infec Dis 1992; 15: 434–438.
Sillo P, Pinter D, Ostorhazi E, Mazan M, Wikonkal N, Ponyai K . Eosinophilic Fasciitis associated with Mycoplasma arginini infection. J Clin Microbiol 2011; 50: 1113–1117.
Watanabe M, Hitomi S, Goto M, Hasegawa Y . Bloodstream infection due to Mycoplasma arginini in an immunocompromised patient. J Clin Microbiol 2012; 50: 3133–3135.
Song SU, Kim CS, Yoon SP, Kim SK, Lee MH, Kang JS et al. Variations of clonal marrow stem cell lines established from human bone marrow in surface epitopes, differentiation potential, gene expression, and cytokine secretion. Stem Cells Dev 2008; 17: 451–461.
Acknowledgements
This study was supported by the Bio and Medical Technology Development Program (NRF-2011-0019634 and NRF-2011-0019637) of the National Research Foundation by the Korean government (MEST), and by a grant from the Inha University (44773-01).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by M Agostini
Supplementary Information accompanies this paper on Cell Death and Disease website
Supplementary information
Rights and permissions
Cell Death and Disease is an open-access journal published by Nature Publishing Group.This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Lee, DS., Yi, T., Lee, HJ. et al. Mesenchymal stem cells infected with Mycoplasma arginini secrete complement C3 to regulate immunoglobulin production in b lymphocytes. Cell Death Dis 5, e1192 (2014). https://doi.org/10.1038/cddis.2014.147
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2014.147
Keywords
This article is cited by
-
Effects of cryopreservation and long-term culture on biological characteristics and proteomic profiles of human umbilical cord-derived mesenchymal stem cells
Clinical Proteomics (2020)
-
Interactions between mesenchymal stem cells and the immune system
Cellular and Molecular Life Sciences (2017)