Abstract
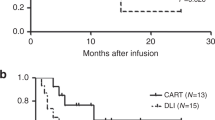
PBSCs are increasingly being chosen as the mode of donation among unrelated donors. Pediatric patients, in particular, may receive very high CD34+ and CD3+ doses during unrelated PBSCT. In this work, we analyzed survival and GVHD outcomes in a cohort of 81 children who received unrelated PBSCT with uniform antithymocyte globulin (ATG)-based in vivo T-cell depletion for treatment of hematologic malignancy, with emphasis on the impact of cell dose on transplant outcomes. EFS was 61.5±5.6%, with higher CD34+ dose (>10.0 × 106/kg) and lower patient risk status predicting improved survival in multivariate study. Cumulative incidence of relapse was 30.2±5.2%; a low CD34+ dose was the only significant factor for relapse. Neither CD34+ nor CD3+ dose was a significant determinant of acute or chronic GVHD. Importance of CD34+ dose was reaffirmed in a subcohort of younger patients who received greater median cell doses than the overall cohort. In summary, for children who received unrelated PBSCT with ATG-based T-cell depletion for treatment of hematologic malignancy, the CD34+ dose was the most important factor for relapse and EFS, and neither the CD34+ nor the CD3+ dose influenced incidence of acute or chronic GVHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Eapen M, Logan BR, Confer DL, Haagenson M, Wagner JE, Weisdorf DJ et al. Peripheral blood grafts from unrelated donors are associated with increased acute and chronic graft-versus-host disease without improved survival. Biol Blood Marrow Transplant 2007; 13: 1461–1468.
Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med 2012; 18: 1487–1496.
Meisel R, Laws HJ, Balzer S, Bernbeck B, Kramm C, Schönberger S et al. Comparable long-term survival after bone marrow versus peripheral blood progenitor cell transplantation from matched unrelated donors in children with hematologic malignancies. Biol Blood Marrow Transplant 2007; 13: 1338–1345.
Remberger M, Ringdén O . Similar outcome after unrelated allogeneic peripheral blood stem cell transplantation compared with bone marrow in children and adolescents. Transplantation 2007; 84: 551–554.
Lin YF, Lairson DR, Chan W, Du XL, Leung KS, Kennedy-Nasser AA et al. Children with acute leukemia: a comparison of outcomes from allogeneic blood stem cell and bone marrow transplantation. Pediatr Blood Cancer 2011; 56: 143–151.
Meisel R, Klingebiel T, Dilloo D . Peripheral blood stem cells versus bone marrow in pediatric unrelated donor stem cell transplantation. Blood 2013; 121: 863–865.
Pulsipher MA, Chitphakdithai P, Logan BR, Leitman SF, Anderlini P, Klein JP et al. Donor, recipient, and transplant characteristics as risk factors after unrelated donor PBSC transplantation: beneficial effects of higher CD34+ cell dose. Blood 2009; 114: 2606–2616.
Kałwak K, Porwolik J, Mielcarek M, Gorczyńska E, Owoc-Lempach J, Ussowicz M et al. Higher CD34(+) and CD3(+) cell doses in the graft promote long-term survival, and have no impact on the incidence of severe acute or chronic graft-versus-host disease after in vivo T cell-depleted unrelated donor hematopoietic stem cell transplantation in children. Biol Blood Marrow Transplant 2010; 16: 1388–1401.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Lee SJ, Vogelsang G, Flowers MED . Chronic graft-versus-host disease. Biol Blood Marrow Transplant 2003; 9: 215–233.
Gaziev J, Isgrò A, Marziali M, Daniele N, Gallucci C, Sodani P et al. Higher CD3(+) and CD34(+) cell doses in the graft increase the incidence of acute GVHD in children receiving BMT for thalassemia. Bone Marrow Transplant 2012; 47: 107–114.
Tsirigotis P, Shapira MY, Or R, Bitan M, Samuel S, Gesundheit B et al. The number of infused CD34+ cells does not influence the incidence of GVHD or the outcome of allogeneic PBSC transplantation, using reduced-intensity conditioning and antithymocyte globulin. Bone Marrow Transplant 2010; 45: 1189–1196.
Bahçeci E, Read EJ, Leitman S, Childs R, Dunbar C, Young NS et al. CD34+ cell dose predicts relapse and survival after T-cell-depleted HLA-identical haematopoietic stem cell transplantation (HSCT) for haematological malignancies. Br J Haematol 2000; 108: 408–414.
Sohn SK, Kim JG, Kim DH, Lee NY, Suh JS, Lee KB . Impact of transplanted CD34+ cell dose in allogeneic unmanipulated peripheral blood stem cell transplantation. Bone Marrow Transplant 2003; 31: 967–972.
Gonzalez-Vicent M, Diaz MA . Higher doses of CD34+ PBPC are associated with a rapid acquisition of full donor chimerism and lower risk of relapse after allogeneic transplantation in pediatric patients with hematological malignancies. J Pediatr Hematol Oncol 2011; 33: 185–189.
Nakamura R, Auayporn N, Smith DD, Palmer J, Sun JY, Schriber J et al. Impact of graft cell dose on transplant outcomes following unrelated donor allogeneic peripheral blood stem cell transplantation: higher CD34+ cell doses are associated with decreased relapse rates. Biol Blood Marrow Transplant 2008; 14: 449–457.
Zaucha JM, Gooley T, Bensinger WI, Heimfeld S, Chauncey TR, Zaucha R et al. CD34 cell dose in granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cell grafts affects engraftment kinetics and development of extensive chronic graft-versus-host disease after human leukocyte antigen-identical sibling transplantation. Blood 2001; 98: 3221–3227.
Mohty M, Bilger K, Jourdan E, Kuentz M, Michallet M, Bourhis JH et al. Higher doses of CD34+ peripheral blood stem cells are associated with increased mortality from chronic graft-versus-host disease after allogeneic HLA-identical sibling transplantation. Leukemia 2003; 17: 869–875.
Sedlácek P, Formánková R, Keslová P, Srámková L, Hubácek P, Król L et al. Low mortality of children undergoing hematopoietic stem cell transplantation from 7 to 8/10 human leukocyte antigen allele-matched unrelated donors with the use of antithymocyte globulin. Bone Marrow Transplant 2006; 38: 745–750.
Remberger M, Mattsson J, Hausenberger D, Schaffer M, Svahn BM, Ringdén O . Genomic tissue typing and optimal antithymocyte globuline dose using unrelated donors results in similar survival and relapse as HLA-identical siblings in haematopoietic stem-cell transplantation for leukaemia. Eur J Haematol 2008; 80: 419–428.
Shaw BE, Apperley JF, Russell NH, Craddock C, Liakopoulou E, Potter MN et al. Unrelated donor peripheral blood stem cell transplants incorporating pre-transplant in-vivo alemtuzumab are not associated with any increased risk of significant acute or chronic graft-versus-host disease. Br J Haematol 2011; 153: 244–252.
Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol 2009; 10: 855–864.
Giebel S, Giorgiani G, Martinetti M, Zecca M, Maccario R, Salvaneschi L et al. Low incidence of severe acute graft-versus-host in children given haematopoietic stem cell transplantation from unrelated donors prospectively matched for HLA class I and II alleles with high-resolution molecular typing. Bone Marrow Transplant 2003; 31: 987–993.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
Supplementary information
Rights and permissions
About this article
Cite this article
Lee, J., Kim, Sk., Jang, PS. et al. Impact of CD34+ cell dose in children who receive unrelated PBSCT with in vivo T-cell depletion for hematologic malignancies. Bone Marrow Transplant 50, 68–73 (2015). https://doi.org/10.1038/bmt.2014.202
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2014.202