Abstract
Data are limited regarding the prevalence of menstrual cycles and pregnancies after high-dose chemotherapy (HDC) and auto-stem cell transplantation (SCT). Female patients who underwent HDC auto-SCT for non-Hodgkin and Hodgkin lymphoma (1997–2012) were reviewed. The selection criteria were as follows: (1) alive without disease 12 and 24 months after auto-SCT for menstrual cycles and pregnancy, respectively, (2) age <40 years at auto-SCT, and (3) no primary infertility. One-hundred and seventy-six females underwent single auto-SCT. Eighty-nine were eligible for menstrual cycles and pregnancy analysis. Median age at auto-SCT was 25 years (14–40 years), at pregnancy 27 years (20–37 years), median follow-up 65 months (range 24–190). Regular menstrual-cycles resumed in 56/89 patients (63%). Increasing age (P=0.02) and number of prior chemotherapy cycles (P=0.02) are associated with higher risk of amenorrhea. Forty patients tried to get pregnant, 26 (65%) became pregnant 50 times: 43 (86%) live birth, 7 (14%) miscarriage and 2/50 had birth defects. Twenty-four patients practiced breastfeeding (median duration 4 months (1–24 months)). Enough breast milk production was reported 62.5% vs 100% in those patients who did or did not receive above the diaphragm radiation therapy, respectively, (P=0.066). Our data highlights significantly higher than perceived incidence of menstrual cycle resumption, successful pregnancies and breastfeeding after HDC auto-SCT.
Similar content being viewed by others
Introduction
There is an increasing use of high-dose chemotherapy (HDC) and autologous stem cell transplantation (auto-SCT) for patients with relapsed or refractory non-Hodgkin and Hodgkin lymphoma (HL) and other hematological malignancies. Most pre-transplant conditioning regimens use alkylating agents with or without radiation therapy (XRT), either of which can potentially cause germ cell injury, thus resulting in premature ovarian failure (POF) and infertility.1, 2, 3 Available data are limited to address the incidence and prevalence of pregnancies after HDC auto-SCT.4, 5, 6, 7, 8, 9, 10, 11, 12, 13 Many studies have combined both allogeneic and auto-SCT for various hematological malignancies and even non-malignant conditions.14, 15 Over the last 10–15 years, early HDC auto-SCT has resulted in a significantly reduced number of prior chemotherapy cycles. Data are non-existent in the Middle Eastern/Arab countries where average family size is significantly larger and patients are relatively younger than patients in Western/North American societies. The primary objective of our study is to identify in females with diffuse large B-cell lymphoma and HL who underwent HDC auto-SCT; (1) prevalence of menstrual cycles, (2) incidence and outcome of pregnancy and (3) breastfeeding-related issues.
Materials and methods
Study design
This was a Retrospective cohort study approved by the Institutional Research Advisory Council, with permission to interview patients and collect relevant information regarding reproductive health. Consents for all treatments, procedures and HDC auto-SCT were obtained as per institutional policies. Patients, and where appropriate, families, were informed of POF and infertility risk, both before the salvage chemotherapy as well as HDC auto-SCT.
Questionnaire and interview methods
Disease and treatment related information was gathered using HDC auto-SCT comprehensive data. Investigators developed a questionnaire consisting of 50 questions to address menstruation, pregnancy, breastfeeding information and social issues, such as the number of children in a family, level of support during breastfeeding, safety of breastfeeding and patients’ perspective. A single interviewer (IY) administered this questionnaire. Information related to menstruation and pregnancies (a) before the diagnosis of lymphoma, (b) after finishing primary chemotherapy, (c) after finishing HDC auto-SCT and (d) at the time of interview was collected. Menstruation was recorded as regular, irregular, no menstruation and whether with or without the assistance of hormones replacement and/or oral contraception pills. All pregnancies and miscarriage/abortions for these patients at any time (before and after the diagnosis of lymphoma) were recorded.
Statistical analysis
Age at HDC auto-SCT and selected factors (pathology, type and number of chemotherapy cycles, number of salvage chemotherapy used, use of radiation therapy and refractory vs relapsed disease) and their impact on menstruation and pregnancy was calculated. Categorical variables were summarized using frequencies and percentages whereas continuous variables were summarized using medians and rages. Chi-square test was used to compare categorical variables and Mann–Whitney test for comparing continuous variables. Odds ratio for selected factors on menstruation and pregnancy were calculated using logistic regression. Factors with P-value<0.2 were selected for multivariate analysis using logistic regression.
Patient population and definitions
All female patients age 14–40 years (at HDC auto-SCT) who underwent HDC auto-SCT for diffuse large B-cell lymphoma and HL from 1997 to December 2012 in the Section of Adult Medical Oncology with the following selection criteria were included; (1) alive without evidence of disease 12 and 24 months after HDC auto-SCT for menstrual cycles and pregnancy respectively, (2) age <40 years at the time of HDC auto-SCT, (3) no known cause of primary infertility and (4) no radiation therapy to pelvic area, and (5) alive and willing to participate in an interview. Regular menstrual cycle was defined as menstrual cycles at regular intervals (from 20 to 35 days) for that patient for a period of six consecutive months. Cycles were considered irregular if they failed to follow a regular pattern. Follicle stimulating hormone and luteinizing hormone measurement, or ovarian ultrasounds, were not required for any definition nor ordered for this study. Pregnancy evaluation was planned after 24 months post-HDC auto-SCT as patients were instructed not to get pregnant for 24 months post-HDC auto-SCT. Methods for pregnancy prevention after HDC auto-SCT were left up to the patient’s discretion and their family physicians/gynecologists. Menstrual cycles were checked at 12 months due to early menstrual cycle recovery in our group.
Results
Eligible patients
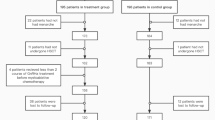
From March 1997 to December 2012, 176 females underwent HDC auto-SCT. Eighty-seven were excluded: 62 were dead at the time of this analysis (32/62 persistent/progressive disease, 8/62 treatment-related mortality, 16/62 died due to relapsed disease within 24 months and 6/62 died of an other reason). Eighteen were >40 years, three had active disease and four with no information. Finally, 89 patients (>24 months follow-up) were evaluable for both menstrual cycles and pregnancy (Figure 1). Patients’ characteristics are shown in Table 1.
Patients’ characteristics and treatment
Median age of patients at HDC auto-SCT was 25 years (14–40 years). Median follow-up from HDC auto-SCT was 65 months (24–190 months), HL in 71 (80%) and diffuse large B-cell lymphoma in 18 (20%). Primary chemotherapy was adriamycin, bleomycin, vinblastin and dacarbazine (ABVD) in 60 (68%) and cyclophosphamide, adriamycin, vincristine and prednisone (CHOP) in 16 (18%; Table 1). Median number of chemotherapy cycles before HDC was 10 for these 89 patients; same as for those who actually became pregnant (9.5 cycles). Fifty-seven (64%) patients had prior XRT. Forty-two (74%) patients had mediastinal area XRT: mediastinum alone in 26%, mediastinum+neck in 33%, mediastinum+neck+axilla in 11% and mediastinal+below the diaphragm in 9%. Etoposide, solumedrol, cisplatinum and Ara-C (ESHAP) was primarily used as salvage chemotherapy in 81 patients (91%). Carmustine, etoposide, cytarabine and melphalan was used as HDC (Table 1).
Use of hormones and contraceptive pills
Fifteen females used some form of hormones for 1–8 years. Five used combination monophasic contraceptive pills, seven used some hormones to regularize their periods (only two provided the details) and three used both hormones and contraceptive pills at different time frames (only one provided the name of contraceptive pills she used). Twelve patients had regular periods and three had varying duration of periods while using these pills due to irregular/interrupted use of contraceptive pills and were grouped in the no menstruation group. Of these 15 patients, seven tried to become pregnant and four became pregnant seven times. Eight of these 15 patients did not try pregnancy post auto-SCT (four not sexually active, three already with children and one with no contact).
Menstrual cycle recovery
Before the start of primary (first line) chemotherapy, regular menstrual cycles were reported in 88%, irregular in 9% and no menstrual cycles in 3% (age at diagnosis 13, 14 and 27 years). In all, 56/89 (63%) patients resumed regular menstrual cycles post-HDC auto-SCT (12/56 patients with hormone assistance). Median time to resume regular menstruation was 8.5 months (1–48 months). However, this was as early as 1 month for 10 patients. Of these 56 patients, 76% resumed regular periods between 1 and 12 months. The oldest patient who resumed menstruation was 39 years at HDC auto-SCT. Only 4/17 patients above the age of 30 had resumption of menstruation (2 with hormonal assistance). In all, 33/89 (37%) patients had no (23 patients, 26%) or irregular (10 patients, 11%) menstruation; only 14/33 patients had followed up <48 months. In all, 3/33 females also tried hormone assistance but failed to resume menstruation. Table 2 provides various factors and their impact on menstruation.
Age as a continuous variable (P=0.007, Fisher’s exact test) and prior chemotherapy cycles (P=0.013, Fisher’s exact test) clearly showed an association of higher age at HDC auto-SCT and increasing number of chemotherapy cycles with higher risk of amenorrhea. In multivariate analysis, only age (P=0.02, odds ration 1.1, confidence interval 1.01–1.2, logistic regression) and number of prior chemotherapy cycles (P=0.02, odds ration 1.3, confidence interval 1.03–1.6, logistic regression) were significant (Tables 2 and 3). In other words, for these patients, with each increasing year in age, there was an 11% increased chance of amenorrhea, and with each cycle of chemotherapy, there was a 13% increased chance of amenorrhea.
Pregnancies and their outcome
Before HDC auto-SCT, 49 females were married and 29 of them already had 75 pregnancies with 9 (12%) miscarriages. In all, 22/25 (one patient not accessible) patients who actually delivered post-HDC auto-SCT anticipated that they might become pregnant after HDC despite our discussion of high risks of POF and infertility. Regarding ‘number of children considered as a complete family’, patients’ response was: one and two children by 17 (20%), three and four children by 46 (55%) and five or more children by 21 (25%) patients.
Fifty-one of these 89 patients were married and 48 were sexually active at the time of interview (3 are now divorced/not active sexually). Eight females did not attempt to become pregnant; Seven of them already had 1–6 children and one (age 24 years at HDC) had no menstruation after HDC auto-SCT. Forty females tried to become pregnant. Out of 26 patients who became pregnant, 17/26 had regular spontaneous menstruation, 3/26 had regular hormone-assisted menstruation, 3/26 had irregular menstruation and 3/26 became pregnant while they were not having menstruation. Of those 14 patients who tried to become pregnant and failed, 9 tried pregnancy while not having any periods post-HDC auto-SCT. Three patients had regular spontaneous menstruation and two consulted their local gynecologists to regularize their menstruation with hormones, then tried to become pregnant with no success.
Twenty-six patients (65%) became pregnant 50 times (range 1–6 times). Median age at first pregnancy post-HDC auto-SCT was 27 years (range 20–37 years) (Table 4). Of these 50 pregnancies, 43 (86%) were live births and 7 (14%) miscarriages, including 1 still birth (at 28 weeks). In all, 2/26 pregnant patients used hormone assisted ovulation, 1/26 had hormone assistance then in vitro fertilization. The remaining 23 patients had unassisted normal conception. The first pregnancy was observed from 5 to 114 months after HDC auto-SCT.
Birth defects were observed in two live births as reported by the patients (congenital diaphragmatic hernia in one live birth, died 3 days after delivery and one had situs invertus, who is still alive). Eight females had their first ever conception (gravida 1) after the HDC auto-SCT. In all, 14/40 females had no pregnancy despite their efforts and only one of them had a workup for infertility while no male partner had any workup for infertility. Multiple factors were tested as shown in Table 2 that failed to show any impact on pregnancy, most likely due to the small number of patients.
Child development
Details of birth weight and developmental milestones were not available for live birth/alive children as most of them were neither born nor followed in our institution. At the time of this report, these children were 2 months to 11.5 years old. Their mothers had not reported any developmental issues or concerns related to social interactions or school performance for these children.
Breastfeeding
Twenty-four patients breastfed their children; information was not available for two patients, one with intrauterine fetal demise and one who left the country/no contact. In all, 6/24 patients used only breast milk as their sole source for milk, whereas 18/24 patients used breast milk+formula milk. Breast milk production was considered enough by 18/24 (75%) patients; still 12/18 of them used supplemental formula. In all, 6/24 (23%) patients used supplemental formula due to suboptimal milk production; one had no milk production, one switched to formula after a few days due to suboptimal production, two patients breastfed for 3 months, and for one patient, duration is not available while one was still breastfeeding and using supplemental formula from the beginning. All these six women with suboptimal breast milk production had received radiation therapy (five to mediastinum and one to axilla).
All females who gave live births breastfed their children (except one with no milk production). Only one patient in this group considered breastfeeding post-HDC auto-SCT as unsafe but interestingly she also breastfed her child for 3 months. Breastfeeding post-HDC auto-SCT was considered safe by 96% of those who gave birth as compared with 69% by those who never gave birth (P=0.008, Fisher’s exact test, two sided).
Median duration of breastfeeding was 4 months (range 1–24 months); 9 (41%) breastfed for <6 months, 4 (18%) for 7–12 months and 2 (9%) for 12–24 months (unknown for 7 women and 1 still feeding). Only two women claimed that their husband or family members stopped them from breastfeeding, whereas 19/24 were encouraged to breastfeed. In all, 59/89 (66%) patients considered breast milk as a safe option after HDC auto-SCT, whereas 17/89 (19%) did not (no answer from 10 patients). All respondents answered ‘Yes’ to the question ‘would you consider breastfeeding your child if you had no lymphoma?’. Sixteen patients who breastfed also had XRT. One patient had mesenteric area XRT 4500 cGy. All other 15/16 had mediastinal area XRT: 2/15 had modified mantle XRT (3700–4000 cGy), 4/15 had mediastinal+neck XRT (3060–3600 cGy), 8/15 had only mediastinal XRT (3000–3960 cGy) and 1/15 medistinum+thoracic spine (3060 cGy). Dose to mediastinum for six patients was 3060 cGy, five had 3600–3700 cGy and four had 3800-4000 cGy mediastinal XRT. In all, 10/16 (62.5%) patients who had radiation claimed to had enough breast milk production as compared with 8/8 (100%) patients who never received above the diaphragm XRT (P=0.066, Fisher’s exact test, two sided).
Discussion
This is the first study from the Middle East/Arab countries exploring menstrual cycles, fertility, outcome of pregnancy and breastfeeding in patients who underwent HDC auto-SCT. As compared to Western/North American reports, our population is younger, has larger family size with difference in sexual practices that is, having children without marriage is socially/legally and religiously unacceptable. Previous reports have not addressed the intentional ‘no pregnancy’ issue in potentially fertile HDC auto-SCT patients. Our patients have uniform treatment and no TBI.16 We have only included patients <40 years old at HDC auto-SCT. We have observed 63% regular menstrual cycles after HDC auto-SCT, 29% pregnancy in the entire potential group of 89 patents and 65% pregnancy in those patients who actually tried (40 patients) to become pregnant. This is the highest incidence of pregnancies ever reported after HDC auto-SCT. Furthermore, 86% normal pregnancies and 14% miscarriage+stillbirths is almost the same in this group of patients as observed before auto-SCT (12%). We identified increasing age (P=0.02) and higher number of prior chemotherapy cycles (P=0.02) as risk factors for amenorrhea on both univariate and multivariate analysis. Same factors failed to show any impact on pregnancy, likely due to small number of patients. Our major limitations include the unavailability of follicular stimulating hormone and luteinizing hormone levels and ovarian ultrasound in those patients who were having amenorrhea, irregular periods or having periods but failed to become pregnant despite their efforts. Also, details of hormonal use are not available for 8/15 patients. Another limitation is the absence of infertility evaluation of male partners. Our observation of early resumption of menstrual cycle and pregnancies suggests that future studies should consider early evaluation for menstrual cycles. Also, presence or absence of menstrual cycle should not be considered a definitive sign for fertility or infertility without a proper diagnostic workup. Appropriate timing to consider someone having POF post-HDC auto-SCT requires more data and input from other studies. Question about number of children considered as a complete family was asked as part of the interview, after the patients already had HDC auto-SCT. There is a chance that this answer might vary before and after HDC auto-SCT and ideally a base line response prior to HDC auto-SCT should have been obtained. Also, patients’ perceptions of breastfeeding as unsafe who never delivered is an intriguing observation and may change after the birth.
Pregnancy and menstruation related data are limited in the HDC auto-SCT setting. There are limited case reports/series addressing pregnancies after HDC auto-SCT.4, 5, 6, 7, 8, 9, 10, 11, 12 Carter et al.8 reported 122 female patients who underwent HDC auto-SCT; only four (3%) of them became pregnant and gave live birth nine times (three with HL and one with non-Hodgkin lymphoma). Two of these patients also had TBI based conditioning. Loren et al.11 reported Center for International Blood and Marrow Transplant Research (CIBMTR) observational data on patients transplanted before 2007. They identified 20 females (18 with lymphoma) who underwent HDC auto-SCT (non-TBI based conditioning) and became pregnant. Further details are missing.
Salooja et al.13 from University College Hospital, London, UK reported 24 premenopausal females. Twelve had a double transplant and only one resumed menstruation. Ten had single transplant and six of them (age range 21–32 years) resumed menstruation. Five of these six menstruating women became pregnant between 4 and 40 months following HDC auto-SCT. Salooja et al.4 also reported The European Group for Blood and Marrow Transplantation (EBMT) data on transplants performed before 1994. Total HDC auto-SCT were 17 950 (separate numbers for female are not provided). She reported 39 females with 44 pregnancies.
We have evaluated 89 patients for menstrual cycles, pregnancies and related issues. This is one of the highest single institution numbers reported to-date in this setting. We have not used gonadotropin-releasing hormone agonist before HDC. Blumenfeld et al.17 reported administration of gonadotropin-releasing hormone agonist before HDC auto-SCT with decrease in the gonadotoxicity and POF from 82% to 33% in lymphoma but not in leukemia patients; indicating disease specific primary treatment effect on POF. Donnez et al.18 reported 60 orthotopic reimplantations of cryopreserved ovarian tissue with promising results. Utilization of these and other fertility preservation techniques may be offered to a carefully selected group of patients who are likely to suffer from POF and have good chances of preservation of fertility with these techniques.
Conclusion
A properly defined selection criterion for pregnancies and fertility studies post transplant is essential. Our data highlights a significantly higher than perceived incidence of menstrual periods and successful pregnancies with normal deliveries after auto-SCT in patients younger than 40 years. Furthermore, advanced age and increasing numbers of prior chemotherapy cycles are associated with higher risk of amenorrhea. Breastfeeding was common in this population. Finally, proper counseling and discussion regarding fertility is essential before HDC auto-SCT.
References
Reinmuth S, Hohmann C, Rendtorff R, Balcerek M, Holzhausen S, Muller et al. Impact of chemotherapy and radiotherapy in childhood on fertility in adulthood: the FeCt-survey of childhood cancer survivors in Germany. J Cancer Res Clin Oncol 2013; 139: 2071–2078.
Green DM . Fertility and pregnancy outcome after treatment for cancer in childhood or adolescence. The Oncologist 1997; 2: 171–179.
Liu J, Malhotra R, Voltarelli J, Stracieri AB, Oliveira L, Simoes BP et al. Ovarian recovery after stem cell transplantation. Bone Marrow Transplant 2008; 41: 275–278.
Salooja N, Szydlo RM, Socie G, Rio B, Chatterjee R, Ljungman P et al. Pregnancy outcomes after peripheral blood or bone marrow transplantation: a retrospective survey. Lancet 2001; 358: 271–276.
Sanders JE, Hawley J, Levy W, Gooley T, Buckner CD, Deeg HJ et al. Pregnancies following high-dose cyclophosphamide with or without high-dose busulfan or total-body irradiation and bone marrow transplantation. Blood 1996; 87: 3045–3052.
Brice P, Pautier P, Marolleau JP, Castaigne S, Gisselbrecht C . Pregnancy after autologous bone marrow transplantation for malignant lymphomas. Nouv Rev Fr Hematol 1994; 36: 387–388.
Brice P, Haioun C, Andre M, Gisselbrecht C . Groupe d'Etude des Lymphomes de l'Adulte. Pregnancies after high-dose chemotherapy and autologous stem cell transplantation in aggressive lymphomas. Blood 2002; 100: 736.
Carter A, Robison LL, Francisco L, Smith D, Grant M, Baker KS et al. Prevalence of conception and pregnancy outcomes after hematopoietic cell transplantation: report from the Bone Marrow Transplant Survivor Study. Bone Marrow Transplant 2006; 37: 1023–1029.
Dupont C, Bally C, Eustache F, Sermondade N, Benzacken B, Fenaux P et al. Spontaneous conception after autologous hematopoietic stem cell transplantation: a case report. Asian J Androl 2013; 15: 155–156.
Hershlag A, Schuster MW . Return of fertility after autologous stem cell transplantation. Fertil Steril 2002; 77: 419–421.
Loren AW, Chow E, Jacobsohn DA, Gilleece M, Halter J, Joshi S et al. Pregnancy after hematopoietic cell transplantation: a report from the late effects working committee of the Center for International Blood and Marrow Transplant Research (CIBMTR). Biol Blood Marrow Transplant 2011; 17: 157–166.
Nakagawa K, Kanda Y, Yamashita H, Nakagawa S, Sasano N, Ohtomo K et al. Ovarian shielding allows ovarian recovery and normal birth in female hematopoietic SCT recipients undergoing TBI. Bone Marrow Transplant 2008; 42: 697–699.
Salooja N, Chatterjee R, McMillan AK, Kelsey SM, Newland AC, Milligan DW et al. Successful pregnancies in women following single autotransplant for acute myeloid leukemia with a chemotherapy ablation protocol. Bone Marrow Transplant 1994; 13: 431–435.
Grigg AP, McLachlan R, Zaja J, Szer J . Reproductive status in long-term bone marrow transplant survivors receiving busulfan-cyclophosphamide (120 mg/kg). Bone Marrow Transplant 2000; 26: 1089–1095.
Meng J, Wang J, Liang W, Qin S, Wu C . Long-term remission after successful pregnancy in autologous peripheral blood stem cell transplanted system lupus erythematosus patients. Rheumatol Int 2011; 31: 691–694.
Akhtar S, Al-Sugair AS, Abouzied M, Alkadhi Y, Dingle M, Abdelsalam M et al. Pre-transplant FDG-PET-based survival model in relapsed and refractory Hodgkin's lymphoma: outcome after high-dose chemotherapy and auto-SCT. Bone Marrow Transplant 2013; 48: 1530–1536.
Blumenfeld Z, Patel B, Leiba R, Zuckerman T . Gonadotropin-releasing hormone agonist may minimize premature ovarian failure in young women undergoing autologous stem cell transplantation. Fertil Steril 2012; 98: 1266–1270.
Donnez J, Squifflet J, Jadoul P, Demylle D, Cheron AC, Van Langendonckt et al. Pregnancy and live birth after autotransplantation of frozen-thawed ovarian tissue in a patient with metastatic disease undergoing chemotherapy and hematopoietic stem cell transplantation. Fertil Steril 2011; 95: 1787.e1-4.
Acknowledgements
We appreciate Dr Abida Rehman for data management and Haris Syed for proof reading.
Author contributions
SA was the principal investigator, analyzed the data and took primary responsibility for the paper. IY conducted interviews with the patients and helped in manuscript writing. HS helped in manuscript writing who also holds an academic position at Oncology Department, Faculty of Medicine at Cairo University, Cairo, Egypt. TAME performed statistical analysis and helped in manuscript writing. SMR helped in manuscript writing. IM was the co-principal investigator and helped in data interpretation and in manuscript writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Akhtar, S., Youssef, I., Soudy, H. et al. Prevalence of menstrual cycles and outcome of 50 pregnancies after high-dose chemotherapy and auto-SCT in non-Hodgkin and Hodgkin lymphoma patients younger than 40 years. Bone Marrow Transplant 50, 1551–1556 (2015). https://doi.org/10.1038/bmt.2015.178
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.178