Abstract
Myocardial ischemia–reperfusion (I/R) causes severe cardiac damage. Although the primary function of oxymyoglobin (Mb) has been considered to be cellular O2 storage and supply, previous research has suggested that Mb is a potentially protective element against I/R injury. However, the mechanism of its protective action is still largely unknown. With a real-time fluorescent technique, we observed that at the onset of ischemia, there was a small burst of superoxide (O2•–) release, as visualized in an isolated rat heart. Thus, we hypothesize that the formation of O2•– correlates to Mb due to a decrease in oxygen tension in the myocardium. Measurement of O2•– production in a Langendorff apparatus was performed using surface fluorometry. An increase in fluorescence was observed during the onset of ischemia in hearts perfused with a solution of hydroethidine, a fluorescent dye sensitive to intracellular O2•–. The increase of fluorescence in the ischemic heart was abolished by a superoxide dismutase mimic, carbon monoxide, or by Mb-knockout gene technology. Furthermore, we identified that O2•– was not generated from the intracellular endothelium but from the myocytes, which are a rich source of Mb. These results suggest that during the onset of ischemia, Mb is responsible for generating O2•–. This novel mechanism may shed light on the protective role of Mb in I/R injury.
Similar content being viewed by others
Main
Ischemia–reperfusion (I/R) injuries are recognized as one of the key factors in the exacerbation of cardiovascular diseases.1 Ischemic preconditioning (IPC), using a few cycles of short ischemic period, is shown to protect against I/R damage in cardiac muscles.2 It has been speculated that IPC could correlate to signaling cascades initiated by reactive oxygen species (ROS),2 yet, the exact redox mechanisms of IPC has not been thoroughly elucidated. For example, there is a lack of direct evidence for ROS formation measured at the onset of ischemia in an intact heart. The source of ROS formation has not been determined during early ischemia, which correlates to the timeframe of IPC.
Oxymyoglobin (Mb) has been shown to have a role in alleviating I/R injuries.3, 4 However, the complete mechanism of its protective action is still unclear. Mb has one O2 binding site consisting of heme, which is a prosthetic group containing an iron (Fe) ion. Mb functions as both an O2 storage site under normal conditions and an O2 supply during temporary deficits.5 The oxygen binding properties of Mb are contingent upon the oxidation state of Fe within the heme group. Ferrous heme (Fe2+) is found in the reduced form of Mb and can function as an O2 binding site. In contrast, when ferric heme (Fe3+) is present in the Mb complex, O2 binding cannot occur. One key physiological result of Fe2+ oxidation is the generation of superoxide (O2•–) through the following reaction:6
Fe2++O2 → Fe3++O2•–
O2•–, a type of ROS, is a biologically important signaling molecule involved in many physiological and pathological processes, including hypoxia, heat stress, septic shock, and muscle dysfunction.7 Increased O2•– formation following ischemia is associated with the pathogenesis of I/R injury.8 Oxidative damage during I/R is commonly linked to the formation of O2•– and generally attributed to reperfusion, a process in which restored flux of O2 encounters a highly reduced environment of ischemic tissue, leading to tissue damage.9, 10 As the correlation between O2•– formation and reperfusion injury has been well studied in the past decade,11, 12, 13 we are primarily focused on O2•– formation at the early phase of ischemia, which is understudied.
O2•– and O2•–-derived oxidants can be formed during the early period of reperfusion.1 Some research showed that this oxidative burst is attributed to the accumulation of xanthine during ischemia and the activation of xanthine oxidase (XO) enzyme at reperfusion.9 Other researchers suggested that the mitochondrion is a primary source.14 However, O2•– formation has not been reported during the onset of myocardial ischemia in a Langendorff heart model.15 Furthermore, the mechanism of O2•– production during early ischemic period has been largely overlooked. It is likely that this may be correlated to IPC, which employs brief cycles of ischemia and has been shown to have a critical role in cardiac therapeutics.2 The production of O2•– at the early ischemia may possibly protect an ischemic heart from further damage during reperfusion via IPC signaling cascades.2
We have previously identified a large burst of O2•– formation during reperfusion in both in vivo and in vitro heart models.1, 16 Thus, the current research is primarily focused on the O2•– formation at early ischemia. We have designed an innovative study which demonstrates that O2•– formation occurs during the onset of ischemia (within the first min). Using an isolated perfused rat heart model, the intracellular O2•– formation is detected by a fluorescent O2•– probe. We hypothesize that Mb oxidation (Fe2+→Fe3+) coupled with the production of O2•– may occur during early ischemia. The current study may help to develop new therapeutic preconditioning methods for I/R injuries, which is consistent with previous research showing that Mb is a potentially protective element during I/R through redox pathways.3
Results
Previous studies have chemically demonstrated that the autoxidation reaction of Mb (Fe2+) to MetMb (Fe3+) results in the accompanied formation of O2•–.17, 18 In order to determine whether O2•– production in real time occurs within the ischemic cardiac tissue, ethidium (ET) fluorescence was monitored in an isolated rat heart with or without ischemia treatment, and recorded in a relative unit using the surface fluorometric method described above. As shown in Figure 1, a rapid increase in ET fluorescence (∼18% of baseline from autofluorescence) was detected within 3 min after the onset of ischemia and reached ∼24% of baseline at 9 min of the ischemic period, as compared with all other treatments (n=5; P<0.05). Meanwhile, autofluorescence decreased in non-loaded ischemic hearts (∼10% at 20 s from the start of ischemia; n=3). This change in the basal fluorescence was likely due to the autofluorescence of intracellular flavine adenine dinucleotide (FAD), which decreased during the course of ischemia or hypoxia in striated muscles.19 To confirm that the elevated ET fluorescence was due to O2•– production in the ischemic heart, superoxide dismutase (SOD) mimetic was used, and it turned out that the increase of ET fluorescence in the ischemia heart was subsequently abolished (n=8). To further analyze the involvement of Mb in O2•– production, we treated the hearts with a CO solution (10%) that potentially blocks ferro-metallo proteins such as Mb from binding to oxygen, which chemically eliminates the formation of O2•–.6 CO treatment reduced ET fluorescence in the ischemic heart compared with the pure ischemia group (n=4). These results strongly indicate that Mb is involved in O2•– formation in the heart at the early onset of ischemia.
As we observed significant O2•– generation within 3 min of ischemia (Figure 1), it is critical to explore this phenomenon in a micro time course during a 1-min period, as illustrated in Figure 2. During the first 12 s of ischemia, there was no obvious change of ET fluorescence. However, at 16 s, the fluorescence started to increase to ∼12% of baseline compared with autofluorescence and reached a peak of ∼18% at 20 s after ischemia. These increases were significant compared with all other groups (n=3; P<0.05), which suggest that O2•– generation in the heart is an immediate response to ischemia.
Mean fluorescence rate (averaged by three rat hearts) was calculated over a micro time course of 60 s immediately following the ischemia period, and was displayed in a relative unit per second. In the ischemia-only group, there are two large spikes (representing rapid increases) and one small spike (for slow increases) on the ET signal rate. Among these three spikes, the first one appears as early as 8 s, the middle one shows at 24 s, and the last one (the smallest) occurs at ∼44 s. This clearly demonstrated that two large O2•– bursts occurred within 24 s from the start of ischemia (Figure 3a). We also noticed that the second peak was∼25% greater than the first one. These spikes were suppressed in both SOD mimic (Figure 3b) and CO groups (Figure 3c), which indicated a possible involvement of Mb in determination of O2•– generation rate. There were no positive spikes in baseline autofluorescence, but a large negative spike was observed, showing that O2•– signal should overcome the autofluorescence decline first before it rises up (as shown in the ischemia group). Thus, we underestimated the increased O2•– signal, which would otherwise have been more significant (Figures 2 and 3).
Mean fluorescence rate (fluorescence change per second; relative unit per second, RU/s) over the time course of 60 s from the start of ischemia in rat heart. (a) mean fluorescence rate in the ischemia-only group. (b) mean fluorescence rate in SOD mimic treatment group. (c) mean fluorescence rate in CO treatment group. (d) mean fluorescence rate in autofluorescence group (n=3)
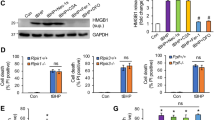
In order to further confirm the role of Mb in O2•– generation in other rodent models, Myo−/− mice and wild-type mice were used following a similar protocol in the rat experiments. As early as 20 s from the start of ischemia, fluorescence was enhanced (∼4% greater than baseline autofluorescence) and maintained throughout the ischemic period in wild-type mice compared with Myo−/− mice (n=4; P<0.05; Figure 4). Interestingly, fluorescence from Myo−/− mice decreased in a manner similar to autofluorescence as shown in Figure 4, suggesting that Mb have an important role in O2•– generation in early ischemia.
Similar to the rat study, the mean rate of increase of ROS fluorescence during the first 60 s of ischemia was calculated in the transgenic mouse model. In the wild-type mice group, a spike in the mean rate of ET signal was observed as early as 16 s (Figure 5a). However in Myo−/− group, this spike disappeared, but a negative spike occurred at 4 s (Figure 5b), which is similar to the response curve from the autofluorescence in rat (Figure 3d).
To determine the cellular location and the source of O2•– production, we analyzed ET fluorescence in an ischemic heart using confocal microscopy via dual-labeling of the myocytes and endothelial cells. Figure 6a showed that the baseline fluorescence before ischemia treatment is kept at a minimal level. Figures 6b and c represent the fluorescent images at 3 min of ischemia, which are brighter in red compared with Figure 6a. This suggests that the early generation of O2•– in response to ischemia. As shown in Figure 6c, the increase of ischemia-induced fluorescence originated from cardiomyocytes (Figures 6b and c; the red represents ROS formation and the green represents endothelium), but not endothelial cells (shown in green in Figure 6c) because there was clearly no overlap between the two dyed areas. These results confirmed that O2•– formation occurred in the Mb-rich cardiac muscle tissue but not in the endothelial tissue.
Localization of O2•– formation during the onset of ischemia on the heart surface using confocal microscopy. (a) heart baseline fluorescence before ischemia. (b) O2•– generation in the HE-loaded heart within 3 min during ischemia. (c) O2•– generation in hearts treated with dual-fluorescence probes (HE and fluorescein lectin I-isolectin B4 (FLI-IB4)), showing that O2•– production is within the cardiomyocytes, not in the endothelial vessels
Discussion
This is the first study demonstrating that Mb is a major source of O2•– formation at the onset of ischemia in a Langendorff heart model. Our data provide an insight into the molecular mechanism of IPC which utilizes ROS generated during early ischemia to protect the cardiomyocytes via redox signaling cascades.2
The generation of reactive, partially reduced oxygen species has been well established as a causative factor for tissue damage that occurs during reperfusion of a previously ischemic tissue.20 Protection against oxidant injury is particularly meaningful during the early reperfusion period after an ischemic insult, which is characterized by the sudden formation of large amounts of O2•–.
Former research assumed that sources such as XO, NADPH oxidase, and the mitochondrial electron transport chain are the primary sources of ROS development during ischemia.15, 21, 22 Other research has shown that ROS formation occurs during extended simulated ischemia (1 h) using cell culture system.15 However, there is no convincing evidence showing any ROS generation in the early stage of cardiac ischemia in a whole-heart model. Yet, the enzyme XO, which oxidizes purines such as hypoxanthine and xanthine to produce uric acid and O2•–, has received a great deal of experimental attention as a source of O2•– during reperfusion,23 but not at the onset of ischemia. Likewise, the mitochondrion is an additional possible source of ROS generation, but has not previously been reported its correlation to ROS formation during early ischemia.24
As questions have remained regarding the production of ROS at the early onset of ischemia, our work has filled the gap of previous knowledge by investigating the potential role of Mb in the production of ROS during ischemia in a Langendorff model. Mb is a ubiquitous protein that is present in the cardiac muscle at relatively high concentrations, and has also been viewed to facilitate the diffusion of O2 in the cardiac muscle.25 Even under normal conditions, Mb undergoes reactions that generate metMb (Fe3+) species and O2•–.26 Yet, the function of Mb has not been previously identified as a potential factor in ROS formation during ischemia. Therefore, the demonstration of O2•– production by Mb gives a new perspective on the mechanism of O2•– formation at the onset of ischemia.
From our previous research16 and current data, this amount of O2•– is small compared with reperfusion-induced ROS, which is ideal for preconditioning signal.2 In addition, our protocol used CO treatment coupled with ischemia to verify that MbO2 autoxidation is a primary source of O2•– generation. As shown in Figures 1 and 2, the fluorescence levels were significantly lower in the ischemia with CO model compared with ischemia alone. As there is no hemoglobin in our Langendorff perfusion apparatus, the binding of CO to the cardiac Mb in our set up effectively prevents O2•– formation. Figure 6 confirmed that O2•– does not originate from Mb-deficient vasculatures but rather from the myocytes, whereby the amount of Mb is abundant.
At ∼20 s from the start of ischemia, the increase of O2•– signal in rat models (∼18%>baseline autofluorescence, Figure 2) was larger than the mouse model (∼4%>baseline autofluorescence, Figure 4). Similarly, in the curves from the mean rate of ROS fluorescence, the rat model had two large O2•– bursts (Figure 3), whereas the mouse model only had one, which is ∼60% smaller (Figure 5). This difference is possibly owing to the usage of different animal models (rat versus mouse). We also noticed that CO only blocked ∼70% of the ischemic signal, whereas almost 100% of the signal was inhibited by the SOD mimic within 20 s after the ischemia started in the rat model (Figure 2). We initially speculated that mitochondria or other ROS generators accounted for this ∼30% difference in the blockage of O2•– signals. However, this is unlikely because the ROS signal was completely abolished in the transgenic Myo−/− mouse model (Figures 4 and 5), suggesting the key role of Mb in O2•– formation. Thus, it is probably due to the partial blockage of Mb by CO as a relatively low dosage of CO as well as a short incubation period was used. Yet, it is difficult to increase this dosage to a greater level as higher levels of CO could directly cause irreversible cardiac failure.
There are other limitations associated with CO blockage. As the Ki of CO for cytochrome oxidase is of the same order as the Km for oxygen,27 the 10% proportion of CO in the gas phase would result in about 10% inhibition of cytochrome oxidase under aerobic conditions. However, when oxygen is depleted upon ischemia, the addition of CO not only blocks Mb function but also inhibits mitochondrial cytochrome oxidase during ischemia. Thus, it is critical to perform Myo−/− mice experiments to verify the role of Mb in our setup.
During the first 60 s from the start of ischemia, the O2•– formation rate is not constant, that is, the generation of O2•– was not continuous, including the first two larger ROS bursts at 8 s and 24 s respectively, followed by an extremely small burst (∼ one-third of the previous one) at 44 s (Figure 3a). This suggested a possible involvement of endogenous antioxidant enzymes such as SOD, catalase, and glutathione peroxidase during early ischemia, which gradually attenuated the O2•– formation rate.19
From a clinical perspective, an oxidative burst occurs in the myocardium during open heart surgery as a result of reperfusion injury following ischemia.28 This oxidative stress overwhelms the antioxidant defense system and leads to DNA damage and protein degradation.28 Hypoxic preconditioning (HPC) partially simulates early hypoxia or ischemia by using a few cycles of short hypoxia treatment to protect skeletal muscles from oxidative damage.29 Our previous work further identified a plausible cellular signaling mechanism of HPC involves a phosphatidylinositol 3-kinase (PI3K), which also has a crucial role in cardiomyocyte protection from I/R injury.29, 30 Similar to HPC, IPC uses a few short cycles of ischemia, which significantly protects cardiac muscle from I/R injury through the opening of mitochondrial ATP potassium channels (KATP channel).2 IPC or HPC can potentially initiate the PI3K signaling pathway to inhibit glycogen synthase kinase-3β, which has beneficial effects on cardiomyocytes,31 as the activation of glycogen synthase kinase-3β leads to mitochondrial permeability transition pore opening, therefore disrupting ATP synthesis.2
Interestingly, confocal data from previous HPC research illustrated that intramuscular ROS formation significantly decreases after HPC treatment,29 and thus it is likely that PI3K activated by HPC can enhance antioxidant defenses in the cardiac muscle as it has done in the skeletal muscle. Furthermore, the activation of mitochondrial KATP channels has been shown in several studies to have a role in preconditioning;32, 33 however, it was recently suggested that the opening of mitochondrial KATP channels initiates the preconditioning by producing free radicals.34 Antioxidants applied before IPC or HPC treatment significantly decrease the cardioprotection during I/R.2 These studies strongly suggest that the generation of free radicals such as O2•– during IPC is necessary to trigger an inherent protective mechanism of preconditioning. The oxygenation and deoxygenation of Mb and the resulting small formation of O2•– identified in our current research likely occurs during IPC. Our identification of Mb as a novel O2•– generator in cardiomyocyte ischemia gives it an anticipated role in cardioprotection for ischemic injuries.
Our result contradicts Schrader and group’s35 previous study, which showed that O2•– production decreased to zero within seconds upon ischemia onset and stayed at such a level until reperfusion. Such a disparity may have been a result of the substantially different technology used in our study compared with that of the Schrader’ experiments. Unlike the experiments conducted by Schrader and group’s35, we utilized a fluorescent probe rather than a chemiluminescence probe lucigenin. Previous research has raised significant concerns on the effectiveness of lucigenin for the detection of O2•–. For instance, in various models, the fluorescent O2•– probes appear to be sensitive in detecting residual O2•– than chemiluminescent probes. Moreover, lucigenin-based measurements of O2•– can cause artifacts in NADPH-rich tissues, such as cardiac or skeletal muscles.36, 37, 38, 39, 40 The fluorescence probe, dihydroethidium (DHE), is highly sensitive and capable of detecting weak intramuscular O2•– signals in both rodent muscle and myocyte models, whereas chemiluminescence is less adapted in detecting small O2•– signals.1, 16, 41, 42, 43, 44, 45 Thus, the fact that O2•– production decreased to zero within seconds upon ischemia in Schrader’s observation may be possibly due to the lack of sensitivity.
Budd et al.46 showed that uncoupler-induced ET fluorescence increase is not due to an increase in O2•– production but results from the collapse of the mitochondrial membrane potential, because oxidized DHE (2-hydroxyethidium and ET) behaves as a mitochondrial membrane potential probe. Thus, their research suggested that the loading concentration of DHE should be kept sufficiently low (i.e., 5 μM) in cell culture or mitochondrial suspensions. This dosage is highly consistent with our former study which used the isolated cardiomyocytes.41 However, Budd et al.46 had a loading condition that was set for the cell culture system (i.e., 5 μM for 10 min); in our study, we were using a rodent heart, which is comprised of hundreds of tissue layers that required high-loading concentrations compared with that of the cell culture. Although we used a range of 1–10 μM of DHE to load the heart, we were unable to detect any signal from the heart during these preliminary tests. Following the previous effective loading protocols for the multilayer muscle tissue,42 our current loading concentration is set higher (44 μM) and the loading time is set much shorter (1.5 min) than those of the cells. This procedure is immediately followed by a 5 min washout, to remove excess dye, and a short ischemia protocol. It is worth noting that former research has also shown that it typically requires a longer time (i.e., 60 min or longer) for a fluorescent probe to successfully load into the mitochondria in cultured cardiomyocytes.47 It is likely that the loading time for mitochondria in the whole heart (used in out experiments) may be even longer. Therefore, it is very unlikely that within such a short period (1.5 min in our assay) the DHE probe has sufficient time to reach the mitochondrial compartment to cause any artificial signals owing to the collapse of mitochondrial membrane potential.
Conclusion and significance
Through the use of SOD mimic, CO treatments, and Mb-knockout techniques, we have identified Mb as a novel O2•– generator in the cardiac myocyte during the onset of ischemia. A small burst of O2•– that was produced by Mb within 20 s of ischemia may be correlated with IPC preconditions, though this mechanism has not been thoroughly investigated. For future studies, other biological techniques such as electron paramagnetic resonance may be used to quantify O2•– signals in this model, and explore a more specific role of Mb in cardiac protection, which facilitates the understanding of the molecular signaling pathways for IPC and O2•– development during ischemia.
Materials and Methods
Rat Langendorff heart perfusion
Male Sprague–Dawley rats weighing ∼350 g were anesthetized with pentobarbital (∼50 mg/kg intraperitoneal injection). After hemithoractomy, hearts were rapidly excised, and aorta were cannulated under retrograde coronary perfusion at 80 mm Hg with Krebs-Henseleit buffer (120.0 mM NaCl, 5.9 mM KCl, 2.5 mM CaCl2, 1.2 mM MgCl2, 16.7 mM glucose, 25.0 mM NaHCO3, 0.5 mM EDTA, bubbled with 95%/5% O2/CO2).1 Hearts were mounted on a Langendorff perfusion apparatus. Each heart was perfused until the recovery of steady cardiac frequency at 37 °C for 15 min. Ischemia was induced by the stopping of the flow of perfusate.
Mb-knockout mice
Mb-knockout (Myo−/−) mice were generated by deletion of the essential genes of Mb in embryonic stem cells, as described previously.48 Mice were genotyped when they were weaned. The experimentation was performed using male mice, and tail clips were kept to reconfirm the genotypes. Both Myo−/− and wild-type mice were heparinized (500 U/kg) and anesthetized via intraperitoneal injection with a combination of ketamine (70 mg/kg) and xylazine (10 mg/kg). After hemithoractomy, hearts were rapidly excised and mounted in a Langendorff perfusion apparatus following the similar protocol to the rat experiments.
Carbon monoxide perfusion
Carbon monoxide (CO) was used to block the O2 binding to Mb. In addition to the Langendorff heart protocol, CO was fully equilibrated with gas sampling tube for 20 min. At 37 °C, Krebs-Henseleit buffer flow rate was 16.2 ml/min and the adjacent tube of CO had a flow rate of 1.8 ml/min. Thus, the overall CO flow rate was set at 10% of the total flow rate, which was 18 ml/min (16.2+1.8=18) for 5 min.
Surface fluorometry
We measured changes in radical formation in the early ischemia in an isolated rodent (rat/mouse) heart. A fiber optic probe was positioned facing the left ventricle in order to obtain an emission signal from the heart. The distance between the heart and cable surface was adjusted to minimize the motion artifact. DHE/ET fluorescence was used as a non-charged O2•–-sensitive probe. DHE (Molecular Probes/Life Technologies, Grand Island, NY, USA) stock was dissolved in N,N-dimethylacetamide (Acros Organics/Thermo Fisher Scientific, Waltham, MA, USA). In response to O2•–, DHE is dehydrogenated, resulting in the formation of 2-hydroxyethidium, which is relatively unstable and converts to a stabilized ET.41, 49 ET is positively charged and has better cellular retention and stability when compared with DHE.42 Therefore, ET formation was chosen as a reliable indicator of O2•– production.43, 44, 46 The ET excitation filter was set at 515±20 nm, and the ET emission was set within a range of 590±25 nm. The emitted fluorescent signal was recorded every 4 s and then transmitted to a computer through an A/D board. A mean fluorescence rate was used to monitor the ET signal change per second at each specific time. A fresh DHE solution was made before dye injection into the heart. Thus, any oxidation of DHE in the solution that bubbled in 95% O2 was kept at a minimal.50 Hearts were perfused with 44 μM DHE for 1.5 min at a perfusion rate of 1 ml/min, followed by a short global ischemia. To confirm that fluorescence was in fact trigged by a burst of O2•– production, a group of hearts were perfused with both the SOD mimic Mn(III)tetrakis(1-methyl-4-pyridyl) porphyrin (MnTMPyP, Enzo Life Sciences/Alexis Biochemicals, Farmingdale, NY, USA; 250 μM) and DHE before ischemia as negative controls.
Confocal study
Langendorff rat hearts were first perfused with a solution of DHE (44 μM) to detect O2•– and fluorescein lectin I-isolectin B4 (FLI-IB4, 0.67 μg/ml, Vector Labs, Burlingame, CA, USA) as a marker for intracellular endothelium for 1.5 min at 1 ml/min. The excess dye was washed out for 5 min with buffer. Hearts were immobilized by an actin–myosin complex blocker 2,3-butanedione monoxime (4 mM; Acros Organics),42 transferred to the confocal microscope stage, and perfused with 37 °C buffer for ∼5 min immediately followed by an ischemic period. The confocal images were recorded when the heart was in an ischemia condition.
The set up for laser scan confocal imaging of O2•– was the following: Laser: argon; objective, × 40 with 1.5-mm working distance; ET excitation, 568 nm; ET emission, long pass (LP, 590 nm). The autofluorescence background was kept minimal in the current settings. Images of the emitted fluorescence signals were captured by a photomultiplier tube and transferred to a computer monitor that displayed them at 512 × 512 pixels for analysis.1, 42
Statistical analysis
Data are expressed as mean±S.E., unless noted otherwise. The statistical significance of differences between groups was calculated using two-way analysis of variance. The P-values of<0.05 were considered significant.
Abbreviations
- I/R:
-
ischemia–reperfusion
- O2•–:
-
superoxide
- IPC:
-
ischemic preconditioning
- ROS:
-
reactive oxygen species
- Fe2+:
-
ferrous heme
- Fe3+:
-
ferric heme
- XO:
-
xanthine oxidase
- Myo−/−:
-
Mb knockout
- WT:
-
wild type
- DHE:
-
dihydroethidium
- ET:
-
ethidium
- SOD:
-
superoxide dismutase
- MnTMPyP:
-
Mn(III)tetrakis(1-methyl-4-pyridyl) porphyrin
- FLI-IB4:
-
fluorescein lectin I-isolectin B4
- RU:
-
relative unit
- RU/s:
-
relative unit per second
- FAD:
-
flavine adenine dinucleotide
- HPC:
-
hypoxic preconditioning
- PI3K:
-
phosphatidylinositol 3-kinase
- KATP channel:
-
ATP potassium channel
- GSK-3β:
-
glycogen synthase kinase-3β
- mPTP:
-
mitochondrial permeability transition pore
References
Zuo L, Chen YR, Reyes LA, Lee HL, Chen CL, Villamena FA et al. The radical trap 5,5-dimethyl-1-pyrroline N-oxide exerts dose-dependent protection against myocardial ischemia-reperfusion injury through preservation of mitochondrial electron transport. J Pharmacol Exp Ther 2009; 329: 515–523.
Zuo L, Roberts WJ, Tolomello RC, Goins AT . Ischemic and hypoxic preconditioning protect cardiac muscles via intracellular ROS signaling. Front Biol 2013; 8: 305–311.
Galaris D, Eddy L, Arduini A, Cadenas E, Hochstein P . Mechanisms of reoxygenation injury in myocardial infarction: implications of a myoglobin redox cycle. Biochemi Biophy Res Commun 1989; 160: 1162–1168.
Galaris D, Cadenas E, Hochstein P . Redox cycling of myoglobin and ascorbate: a potential protective mechanism against oxidative reperfusion injury in muscle. Arch Biochem Biophys 1989; 273: 497–504.
Ordway GA, Garry DJ . Myoglobin: an essential hemoprotein in striated muscle. J Exp Biol 2004; 207 (Pt 20): 3441–3446.
George P, Stratmann CJ . The oxidation of myoglobin to metmyoglobin by oxygen. III. Kinetic studies in the presence of carbon monoxide, and at different hydrogen-ion concentrations with considerations regarding the stability of oxymyoglobin. Biochem J 1954; 57: 568–573.
Reid MB, Haack KE, Franchek KM, Valberg PA, Kobzik L, West MS . Reactive oxygen in skeletal muscle. I. Intracellular oxidant kinetics and fatigue in vitro. J Appl Physiol 1992; 73: 1797–1804.
Yang J, Marden JJ, Fan C, Sanlioglu S, Weiss RM, Ritchie TC et al. Genetic redox preconditioning differentially modulates AP-1 and NF kappa B responses following cardiac ischemia/reperfusion injury and protects against necrosis and apoptosis. Mol Ther 2003; 7: 341–353.
Zweier JL, Kuppusamy P, Williams R, Rayburn BK, Smith D, Weisfeldt ML et al. Measurement and characterization of postischemic free radical generation in the isolated perfused heart. J Biol Chem 1989; 264: 18890–18895.
Thompson-Gorman SL, Zweier JL . Evaluation of the role of xanthine oxidase in myocardial reperfusion injury. J Biol Chem 1990; 265: 6656–6663.
Obal D, Dai S, Keith R, Dimova N, Kingery J, Zheng YT et al. Cardiomyocyte-restricted overexpression of extracellular superoxide dismutase increases nitric oxide bioavailability and reduces infarct size after ischemia/reperfusion. Basic Res Cardiol 2012; 107: 305.
Chen Z, Siu B, Ho YS, Vincent R, Chua CC, Hamdy RC et al. Overexpression of MnSOD protects against myocardial ischemia/reperfusion injury in transgenic mice. J Mol Cell Cardiol 1998; 30: 2281–2289.
Wang P, Chen H, Qin H, Sankarapandi S, Becher MW, Wong PC et al. Overexpression of human copper, zinc-superoxide dismutase (SOD1) prevents postischemic injury. Proc Natl Acad Sci USA 1998; 95: 4556–4560.
Perrelli MG, Pagliaro P, Penna C . Ischemia/reperfusion injury and cardioprotective mechanisms: role of mitochondria and reactive oxygen species. World J Cardiol 2011; 3: 186–200.
Becker LB, vanden Hoek TL, Shao ZH, Li CQ, Schumacker PT . Generation of superoxide in cardiomyocytes during ischemia before reperfusion. Am J Physiol 1999; 277 (6 Pt 2): H2240–H2246.
Zhu X, Zuo L, Cardounel AJ, Zweier JL, He G . Characterization of in vivo tissue redox status, oxygenation, and formation of reactive oxygen species in postischemic myocardium. Antioxid Redox Signal 2007; 9: 447–455.
Brantley RE Jr, Smerdon SJ, Wilkinson AJ, Singleton EW, Olson JS . The mechanism of autooxidation of myoglobin. J Biol Chem 1993; 268: 6995–7010.
Saltman P . On and beyond O2 binding: hemoglobin and myoglobin revisited. Experientia 1995; 51: 205–206.
Zuo L, Clanton TL . Reactive oxygen species formation in the transition to hypoxia in skeletal muscle. Am J Physiol Cell Physiol 2005; 289: C207–C216.
Li JM, Shah AM . Endothelial cell superoxide generation: regulation and relevance for cardiovascular pathophysiology. Am J Physiol Regul Integr Comp Physiol 2004; 287: R1014–R1030.
Lu Q, Wainwright MS, Harris VA, Aggarwal S, Hou Y, Rau T et al. Increased NADPH oxidase-derived superoxide is involved in the neuronal cell death induced by hypoxia-ischemia in neonatal hippocampal slice cultures. Free Radic Biol Med 2012; 53: 1139–1151.
Suh SW, Shin BS, Ma H, Van Hoecke M, Brennan AM, Yenari MA et al. Glucose and NADPH oxidase drive neuronal superoxide formation in stroke. Ann Neurol 2008; 64: 654–663.
Linas SL, Whittenburg D, Repine JE . Role of xanthine oxidase in ischemia/reperfusion injury. Am J Physiol 1990; 258 (3 Pt 2): F711–F716.
Turrens JF . Mitochondrial formation of reactive oxygen species. J Physiol 2003; 552 (Pt 2): 335–344.
Braunlin EA, Wahler GM, Swayze CR, Lucas RV, Fox IJ . Myoglobin facilitated oxygen diffusion maintains mechanical function of mammalian cardiac muscle. Cardiovasc Res 1986; 20: 627–636.
Gunther MR, Sampath V, Caughey WS . Potential roles of myoglobin autoxidation in myocardial ischemia-reperfusion injury. Free Radic Biol Med 1999; 26: 1388–1395.
Cooper CE, Brown GC . The inhibition of mitochondrial cytochrome oxidase by the gases carbon monoxide, nitric oxide, hydrogen cyanide and hydrogen sulfide: chemical mechanism and physiological significance. J Bioenerg Biomembr 2008; 40: 533–539.
Raedschelders K, Ansley DM, Chen DD . The cellular and molecular origin of reactive oxygen species generation during myocardial ischemia and reperfusion. Pharmacol Ther 2012; 133: 230–255.
Roberts WJ, Zuo L . Hypoxic preconditioning reduces reoxygenation injuries via PI3K in respiratory muscle. GSTF JBio 2012; 2: 42–53.
Juhaszova M, Zorov DB, Kim SH, Pepe S, Fu Q, Fishbein KW et al. Glycogen synthase kinase-3beta mediates convergence of protection signaling to inhibit the mitochondrial permeability transition pore. J Clin Invest 2004; 113: 1535–1549.
Tong H, Imahashi K, Steenbergen C, Murphy E . Phosphorylation of glycogen synthase kinase-3beta during preconditioning through a phosphatidylinositol-3-kinase—dependent pathway is cardioprotective. Circ Res 2002; 90: 377–379.
Liu Y, Sato T, O'Rourke B, Marban E . Mitochondrial ATP-dependent potassium channels: novel effectors of cardioprotection? Circulation 1998; 97: 2463–2469.
Schulz R, Cohen MV, Behrends M, Downey JM, Heusch G . Signal transduction of ischemic preconditioning. Cardiovasc Res 2001; 52: 181–198.
Pain T, Yang XM, Critz SD, Yue Y, Nakano A, Liu GS et al. Opening of mitochondrial K(ATP) channels triggers the preconditioned state by generating free radicals. Circ Res 2000; 87: 460–466.
Flogel U, Godecke A, Klotz LO, Schrader J . Role of myoglobin in the antioxidant defense of the heart. FASEB J 2004; 18: 1156–1158.
Tarpey MM, Wink DA, Grisham MB . Methods for detection of reactive metabolites of oxygen and nitrogen: in vitro and in vivo considerations. Am J Physiol Regul Integr Comp Physiol 2004; 286: R431–R444.
Li Y, Zhu H, Kuppusamy P, Roubaud V, Zweier JL, Trush MA . Validation of lucigenin (bis-N-methylacridinium) as a chemilumigenic probe for detecting superoxide anion radical production by enzymatic and cellular systems. J Biol Chem 1998; 273: 2015–2023.
Liochev SI, Fridovich I . Lucigenin luminescence as a measure of intracellular superoxide dismutase activity in Escherichia coli. Proc Natl Acad Sci USA 1997; 94: 2891–2896.
Vasquez-Vivar J, Hogg N, Pritchard KA Jr., Martasek P, Kalyanaraman B . Superoxide anion formation from lucigenin: an electron spin resonance spin-trapping study. FEBS Lett 1997; 403: 127–130.
Barbacanne MA, Souchard JP, Darblade B, Iliou JP, Nepveu F, Pipy B et al. Detection of superoxide anion released extracellularly by endothelial cells using cytochrome c reduction, ESR, fluorescence and lucigenin-enhanced chemiluminescence techniques. Free Radic Biol Med 2000; 29: 388–396.
Zuo L, Youtz DJ, Wold LE . Particulate matter exposure exacerbates high glucose-induced cardiomyocyte dysfunction through ROS generation. PLoS One 2011; 6: e23116.
Zuo L, Christofi FL, Wright VP, Liu CY, Merola AJ, Berliner LJ et al. Intra- and extracellular measurement of reactive oxygen species produced during heat stress in diaphragm muscle. Am J Physiol Cell Physiol 2000; 279: C1058–C1066.
Al-Mehdi AB, Shuman H, Fisher AB . Intracellular generation of reactive oxygen species during nonhypoxic lung ischemia. Am J Physiol 1997; 272 (2 Pt 1): L294–L300.
Nethery D, Stofan D, Callahan L, DiMarco A, Supinski G . Formation of reactive oxygen species by the contracting diaphragm is PLA(2) dependent. J Appl Physiol 1999; 87: 792–800.
Zuo L, Clanton TL . Detection of reactive oxygen and nitrogen species in tissues using redox-sensitive fluorescent probes. Methods Enzymol 2002; 352: 307–325.
Budd SL, Castilho RF, Nicholls DG . Mitochondrial membrane potential and hydroethidine-monitored superoxide generation in cultured cerebellar granule cells. FEBS Lett 1997; 415: 21–24.
Christensen ML, Braunstein TH, Treiman M . Fluorescence assay for mitochondrial permeability transition in cardiomyocytes cultured in a microtiter plate. Anal Biochem 2008; 378: 25–31.
Godecke A, Flogel U, Zanger K, Ding Z, Hirchenhain J, Decking UK et al. Disruption of myoglobin in mice induces multiple compensatory mechanisms. Proc Natl Acad Sci USA 1999; 96: 10495–10500.
Zielonka J, Hardy M, Kalyanaraman B . HPLC study of oxidation products of hydroethidine in chemical and biological systems: ramifications in superoxide measurements. Free Radic Biol Med 2009; 46: 329–338.
Napankangas JP, Liimatta EV, Joensuu P, Bergmann U, Ylitalo K, Hassinen IE . Superoxide production during ischemia-reperfusion in the perfused rat heart: a comparison of two methods of measurement. J Mol Cell Cardiol 2012; 53: 906–915.
Acknowledgements
This work was supported in part by OSU-HRS Fund 013000, by OSU research resources from HRS and DHLRI, by OU General Fund G110 and Research Excellence Fund of Biomedical Research, by Shanghai Ruijin Hospital (China), and by UCSD research resources. We especially acknowledge the assistance of Allison Hallman for research support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Finazzi-Agró
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Zhu, X., Zuo, L. Characterization of oxygen radical formation mechanism at early cardiac ischemia. Cell Death Dis 4, e787 (2013). https://doi.org/10.1038/cddis.2013.313
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2013.313
Keywords
This article is cited by
-
Protective effect of canagliflozin on post-resuscitation myocardial function in a rat model of cardiac arrest
Intensive Care Medicine Experimental (2023)
-
Role of hypoxia in cancer therapy by regulating the tumor microenvironment
Molecular Cancer (2019)
-
The mechanisms of air pollution and particulate matter in cardiovascular diseases
Heart Failure Reviews (2017)