Abstract
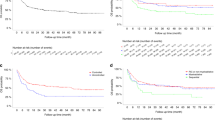
We report a retrospective analysis of 246 myelodysplastic syndrome (MDS) patients in the EBMT (The European Society for Blood and Marrow Transplantation) database who were transplanted for International Prognostic Scoring System (IPSS) low or intermediate-1 disease. The majority of these patients (76%) were reclassified as intermediate or higher risk according to R-IPSS. The 3-year overall survival (OS) and PFS were 58% and 54%, respectively. In a multivariate analysis, adverse risk factors for PFS were marrow blast percentage (hazard ratio (HR): 1.77, P=0.037), donor/recipient CMV serostatus (donor−/recipient+: HR: 2.02, P=0.011) and source of stem cells (marrow and non-CR: HR: 5.72, P<0.0001, marrow and CR: HR: 3.17, P=0.027). Independent risk factors for OS were disease status at time of transplant and the use of in vivo T-cell depletion (TCD). Patients who did not receive TCD and were transplanted from an unrelated donor had worse OS (HR: 4.08, P<0.0001). In conclusion, ‘lower’ risk MDS patients have better outcome than those with ‘higher risk’ after haematopoietic stem cell transplant (HSCT). Selecting the right source of stem cells, a CMV-positive donor for CMV-positive patients and using in vivo TCD results in the best outcome in these patients. More studies are needed to evaluate the role of HSCT in these patients as compared with conventional treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 1997; 89: 2079–2088.
Cutler CS, Lee SJ, Greenberg P, Deeg HJ, Pérez WS, Anasetti C et al. A decision analysis of allogeneic bone marrow transplantation for the myelodysplastic syndromes: delayed transplantation for low-risk myelodysplasia is associated with improved outcome. Blood 2004; 104: 579–585.
Koreth J, Pidala J, Perez WS, Deeg HJ, Garcia-Manero G, Malcovati L et al. Role of reduced-intensity conditioning allogeneic hematopoietic stem-cell transplantation in older patients with de novo myelodysplastic syndromes: an international collaborative decision analysis. J Clin Oncol 2013; 31: 2662–2670.
Platzbecker U, Schetelig J, Finke J, Trenschel R, Scott BL, Kobbe G et al. Allogeneic hematopoietic cell transplantation in patients age 60-70 years with de novo high-risk myelodysplastic syndrome or secondary acute myelogenous leukemia: comparison with patients lacking donors who received azacitidine. Biol Blood Marrow Transplant 2012; 18: 1415–1421.
Robin M, Porcher R, Ades L, Raffoux E, Michallet M, François S et al. HLA-matched allogeneic stem cell transplantation improves outcome of higher risk myelodysplastic syndrome A prospective study on behalf of SFGM-TC and GFM. Leukemia 2015; 29: 1496–1501.
Della Porta MG, Alessandrino EP . Pretransplantation therapy with hypomethylating agents in patients with myelodysplastic syndromes receiving reduced-intensity conditioning regimens. Biol Blood Marrow Transplant 2014; 20: 1260–1261.
Koenecke C, Gohring G, de Wreede LC, van Biezen A, Scheid C, Volin L et al. Impact of the revised International Prognostic Scoring System cytogenetics and monosomal karyotype on outcome after allogeneic stem cell transplantation for myelodysplastic syndromes and secondary acute myeloid leukemia evolving from myelodysplastic syndromes: a retrospective multicenter study of the European Society of Blood and Marrow Transplantation. Haematologica 2014; 100: 400–408.
Martino R, Iacobelli S, Brand R, Jansen T, van Biezen A, Finke J et al. Retrospective comparison of reduced-intensity conditioning and conventional high-dose conditioning for allogeneic hematopoietic stem cell transplantation using HLA-identical sibling donors in myelodysplastic syndromes. Blood 2006; 108: 836–846.
Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med 2011; 364: 2496–2506.
Papaemmanuil E, Gerstung M, Malcovati L, Tauro S, Gundem G, Van Loo P et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood 2013; 122: 3616–3627; quiz 3699.
Bejar R, Stevenson KE, Caughey BA, Abdel-Wahab O, Steensma DP, Galili N et al. Validation of a prognostic model and the impact of mutations in patients with lower-risk myelodysplastic syndromes. J Clin Oncol 2012; 30: 3376–3382.
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia 2014; 28: 241–247.
Malcovati L, Hellstrom-Lindberg E, Bowen D, Adès L, Cermak J, Del Cañizo C et al. Diagnosis and treatment of primary myelodysplastic syndromes in adults: recommendations from the European LeukemiaNet. Blood 2013; 122: 2943–2964.
Schemper M, Smith TL . A note on quantifying follow-up in studies of failure time. Control Clin Trials 1996; 17: 343–346.
Prentice R, Kalbfleisch J, Peterson A, Flournoy N, Farewell V, Breslow N . The analysis of failure times in the presence of competing risks. Biometrics 1978; 34: 541.
Grambsch P, Therneau T . Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994; 81: 515–526.
Gönen M, Heller G . Concordance probability and discriminatory power in proportional hazards regression. Biometrika 2005; 92: 965–970.
Rubin DB, Schenker N . Multiple imputation in health-care databases: an overview and some applications. Stat Med 1991; 10: 585–598.
White IR, Royston P, Wood AM . Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011; 30: 377–399.
Wood AM, White IR, Royston P . How should variable selection be performed with multiply imputed data? Stat Med 2008; 27: 3227–3246.
Harrell FE Jr, Lee KL, Mark DB . Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996; 15: 361–387.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood 2012; 120: 2454–2465.
de Witte T, Brand R, van Biezen A, Mufti G, Ruutu T, Finke J et al. Allogeneic stem cell transplantation for patients with refractory anaemia with matched related and unrelated donors: delay of the transplant is associated with inferior survival. Br J Haematol 2009; 146: 627–636.
Guardiola P, Runde V, Bacigalupo A, Ruutu T, Locatelli F, Boogaerts MA et al. Retrospective comparison of bone marrow and granulocyte colony-stimulating factor-mobilized peripheral blood progenitor cells for allogeneic stem cell transplantation using HLA identical sibling donors in myelodysplastic syndromes. Blood 2002; 99: 4370–4378.
del Canizo MC, Martinez C, Conde E, Vallejo C, Brunet S, Sanz G et al. Peripheral blood is safer than bone marrow as a source of hematopoietic progenitors in patients with myelodysplastic syndromes who receive an allogeneic transplantation. Results from the Spanish registry. Biol Blood Marrow Transplant 2003; 32: 987–992.
Ljungman P, Brand R, Hoek J, de la Camara R, Cordonnier C, Einsele H et al. Donor cytomegalovirus status influences the outcome of allogeneic stem cell transplant: a study by the European group for blood and marrow transplantation. Clin Infect Dis 2014; 59: 473–481.
Ljungman P, Brand R, Einsele H, Frassoni F, Niederwieser D, Cordonnier C . Donor CMV serologic status and outcome of CMV-seropositive recipients after unrelated donor stem cell transplantation: an EBMT megafile analysis. Blood 2003; 102: 4255–4260.
Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol 2009; 10: 855–864.
Kröger N, Solano C, Wolschke C, Bandini G, Patriarca F, Pini M et al. Antilymphocyte globulin for prevention of chronic graft-versus-host disease. N Engl J Med 2016; 374: 43–53.
Acknowledgements
MR, RP, WZ-C and NK designed and analysed the study. RP did the statistical analysis. MR wrote the paper. All co-authors have read the paper, had opportunity to comment it and approved the final version. All co-authors provided patients. We thank all co-investigators who participated in this study providing patients from the European registry (see Appendix).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
Supplementary information
Rights and permissions
About this article
Cite this article
Robin, M., Porcher, R., Zinke-Cerwenka, W. et al. Allogeneic haematopoietic stem cell transplant in patients with lower risk myelodysplastic syndrome: a retrospective analysis on behalf of the Chronic Malignancy Working Party of the EBMT. Bone Marrow Transplant 52, 209–215 (2017). https://doi.org/10.1038/bmt.2016.266
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.266
This article is cited by
-
Allogeneic transplantation of bone marrow versus peripheral blood stem cells from HLA-identical relatives in patients with myelodysplastic syndromes and oligoblastic acute myeloid leukemia: a propensity score analysis of a nationwide database
Annals of Hematology (2023)
-
Allogeneic hematopoietic cell transplantation for myelodysplastic syndrome unclassifiable – a retrospective study on behalf of the Chronic Malignancies Working Party of the EBMT
Bone Marrow Transplantation (2023)
-
Room for Improvement: A 20-Year Single Center Experience with Allogeneic Stem Cell Transplantation for Myelodysplastic Syndromes
Indian Journal of Hematology and Blood Transfusion (2022)
-
Which lower risk myelodysplastic syndromes should be treated with allogeneic hematopoietic stem cell transplantation?
Leukemia (2020)
-
Clinical impact of the loss of chromosome 7q on outcomes of patients with myelodysplastic syndromes treated with allogeneic hematopoietic stem cell transplantation
Bone Marrow Transplantation (2019)