Abstract
Remodeling of the remnant neuronal network after brain injury possibly mediates spontaneous functional recovery; however, the mechanisms inducing axonal remodeling during spontaneous recovery remain unclear. Here, we show that altered γ-aminobutyric acid (GABA) signaling is crucial for axonal remodeling of the contralesional cortex after traumatic brain injury. After injury to the sensorimotor cortex in mice, we found a significant decrease in the expression of GABAAR-α1 subunits in the intact sensorimotor cortex for 2 weeks. Motor functions, assessed by grid walk and cylinder tests, spontaneously improved in 4 weeks after the injury to the sensorimotor cortex. With motor recovery, corticospinal tract (CST) axons from the contralesional cortex sprouted into the denervated side of the cervical spinal cord at 2 and 4 weeks after the injury. To determine the functional implications of the changes in the expression of GABAAR-α1 subunits, we infused muscimol, a GABA R agonist, into the contralesional cortex for a week after the injury. Compared with the vehicle-treated mice, we noted significantly inhibited recovery in the muscimol-treated mice. Further, muscimol infusion greatly suppressed the axonal sprouting into the denervated side of the cervical spinal cord. In conclusion, recovery of motor function and axonal remodeling of the CST following cortical injury requires suppressed GABAAR subunit expression and decreased GABAergic signaling.
Similar content being viewed by others
Main
Activity in the motor cortex sometimes spontaneously recovers, to a limit, despite deleterious loss of motor function after injury. Reorganization of the neural network in the spared regions accompanies this functional recovery.1 The motor cortex on the unaffected side may have a compensatory role to restore the lost motor function.2 Subcortical efferent projections from the intact cortex including the corticospinal tract (CST) exhibit plastic changes following injury.3 CST axons newly sprout into the denervated (lesion) subcortical areas at multiple levels of the brain and spinal cord.4, 5 Intriguingly, treatments that induce axonal growth promote functional recovery.4 Rewiring of the neural network may be responsible for the therapeutic effects of these treatments. However, the mechanisms that induce axonal remodeling during such spontaneous recovery remain unclear.
To obtain mechanistic insights into axonal remodeling in the contralesional cerebral cortex, we sought information on alterations in gene expression after cortical injury. Following injury, the perilesional and contralesional motor cortices exhibit downregulation of the γ-aminobutyric acid type A receptor (GABAAR) and upregulation of the N-methyl-D-aspartate receptor.6, 7, 8 Increased neuronal excitability accompanies changes in the expressions of these proteins in the perilesional areas.9 Here, we hypothesize that the increased neuronal excitability induced by decreased GABAergic signaling leads to axonal remodeling of the intact CST, thereby contributing to functional recovery.
Results
Changes in mRNA expression of GABAAR subunits in the contralesional cortex
We employed a murine model to elucidate the role of GABAergic signaling in neuronal reorganization and functional recovery after traumatic cortical injury. We first investigated the gene expression patterns of each GABAAR subunit in the contralesional cortex following the injury by real-time reverse transcriptase (RT)-PCR. Most GABAARs are heteropentamers composed of isoforms of α-, β-, γ-, and δ- subunits; the most common subtype is α1β2γ2.10, 11 Among the six isoforms of the α-subunit, the mRNA of the α1 isoform in the injured mice compared with the sham mice significantly decreased at 7 days after the injury (Figure 1a, P<0.05). Further, the mRNA expression of the γ2 subunit significantly decreased in the injured group (Figure 1c, P<0.05). On the other hand, the mRNA expressions of the other α-isoforms (Figure 1a), all β-isoforms (Figure 1b), other γ-isoforms, and δ-subunit (Figure 1c) in the contralesional cortex did not change after the injury. Therefore, the mRNA expressions of the α1 and γ2 subunits in the contralesional cortex specifically decreased after the injury.
Downregulation of GABAAR subunit expressions in the contralesional cortex after traumatic brain injury. (a–c) Quantification of the mRNA expression of GABAAR subunits (α (a), β (b), and γ and δ (c) subunits) in the contralesional cortex at 7 days after brain injury (by real-time PCR). The fold change of the injured group (black bars) relative to the sham group (gray bars) is shown as the mean±S.D. (n=3, each group). (d) Western blots of the GABAAR-α1 subunit and NCAM (internal control) in the contralesional cortex at 1, 2, and 4 weeks after the injury. (e) Quantification of GABAAR-α1 protein expression in d. The expression significantly decreased at 1 and 2 weeks after the injury. (n=6, each group). *P<0.05 (Mann–Whitney U-test)
Temporal downregulation of GABAAR-α1 protein expression in the contralesional cortex
To assess the time course of the protein expression of the GABAAR-α1 subunit in the contralesional cortex, western blotting was performed with both sham and injured mice at 1, 2, and 4 weeks after the injury. Consistent with the gene expression pattern (Figure 1a), the protein level of the GABAAR-α1 subunit (about 51 kDa) decreased after the injury (Figure 1d). For quantification, the mean values of this protein level normalized to the expression level of neural cell adhesion molecule (NCAM) were compared between the sham and the injured mice (Figure 1e). At 1 and 2 weeks after the injury, the protein level of the GABAAR-α1 subunit significantly decreased in the injured mice (Figure 1e, P<0.05). However, the level returned to the control level at 4 weeks after the injury (Figure 1e).
We further investigated the localization of the GABAAR-α1 subunit in the contralesional cortex by immunohistochemical staining. The GABAAR-α1 subunit was expressed and localized in all six cortical layers (Figure 2a). At 2 weeks after the injury, the immunoreactivity for the GABAAR-α1 subunit significantly decreased in all the layers (Figures 2a and b). At 4 weeks after the injury, the expression in layers II, III, and V, in which pyramidal corticospinal neurons localize, was still downregulated compared with that in the sham group, but the expression in layers I, IV, and VI returned to the control level (Figure 2c). Thus, GABAAR-α1 subunit expression was downregulated in neurons of the contralesional cortex after brain injury.
Downregulation of GABAAR subunit expressions in the cortical neurons after traumatic brain injury. (a) Immunohistochemical staining of the GABAAR-α1 subunit (green) and Nissl staining (magenta) in the contralesional cortex of the injured mice at 2 weeks after the injury. GABAAR-α1-positive signals decreased in all the layers in injured group. Scale bar: 50 μm. (b and c) Quantification of GABAAR-α1-positive signals by immunohistochemical staining at 2 (b) and 4 weeks (c) after the injury. The data represent the mean±S.D. (n=3, each group); *P<0.05, **P<0.01 versus the sham mice (Mann–Whitney U-test)
Spontaneous functional recovery of impaired forelimbs diminished by muscimol infusion
The temporal downregulation of GABAAR-α1 subunit expression in the contralesional cortex suggests that the activity of these neurons was upregulated. Actually, we found elevated expression of one neuronal activity-dependent gene, alivin-1,12 in the contralesional cortex (Supplementary Figure 1E). Thus, we next tried to explore the functional implications of this phenomenon. In accordance with previous reports,3 the injured mice showed spontaneous functional recovery after the initial motor deficits. We assessed the functional recovery with two motor tests. Although the ability to walk on a grid was severely impaired at one day after the injury, it gradually improved until 4 weeks after the injury (Figure 3a). In the cylinder test, the injured mice showed significant forelimb-use asymmetries for vertical exploration during the first week after the injury, especially reduced use of the impaired left forelimb (Figure 3b, P<0.01). The independent or simultaneous use of the impaired forelimb gradually increased until 4 weeks after the injury, indicating that the function of this forelimb spontaneously recovered (Figure 3b).
Spontaneous recovery of motor function after brain injury is suppressed by muscimol infusion into the contralesional cortex. (a and b) Spontaneous recovery of forelimb motor function in the grid walk (a) and cylinder (b) tests (sham group, dotted line; injured group, solid line; n=7, each group). (c and d) Inhibition of spontaneous recovery of forelimb motor function by muscimol infusion in the grid walk (c) and cylinder (d) tests (saline-treated group, dotted line; muscimol-treated group, solid line). The data represent the mean±S.D. (vehicle n=7, muscimol n=12); *P<0.05, **P<0.01 versus the controls (two-way repeated measure ANOVA followed by Tukey–Kramer test)
We then investigated whether the downregulation of GABAergic signals in the contralesional hemisphere contributes to the functional recovery following the injury. Muscimol or saline was infused into the forelimb region of contralesional cortex for 7 days after the injury (days 3–10). Muscimol treatment induced no behavioral abnormality in the ipsilateral limbs of the mice without cortical injury, but the contralateral limbs showed transient impairment (data not shown). Further, in the grid walk test, two-way repeated measure ANOVA showed that the values in the muscimol-treated group were overall statistically different from those of the vehicle group (P<0.01), and post hoc analysis showed that the differences at day 7 were significant (Figure 3c). The unaffected (right) forelimb also had transient impairment during muscimol infusion (Supplementary Figure 1B), indicating that muscimol was effective in these experiments. In the cylinder test, the muscimol-treated mice used their unaffected forelimb to support their bodies more frequently than the saline-treated mice (Figure 3d). The muscimol-treated group had statistically lower function than the vehicle group (P<0.01, two-way repeated measures ANOVA). At 4 weeks after the injury, the muscimol-treated group had significantly lower use ratio of the affected side than the saline-treated group (P<0.05, Figure 3d). In both tests, although there were significant differences of motor functions between muscimol and vehicle-treated group by two-way repeated measure ANOVA (P<0.01), the difference regarding with the time course was different. It is possible that both tests would measure different aspects of recovery in motor functions. Overall, the results indicated that the muscimol treatment inhibited the spontaneous motor recovery following the cortical injury.
The cortical lesion volume induced by the injury did not differ between the muscimol-treated and the saline-treated groups at 4 weeks (Supplementary Figure 1C; muscimol infusion, 6.3±1.2 mm3; saline infusion, 6.6±1.8 mm3). Further, muscimol infusion did not lead to any apparent histological damage in the infused (contralesional) cortex (Supplementary Figure 1D). As muscimol was infused from 3 to 10 days after the injury (no effect of muscimol was observed at day 14; Supplementary Figure 1B), inactivation of GABARs in this period was important for motor recovery.
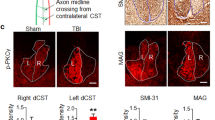
Enhanced GABA activation by muscimol infusion disrupted rewiring of CST fibers
The rewiring of intact corticofugal fibers, especially CST fibers, from the contralesional cortex is a main source of neuronal reorganization contributing to functional recovery after brain injury.3 As the expression of the GABAAR-α1 subunit in layer V neurons including corticospinal neurons decreased (Figures 2a–c), we hypothesized that downregulation of GABAergic signaling in these neurons is necessary for enhanced axonal plasticity. To address this hypothesis, we first investigated whether CST fibers showed increased sprouting into the denervated gray matter of the cervical cord after the injury (Figure 4a). The number of biotinylated dextran amine (BDA)-labeled CST fibers recrossing the midline of the cervical cord was counted. At 2 weeks after the injury, the number of recrossing CST fibers significantly increased (Figures 4b and c). Further, quantification analysis revealed that the number of crossing CST fibers at 2 weeks increased at the C5–C7 levels (Figure 4f, P<0.05). At 4 weeks after the injury, we observed a large number of crossing fibers at the C7 level in the injured mice compared with the sham mice (Figures 4d, e and g, P<0.05). There were more sprouts at 2 weeks than that at 4 weeks after the injury, suggesting that progressive sprout elimination and remodeling of connections had occurred.13 The results supported the notion that rewiring of CST fibers contributed to the functional recovery of motor function in the impaired forelimbs.
Increased number of midline-crossing CST fibers in the cervical spinal cord after traumatic brain injury. (a) Illustration of midline-crossing (recrossing) CST fibers after cortical injury. BDA (green) was injected into the contralesional cortex (blue) to label the CST. The BDA-labeled CST fibers sprouted and recrossed to the denervated side of the cervical spinal cord after injury (green arrows). The recrossing fibers were counted from C4 to C7. (b–e) Photographs of recrossing CST fibers labeled with BDA (green) at the C7 level in the sham (b and d) and injured (c and e) mice at 2 (b and c) and 4 (d and e) weeks after the injury (Z stack, each 0.5 μm, by confocal laser-scanning microscopy). The recrossing CST fibers were marked with arrowheads. Scale bar: 50 μm. (f and g) Quantification of the recrossing CST fibers at each cervical level 2 (f) and 4 (g) weeks after the injury. The fibers increased in the injured group (black bars) compared with the sham group (gray bars). The data represent the mean±S.D. (2 weeks: sham n=6, injury n=4, 4 weeks: sham n=5, injury n=4); *P<0.05 (Mann–Whitney U-test)
We then tried to investigate whether enhanced GABAergic signaling affected the sprouting of CST fibers from the contralesional cortex. We counted the number of midline-crossing CST fibers in the cervical cord at 4 weeks after the injury in the mice treated with muscimol or saline (Figures 5a and b). Fewer CST fibers crossed at the C5–C7 levels in the muscimol-treated group than in the saline-treated group (Figure 5c), although almost the same number as that in the sham group was counted (Figures 4d and g). Further, the extent of growth of the crossing fibers was assessed by measuring the BDA-positive areas in the denervated gray matter. Consistent with the decreased number of recrossing axons (Figure 5c), administration of muscimol significantly inhibited axonal outgrowth into the denervated gray matter at all the cervical levels examined (Figure 5d). These results demonstrated that suppression of GABAergic signaling was necessary for reorganization of the CST after cortical injury.
Sprouting of CST fibers is inhibited by muscimol infusion in the contralesional cortex after brain injury. (a and b) Photographs of the recrossing CST fibers labeled with BDA at the C7 level in the saline-treated (a) or muscimol-treated (b) mice (Z stack, each 0.5 μm, by confocal laser-scanning microscopy). The recrossing CST fibers were marked with arrowheads. Scale bar: 50 μm. (c and d) Quantification of the number of recrossing CST fibers (c) and their positive areas in the denervated cervical spinal cord (d) at each cervical level in the saline-treated (gray bars) and muscimol-treated (black bars) mice at 4 weeks after the injury. Muscimol infusion decreased the number of sprouting axons into the denervated side. The data represent the mean±S.D. (n=5, each group); *P<0.05, **P<0.01 versus the saline-treated mice (Mann–Whitney U-test)
Discussion
Here, we have shown that downregulation of GABAergic signaling after traumatic brain injury in mice is necessary for rewiring of the CST and spontaneous recovery of motor function. Interestingly, when muscimol was infused from days 3 to 10 after the injury, the recovery of motor function and CST rewiring was significantly suppressed at 28 days. Thus, the period of GABAergic signal downregulation is important for neuronal plasticity and the following recovery. Indeed, this period overlaps the time window of neuronal plasticity after ischemic brain injury.14
Although functional deficits do not completely recover after central nervous system damage, partial recovery of function occurs after cortical injury in human and animals, with plastic changes in the neuronal network. For example, dendritic remodeling such as dendritic arborization and spine formation occurs in periinfarct areas.15, 16 Dendritic spine formation significantly increases, peaking at 1–2 weeks, and persists for up to 6 weeks in the periinfarct cortex.15 Further, sprouting of efferent fibers from the contralesional cortex increases on the denervated side of subcortical areas such as the red nucleus and cervical spinal cord after brain injury.4, 5, 17 Interestingly, rehabilitation and neuronal activity can contribute to promotion of these structural changes.18, 19, 20 Hence, neuronal activity might be the key regulator of axonal growth, branch initiation, and neuronal reorganization.21, 22 In this case, it is conceivable that downregulation of GABA signaling might facilitate the activation of neurons and following plastic changes in our model.
Spontaneous recovery after the cortical injury was observed to the large extent during the early phase (up to a week) in the grid walk test, whereas that was observed during the late phase in the cylinder test (Figures 3a and b). Although there were significant differences in the improvement of motor functions between muscimol-treated and vehicle-treated mice, the time points, when the significantly suppressed functional recovery was observed in the muscimol-treated mice, were different in these two tests (Figures 3c and d). The effect of muscimol appears to be significant when the spontaneous recovery rate of the function was maximal in these tests. Therefore, downregulation of GABAergic signaling in the contralateral side cortex may be required for the specific phase of the functional recovery. Reorganization of multiple tracts, including CST, corticorubro tract, corticoreticulo tract, and cortico-cortico pathways, is considered to be required for the functional recovery after the cortical injury. Thus, reorganization of other tracts, other than the CST may work for the functional recovery during the time course when we observed no significant effect of muscimol treatment in each functional test.
GABA is the major inhibitory neurotransmitter controlling the excitation and activity of neurons. The major type of GABAR in vertebrate neurons is a member of the ligand-gated ion channel family of receptors. The GABAAR forms a heterooligomeric complex assembled from a range of homologous subunits sharing a common structure. To date, 18 GABAAR subunits have been identified.23 The local GABA circuits target specific subdomains on nearby pyramidal cells, such as the somaproximal dendritic region or axonal initial segment.24, 25 The somaproximal dendritic region but not the axonal initial segment is rich in the GABAAR-α1 subunit, which is located on the opposite side of synaptic boutons of parvalbumin-positive GABAergic neurons.24, 26 In addition, the GABAAR at the somaproximal dendritic region may be more effective to inhibit neuronal activation than inhibition at the dendritic shaft.27 Hence, downregulation of the GABAAR-α1 subunit would decrease the inhibitory signal to glutamatergic neurons, resulting in enhancement of excitatory signals.
Changes in GABAAR-α1 gene expression have been demonstrated in other animal models of epilepsy, alcohol abuse and withdrawal, and swim stress.28, 29, 30, 31 In neocortical neurons, activation of protein kinase C increases GABAAR-α1 subunit expression via phosphorylation of the cAMP-response element-binding protein bound to the GABAAR-α1 subunit promoter.32 On the other hand, decreased GABAAR-α1 expression depends on the inducible cAMP early repressor.32 Another report indicated that the Janus kinase/signal transducer and activator of transcription pathway regulated by the brain-derived neurotrophic factor mediate seizure-induced decrease of GABAAR-α1 subunit expression in epilepsy.33 Although the mechanism of downregulation in GABAAR-α1 expression is still unclear in our brain injury model, these neuronal activity-related genes might be involved.
Revealing the mechanism of spontaneous compensatory motor recovery on a neural basis is important to develop new therapies for brain injury. Our study reveals that altering GABAergic signaling may be a good therapeutic target to treat patients with brain injury.
Materials and Methods
Surgical procedures for traumatic cortical injury
All experiments were conducted in accordance with the Osaka University Medical School Guide for the Care and Use of Laboratory Animals and were approved by the institutional committee of Osaka University. Eight-week-old male C57BL/6J mice (Charles River Japan, Osaka, Japan) were anesthetized with intraperitoneal sodium pentobarbital (Somnopentyl, 50 mg/kg body weight; Kyouritu Seiyaku, Tokyo, Japan) and then individually placed in a stereotaxic frame for surgery. After a midline incision of the scalp, circular craniotomy (4 mm in diameter) was performed over the right parietal cortex with the center at 0 mm anteroposterior and 2 mm lateral to the bregma. The animal was positioned in a head holder and then subjected to traumatic cortical injury by using a pneumatic cortical impact device (AmScien Instruments, Richmond, VA, USA) with a 3-mm convex tip oriented perpendicular to the cortical surface.34 The impact parameters were 4-mm/ms velocity, 1-mm depth, and 120-ms total time. The injured area covered primary forelimb and hindlimb motor area, premotor area, and sensory area of mouse cortex.35 Sham-operated mice received a circular craniotomy, and the parietal cortex was exposed. The scalp was then sutured and the animal was allowed to awaken from the anesthesia. The mice were maintained according to a 12-h light/dark cycle with ad libitum access to food and water.
Quantitative real-time RT-PCR
Total ribonucleic acid (RNA) was extracted from the contralesional cortex (n=3) by using TRIzol reagent (Molecular Probes, Invitrogen, Eugene, OR, USA) at 7 days after the injury and was reverse-transcribed for first-strand complementary (cDNA) synthesis with an oligo(dT) primer and SuperScript II RNase H-reverse transcriptase (Invitrogen). Real-time PCR was performed with oligonucleotide primer sets corresponding to the cDNA sequences of the GABAAR subunits (α, β, γ, and δ), glyceraldehyde-3-phosphate dehydrogenase (GAPDH; Table 1), and alivin-1 (Supplementary Table 1). In brief, 20 μl of a reaction mixture containing 10-μl SYBR Green real-time PCR master mix (Applied Biosystems, Warrington, UK), 1–2 μl each of the sense and anti-sense primers (10 μM), and 1 μl of the cDNA sample (10 ng/μl) was preheated at 95°C for 3 min and then treated with 40 cycles of amplification (denaturation at 95°C for 15 s, annealing and extension at 60°C for 1 min) in an ABI PRISM 7900HT sequence detection system (Applied Biosystems). The relative intensity against GAPDH and the fold change relative to the control were calculated.
Western blot analysis
At 7, 14, and 28 days after the injury, some mice (n=6) were deeply anesthetized and transcardially perfused with chilled saline. Their brains were rapidly removed and the cortical regions contralateral to the injured site (3 × 3 mm2) were sampled. The samples were frozen in liquid nitrogen and stored −80°C until use. Plasma membrane fractionation for detecting GABAAR-α1 subunits was conducted with a plasma membrane protein extraction kit (BioVision, Mountain View, CA, USA). The samples were separated on 10% sodium dodecyl sulfate-polyacrylamide gels with 4.5% stacking gel. Protein was then electrotransferred onto nitrocellulose membranes. The membranes were incubated for 1 h in 0.01 M phosphate-buffered saline (PBS) containing 5% non-fat dry milk at room temperature. They were rinsed briefly in 0.05% Tween 20 in PBS and then incubated overnight at 4°C with rabbit polyclonal anti-GABAAR-α1 antibody (1 : 2000; Covance, Emeryville, CA, USA) and mouse monoclonal anti-neural cell adhesion molecule (NCAM) antibody (1 : 1000; Sigma, St. Louis, MO, USA). Horseradish peroxidase-conjugated secondary antibody (1 : 5000; Cell Signaling Technology, Danvers, MA, USA) and an ECL chemiluminescence system (GE Healthcare, Buckinghamshire, UK) were used for detection.
Histological and immunohistochemical analyses
At 7, 14, and 28 days after the injury, some mice (n=3) were deeply anesthetized and then transcardially perfused with 4% paraformaldehyde (PFA) in PBS. Their brains and cervical spinal cords were removed and fixed in 4% PFA at 4°C overnight and then cryoprotected in 30% sucrose for 3 days. The tissues were embedded in optimal cutting temperature compound (Tissue-Tek, SAKURA Finetek, Tokyo, Japan) and stored at −80°C. Sections of the brain and spine (20-μm thickness) were cut coronally on a cryostat and mounted on Matsumami adhesive silane-coated slides (Matsumami Glass, Osaka, Japan). The sections were rinsed in PBS, blocked in 0.1% Triton X-100 and 5% bovine serum albumin (BSA) in PBS for 1 h, and incubated with rabbit polyclonal GABAAR-α1 antibody (1 : 100; Covance) in 5% BSA in PBS overnight at 4°C. They were then washed with PBS and incubated with Alexa Fluor 488 or 568 conjugated goat anti-rabbit immunoglobulin G (1 : 100; Invitrogen) in 5% BSA in PBS for 1 h. The sections were counterstained with NeuroTrace Nissl stain (1 : 100, Invitrogen) for neuronal markers. All the sections were observed by fluorescence microscopy (Olympus BX51, DP71, Olympus, Tokyo, Japan) or confocal laser-scanning microscopy (Olympus FluoView FV1000, Olympus). For semiquantitative image analysis of GABAAR-α1 subunits, we used a modified method of Redecker et al.7 In brief, measure of relative optical density of GABAAR-α1 subunit staining was performed on one section per animal. Three areas of each layer in the forelimb region of the contralesional motor cortex were photographed by using a confocal laser-scanning microscope (magnification, × 600) and the images were processed with ImageJ (National Institutes of Health, Bethesda, MD, USA).
For analysis of the cortical lesion volume, tissue sections were obtained at every 100 μm and stained with Nissl stain (cresyl violet; Sigma) or hematoxylin and eosin. Each section was digitalized by using a charge-coupled device camera and the cavity area in each section was measured by using ImageJ. On each image, the cavity was outlined with the polygon selection tool by visual inspection, with the dorsal aspect of the lesion estimated from mirror image of the contour of the uninjured hemisphere. The total volume of the cortical cavity was calculated by integrating the measured area from each section.34 The average volume was 6.28±2.0 mm3.
Anterograde labeling of the CST
At 0 or 2 weeks after the injury, BDA (10% in PBS, molecular weight 10 000; Invitrogen) was injected into the left motor cortex (1.2 μl per cortex; 0–0.5 mm anterior and 1–1.5 mm lateral to the bregma, 0.5-mm depth) under anesthesia to label CST fibers. During each injection, 0.2 μl of BDA was delivered for 30 s via a glass capillary (inner diameter, 15–20 μm) attached to a microliter syringe (ITO, Shizuoka, Japan). Fourteen days after BDA injection, the animals were sacrificed by perfusion with 4% PFA. The cervical spinal cords were sampled, post-fixed overnight in the same fixatives, and cryopreserved in 30% sucrose in PBS. They were embedded in TissueTek OCT compound (SAKURA Finetek). The blocks were sectioned coronally (20 μm) from vertebrae C4 to C7. The sections were incubated in 0.3% Triton X-100 in PBS for 4 h and then incubated for 2 h with Alexa Fluor 488-conjugated streptavidin (1 : 400; Invitrogen) in PBS at room temperature.36
Muscimol treatment
Supplementary Figure 1 illustrates the experimental procedures for the muscimol treatment. A stainless steel cannula (Brain infusion kit 3; Alzet, Cupertino, CA, USA) connected to a microosmotic pump (model 1004; Alzet) was implanted in the forelimb area of the left motor cortex (1.0 mm anterior and 1.0 mm lateral to the bregma, 0.65-mm depth from the cortical surface) at 3 days after the injury. For reliable infusion, the cannula was implanted slightly deeper than BDA infusion, because the cannula is thicker than the glass capillary for BDA infusion. Muscimol (10 mM in saline; Sigma), a GABA R agonist, was infused continuously for 7 days (days 3–10; 0.11 μl/h).37, 38 Saline (Otsuka, Tokyo, Japan) was administered as a control.39 To assess the histological changes caused by muscimol infusion, cryosections (20 μm) of the infused cortex (1 mm anterior and 1 mm lateral to the bregma) were stained with hematoxylin and eosin (Supplementary Figure 1D).
Grid walk test
The grid walk test assesses the ability to place the forepaws accurately on the rungs of a grid during spontaneous exploration. The mice were placed on a grid of 0.24 × 0.2 m (length × width) with 10-mm2 openings to explore freely for 4 min. Step errors were videotaped with a camera placed underneath the grid. We counted a step failure when the limb did not bear the body weight and the foot slipped through the grid hole.40 The percentage step failure was calculated by the formula (step failure/50 steps) × 100. The test was performed once a day from a day to 4 weeks after the injury.
Cylinder test
The cylinder test evaluates forelimb use during spontaneous vertical exploration within a cylinder. The mice were placed in a cylinder (115-mm height and 80-mm diameter), and the number of times each forelimb or both forelimbs were used to support the body on the wall of the cylinder was counted. Two mirrors were set behind the cylinder to view all directions. The behaviors were videotaped and the total behaviors of 20 tests were scored.16
Quantification of midline-crossing CST fibers
The number of BDA-labeled midline-crossing CST fibers in the cervical spinal cord was compared between the sham and the injured mice with saline and muscimol treatment, respectively. For quantification, the number of fibers crossing the midline (see Figures 4a–e; arrowheads) was counted by using a fluorescence microscope (final magnification, × 400) in 20 cross-sections (20 μm) per cervical (C4–C7) level. To correct variations in BDA uptake of CST neurons in the motor cortex among the animals, the number of midline-crossing axons was normalized by the number of BDA-labeled dorsal CST fibers, the main pyramidal tract, in the first section at the C4 level, photographed by confocal laser-scanning microscopy (magnification, × 600). The results were calculated as the percentage of the total number of dorsal CST fibers. To quantify the density of crossing CST fibers, 10 cross-sections at each cervical (C4–C7) level were photographed (magnification, × 100) and the BDA-positive areas in the affected and contralesional gray matter were measured by using ImageJ. These results were calculated as the ratio of positive areas in the affected (denervated) gray matter to those in the contralesional gray matter.
Statistical analysis
All data represent the mean±S.D. For mRNA and protein expressions, and data of BDA-labeled crossing CST fibers, non-parametric Mann–Whitney U-test was used for comparisons of groups. All behavioral scores were evaluated using a two-way repeated measure ANOVA to detect significant differences between and among treatment groups; Tukey–Kramer post hoc analysis was used to determine where those differences occurred. P<0.05 was considered significant.
Abbreviations
- GABA:
-
γ-aminobutyric acid
- CST:
-
corticospinal tract
- GABAAR:
-
γ-aminobutyric acid type A receptor
- RT-PCR:
-
reverse transcriptase PCR
- cDNA:
-
complementary DNA
- GAPDH:
-
glyceraldehyde-3-phosphate dehydrogenase
- PBS:
-
phosphate-buffered saline
- NCAM:
-
neural cell adhesion molecule
- PFA:
-
paraformaldehyde
- BDA:
-
biotinylated dextran amine
References
Cramer SC, Crafton KR . Somatotopy and movement representation sites following cortical stroke. Exp Brain Res 2006; 168: 25–32.
Murphy TH, Corbett D . Plasticity during stroke recovery: from synapse to behaviour. Nat Rev Neurosci 2009; 10: 861–872.
Benowitz LI, Carmichael ST . Promoting axonal rewiring to improve outcome after stroke. Neurobiol Dis 2010; 37: 259–266.
Lee JK, Kim JE, Sivula M, Strittmatter SM . Nogo receptor antagonism promotes stroke recovery by enhancing axonal plasticity. J Neurosci 2004; 24: 6209–6217.
Omoto S, Ueno M, Mochio S, Takai T, Yamashita T . Genetic deletion of paired immunoglobulin-like receptor B does not promote axonal plasticity or functional recovery after traumatic brain injury. J Neurosci 2010; 30: 13045–13052.
Witte OW . Lesion-induced plasticity as a potential mechanism for recovery and rehabilitative training. Curr Opin Neurol 1998; 11: 655–662.
Redecker C, Luhmann HJ, Hagemann G, Fritschy JM, Witte OW . Differential downregulation of GABAA receptor subunits in widespread brain regions in the freeze-lesion model of focal cortical malformations. J Neurosci 2000; 20: 5045–5053.
Redecker C, Wang W, Fritschy JM, Witte OW . Widespread and long-lasting alterations in GABA(A)-receptor subtypes after focal cortical infarcts in rats: mediation by NMDA-dependent processes. J Cereb Blood Flow Metab 2002; 22: 1463–1475.
Schiene K, Bruehl C, Zilles K, Qu M, Hagemann G, Kraemer M et al. Neuronal hyperexcitability and reduction of GABAA-receptor expression in the surround of cerebral photothrombosis. J Cereb Blood Flow Metab 1996; 16: 906–914.
Whiting PJ . GABA-A receptor subtypes in the brain: a paradigm for CNS drug discovery? Drug Discov Today 2003; 8: 445–450.
Farrant M, Nusser Z . Variations on an inhibitory theme: phasic and tonic activation of GABA(A) receptors. Nat Rev Neurosci 2005; 6: 215–229.
Ono T, Sekino-Suzuki N, Kikkawa Y, Yonekawa H, Kawashima S . Alivin 1, a novel neuronal activity-dependent gene, inhibits apoptosis and promotes survival of cerebellar granule neurons. J Neurosci 2003; 23: 5887–5896.
Bareyre FM, Kerschensteiner M, Raineteau O, Mettenleiter TC, Weinmann O, Schwab ME . The injured spinal cord spontaneously forms a new intraspinal circuit in adult rats. Nat Neurosci 2004; 7: 269–277.
Biernaskie J, Chernenko G, Corbett D . Efficacy of rehabilitative experience declines with time after focal ischemic brain injury. J Neurosci 2004; 24: 1245–1254.
Brown CE, Li P, Boyd JD, Delaney KR, Murphy TH . Extensive turnover of dendritic spines and vascular remodeling in cortical tissues recovering from stroke. J Neurosci 2007; 27: 4101–4109.
Brown CE, Aminoltejari K, Erb H, Winship IR, Murphy TH . In vivo voltage-sensitive dye imaging in adult mice reveals that somatosensory maps lost to stroke are replaced over weeks by new structural and functional circuits with prolonged modes of activation within both the peri-infarct zone and distant sites. J Neurosci 2009; 29: 1719–1734.
Lenzlinger PM, Shimizu S, Marklund N, Thompson HJ, Schwab ME, Saatman KE et al. Delayed inhibition of Nogo-A does not alter injury-induced axonal sprouting but enhances recovery of cognitive function following experimental traumatic brain injury in rats. Neuroscience 2005; 134: 1047–1056.
Katz LC, Shatz CJ . Synaptic activity and the construction of cortical circuits. Science 1996; 274: 1133–1138.
Uesaka N, Hirai S, Maruyama T, Ruthazer ES, Yamamoto N . Activity dependence of cortical axon branch formation: a morphological and electrophysiological study using organotypic slice cultures. J Neurosci 2005; 25: 1–9.
Maier IC, Baumann K, Thallmair M, Weinmann O, Scholl J, Schwab ME . Constraint-induced movement therapy in the adult rat after unilateral corticospinal tract injury. J Neurosci 2008; 28: 9386–9403.
Ruthazer ES, Akerman CJ, Cline HT . Control of axon branch dynamics by correlated activity in vivo. Science 2003; 301: 66–70.
Hua JY, Smear MC, Baier H, Smith SJ . Regulation of axon growth in vivo by activity-based competition. Nature 2005; 434: 1022–1026.
Jacob TC, Moss SJ, Jurd R . GABA(A) receptor trafficking and its role in the dynamic modulation of neuronal inhibition. Nat Rev Neurosci 2008; 9: 331–343.
Katagiri H, Fagiolini M, Hensch TK . Optimization of somatic inhibition at critical period onset in mouse visual cortex. Neuron 2007; 53: 805–812.
Hensch TK . Critical period plasticity in local cortical circuits. Nat Rev Neurosci 2005; 6: 877–888.
Klausberger T, Roberts JD, Somogyi P . Cell type- and input-specific differences in the number and subtypes of synaptic GABA(A) receptors in the hippocampus. J Neurosci 2002; 22: 2513–2521.
Shen H, Sabaliauskas N, Sherpa A, Fenton AA, Stelzer A, Aoki C et al. A critical role for alpha4betadelta GABAA receptors in shaping learning deficits at puberty in mice. Science 2010; 327: 1515–1518.
Brooks-Kayal AR, Shumate MD, Jin H, Rikhter TY, Coulter DA . Selective changes in single cell GABA(A) receptor subunit expression and function in temporal lobe epilepsy. Nat Med 1998; 4: 1166–1172.
Peng Z, Huang CS, Stell BM, Mody I, Houser CR . Altered expression of the delta subunit of the GABAA receptor in a mouse model of temporal lobe epilepsy. J Neurosci 2004; 24: 8629–8639.
Devaud LL, Fritschy JM, Sieghart W, Morrow AL . Bidirectional alterations of GABA(A) receptor subunit peptide levels in rat cortex during chronic ethanol consumption and withdrawal. J Neurochem 1997; 69: 126–130.
Montpied P, Weizman A, Weizman R, Kook KA, Morrow AL, Paul SM . Repeated swim-stress reduces GABAA receptor alpha subunit mRNAs in the mouse hippocampus. Brain Res Mol Brain Res 1993; 18: 267–272.
Hu Y, Lund IV, Gravielle MC, Farb DH, Brooks-Kayal AR, Russek SJ . Surface expression of GABAA receptors is transcriptionally controlled by the interplay of cAMP-response element-binding protein and its binding partner inducible cAMP early repressor. J Biol Chem 2008; 283: 9328–9340.
Lund IV, Hu Y, Raol YH, Benham RS, Faris R, Russek SJ et al. BDNF selectively regulates GABAA receptor transcription by activation of the JAK/STAT pathway. Sci Signal 2008; 1: ra9.
Onyszchuk G, Al-Hafez B, He YY, Bilgen M, Berman NE, Brooks WM . A mouse model of sensorimotor controlled cortical impact: characterization using longitudinal magnetic resonance imaging, behavioral assessments and histology. J Neurosci Methods 2007; 160: 187–196.
Pronichev IV, Lenkov DN . Functional mapping of the motor cortex of the white mouse by a microstimulation method. Neurosci Behav Physiol 1998; 28: 80–85.
Hata K, Fujitani M, Yasuda Y, Doya H, Saito T, Yamagishi S et al. RGMa inhibition promotes axonal growth and recovery after spinal cord injury. J Cell Biol 2006; 173: 47–58.
Reiter HO, Stryker MP . Neural plasticity without postsynaptic action potentials: less-active inputs become dominant when kitten visual cortical cells are pharmacologically inhibited. Proc Natl Acad Sci USA 1988; 85: 3623–3627.
Martin JH, Kably B, Hacking A . Activity-dependent development of cortical axon terminations in the spinal cord and brain stem. Exp Brain Res 1999; 125: 184–199.
Hurley LM, Tracy JA, Bohorquez A . Serotonin 1B receptor modulates frequency response curves and spectral integration in the inferior colliculus by reducing GABAergic inhibition. J Neurophysiol 2008; 100: 1656–1667.
Baskin YK, Dietrich WD, Green EJ . Two effective behavioral tasks for evaluating sensorimotor dysfunction following traumatic brain injury in mice. J Neurosci Methods 2003; 129: 87–93.
Acknowledgements
This work was supported by a Grant-in-Aid for Young Scientists (S) from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Verkhrasky
Supplementary Information accompanies the paper on Cell Death and Disease website
Supplementary information
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Lee, S., Ueno, M. & Yamashita, T. Axonal remodeling for motor recovery after traumatic brain injury requires downregulation of γ-aminobutyric acid signaling. Cell Death Dis 2, e133 (2011). https://doi.org/10.1038/cddis.2011.16
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2011.16
Keywords
This article is cited by
-
Changes in Genome-Wide DNA Methylation Levels in Different Parts of the Rat Brain in Partial Cerebral Ischemia
Neuroscience and Behavioral Physiology (2023)
-
Inhibition of HDAC increases BDNF expression and promotes neuronal rewiring and functional recovery after brain injury
Cell Death & Disease (2020)
-
Effects of ticagrelor in a mouse model of ischemic stroke
Scientific Reports (2017)
-
Prolyl hydroxylase regulates axonal rewiring and motor recovery after traumatic brain injury
Cell Death & Disease (2015)
-
Weakened rate-dependent depression of Hoffmann’s reflex and increased motoneuron hyperactivity after motor cortical infarction in mice
Cell Death & Disease (2014)