Abstract
Umbilical cord blood (UCB) as a source of hematopoietic stem cells for transplantation is limited by the low number of cells and delayed engraftment. UCB cells are infused i.v. for transplantation, although only a proportion of the cells reach the BM. We investigated whether UCB could be administered safely using superselective intra-arterial (i.a.) injection. We injected human UCB (5 × 106) into the aorta in rats, into the iliac artery in mice and into the femoral nutrient artery (FNA) in rabbits. We used angiography, immunohistochemistry, intravital microscopy and qPCR to assess safety end points and the distribution of injected cells. All animals showed normal behavior. No evidence of organ infarction was noted. UCB injected into the FNA of rabbits did not change the flow rates, measured by angiography. By qPCR, we found significantly higher fold-change values in the injected BM compared with i.v. injection (P=0.0087). Using intravital microscopy we visualized the mouse capillary bed during i.a. injection without cellular congestion. In summary, we show that i.a. infusion of UCB is safe and reaches an eightfold increase in engraftment in the BM compared with i.v. infusion. These studies lay the foundation for clinical trials.
Similar content being viewed by others
Introduction
In the late 1950 s, early in the era of BMT, attempts were made to administer BM intra-arterially (i.a.) to enhance engraftment.1,2 The results did not encourage further development as robust protocols using the i.v. route were established and as the techniques for i.a. injections were technically difficult.
In the 1960 s, interventional radiology was developed from diagnostic angiography. Since then, interventional radiology has become a widely accepted and commonly used therapeutic instrument for several diseases in different fields of medicine. More recently, interventional radiology has been applied to experimental i.a. stem cell delivery to peripheral arteries, the myocardium and the central nervous system.3, 4, 5 The potential advantages in selective i.a. cell transplantation include minimization of cell loss, reduction of non-specific cell engraftment and more effective engraftment by exposing the targeted tissue to all the transplanted cells.
Umbilical cord blood (UCB) has been increasingly used as a source of hematopoietic stem cells in transplantation.6, 7, 8 One of the major obstacles to i.v. UCB transplantation is the relatively low amount of stem cells in the graft, causing delayed engraftment.9 It is well known that there is a correlation between the total dose of nucleated cells transplanted per kilogram of body weight of the recipient and outcome.3, 4, 5,10 Also, some of the repopulating cells in UCB may have attenuated homing capacities.6, 7, 8,11,12 The homing of hematopoietic stem cells to the BM and the spleen has been estimated to be 18–20% and 8–10%, respectively.13,14 The cells that do not reach their hematopoietic niches are to a large extent sequestered in organs with large capillary beds, such as the liver and lungs, where they are killed by radio-resistant host cells.13,15, 16, 17, 18
The aim of this study was to evaluate the safety of i.a. delivery of umbilical cord cells in different animal models and to test the feasibility and safety of superselective i.a. injections to the femoral BM using a rabbit model with full integration of clinical catheters and angiography systems. We show that i.a. infusions of UCB directly to the femoral BM are technically feasible. We used this method to compare i.a. UCB infusion directly to the femoral BM with i.v. infusion. qPCR and immunohistochemistry (IHC) were used to detect differences in the distribution of UCB cells transplanted by the i.a. or i.v. route. By observations of health status, IHC and intravital microscopy we ruled out acute and chronic complications in different animal model systems. This technique is safe, and could promote early and effective engraftment of hematopoietic progenitor cells.
Materials and methods
Cell preparation
UCB was obtained from full-term babies delivered at Karolinska University Hospital in Huddinge, after obtaining informed consent from their parents. Ethical approval was obtained from the institutional ethics review board. Blood samples were collected in heparinized tubes and mononuclear cells were isolated by density-gradient centrifugation over LymphoPrep (AXIS-SHIELD PoC AS, Oslo, Norway). Cells were washed in RPMI medium (Thermo Fisher Scientific, Waltham, MA, USA) with 5% AB serum, frozen slowly in medium supplemented with 10% DMSO (WAK-Chemie Medical GmbH, Steinbach, Germany), and stored in liquid nitrogen. On the day of transplantation, cells were thawed and kept in RPMI with 5% AB serum at 37 °C before infusion.
Transplantation in small animals
All animal studies were conducted according to the Karolinska Institute guidelines for experiments on rodents and rabbits. This study was approved by the regional ethics committee for animal research.
Four adult male Sprague-Dawley rats (350–400 g) were permitted food and water ad libitum until surgery. Anesthesia was induced using 4% isoflurane mixed with 94% O2 and subsequently maintained at 2% isoflurane. Animals were kept normothermic on a heating pad. An incision (5 mm) was made on the ventral side of the tail. The tail artery was cut and a 0.0157-inch micro-catheter (Sonic; Balt Extrusion, Montmorency, France) carrying a 0.007-inch microwire (Hybrid; Balt Extrusion) was advanced to a tip position in the thoracic aorta. Next, 5 million UCB cells in 300 μl saline with 10% AB serum were infused for 1 min. In four animals, we injected 5 million UCB cells in 300 μl saline with 10% AB serum i.v. into the tail vein. Animals were returned to their cages with food and water ad libitum. Animals were weighed before surgery and at 24 h. Assessment of motility, spontaneous activity and gait was performed at 2, 4 and 24 h for gross evaluation of animal condition. All animals were killed by decapitation under the same anesthesia as during the initial surgery, 24 h after the transplantation. At killing, a macroscopic visual post-mortem analysis was done to reveal any ischemic events in the hind leg muscles, kidneys, spleen, intestine and liver. Tissue samples from the left kidney, the right liver lobe, the spleen, the lungs, vastus muscle and bilateral femoral BM were dissected and snap frozen. Tissue samples were stored at −80 °C. Sagittal cryosections (14 μm) were cut serially and stored at −20 °C. We did not know what to expect, and therefore we started with four animals. Since we did not see any thrombosis or organ damage by i.a. infusion, we moved on to experiments in mice and rabbits to get additional information.
Immunohistochemistry
Sections were fixed in formaldehyde. A monoclonal mouse antibody was used for labeling human nuclei (anti-human nuclei, HuNu, MAB 1281, 1:200, EMD Millipore, UK). Sections were incubated overnight at 4 °C. Biotin block solution (Vector Laboratories Inc., Burlingame, CA, USA) was added to the primary antibody dilution. Furthermore, antibody conjugates were adsorbed with normal rabbit serum to minimize cross-reactivity. An avidin-conjugated secondary antibody was used. For analysis of adverse effects of the transplantation, such as thromboembolic complications, hematoxylin and eosin staining was performed according to Mayer’s protocol.19
qPCR
For extraction of total DNA, tissue was homogenized with a Tissuelyser (2 × 3 min, 25 Hz; Qiagen Retsch, Haan, Germany). DNeasy Blood and Tissue kit (Qiagen, Hilden, Germany) was used on Qiacube (Qiagen Instruments, Hombrechtikon, Switzerland) for isolation and purification of DNA. Three replicates of qPCR were made in TaqMan Fast Universal PCR Master Mix (Applied Biosystems (ABI), Foster City, CA, USA) and run on a qPCR machine 7900HT (ABI, Singapore, Singapore) with ABI software SDS v2.3. DNA (500 ng) was used in a total reaction volume of 15 μl for the double-dye-labeled human genomic DNA detection assay (PrimerDesign, Southampton, UK) and 100 ng DNA was used in the same total reaction volume for the reference gene, 18S rRNA (Hs99999901_s1; ABI). PCR cycling for the human genomic DNA detection assay was done according to the manufacturer's instructions: 95 °C for 10 min, and then 50 cycles of 95 °C for 15 s and 60 °C for 60 s. The cycling for 18S rRNA was qPCR: 95 °C for 20 s, and then 40 cycles of 95 °C for 1 s and 60 °C for 20 s. For ΔΔ Cq calculations, ABI software RQmgr v1.2.1 followed by DataAssist v3.0 were used. In the settings of the DataAssist software, the maximum allowable Ct value was set to 45, which was included in the calculations.
Intravital microscopy
Intravital microscopy was performed as described previously.20 Male C57bl/6 mice (n=2) weighing 20–30 g were catheterized in the left femoral artery using an 80-mm PI-127 catheter (Doccol Corp., Redlands, CA, USA). Five million rhodamine-labeled UCB cells in 200 μl saline with 10% AB serum were injected into the iliac artery for 60 s. Cell behavior in the cremaster muscle microcirculation was assessed using a Leitz Orthoplan microscope (Leica Microsystems, Wetzlar, Germany) equipped with a water immersion lens (x55, numerical aperture 0.8). Microscopic images were televised (WV-1550, WV-1900 cameras, Panasonic, Osaka, Japan) and recorded on a DVD recording unit.
Transplantation in large animals
Twelve New Zealand White rabbits weighing 3.5 kg were used in the study. Six received marrow-selective i.a. injections and six received i.v. UCB injections. Procedures were performed under general anesthesia and under sterile conditions on intubated rabbits connected to a servo ventilator. Anesthesia was induced by s.c. injection of 0.5 mL/kg Hypnorm (fentanyl citrate 0.315 mg/mL, fluanisone 10 mg/mL; Janssen Pharmaceuticals, Beerse, Belgium) combined with 5 mg diazepam (Actavis Group PTC, Hafnarfirdi, Iceland). Maintenance of anesthesia was achieved by continuous i.v. infusion of propofol-lipuro (Braun AB, Skene, Sweden) at a rate of 20 mL/h and i.v. injection of 0.1 mL Hypnorm every 30 min.
A 4F pediatric introducer (Terumo Medical Corporation, Tokyo, Japan) was inserted into the femoral artery through a surgical incision and a 4F catheter (Cobra Hydroglide; Cook, Bloomington, Indiana) was navigated to the contralateral femoral artery. A 1.2F micro-catheter (Magic; Balt Extrusion) was navigated to the femoral nutrient artery (FNA) and in that position 5 million cells from UCB dispersed in 1 mL saline with 10% AB serum were infused over 2.5 min. I.v. cell injections were performed through an i.v. line in the ear of the rabbit, using the same parameters as for i.a. transplantation. Twenty-four hours later, the animals were euthanized and dissected. The femoral bones were dissected and cut at both ends. The BM was snap frozen, and stored at −80 °C. Sagittal cryosections (14 μm) were cut serially and stored at −20 °C. For qPCR, 10 sagittal 50-μm-thick cryosections were sampled through the center of the BM.
Statistics
The Mann–Whitney test was performed to assess significance levels, comparing mean qPCR fold-change values for the i.a. group and the i.v. group in the left and right femora, respectively. Any value of P<0.05 was considered as significant.
Results
To investigate possible complications from i.a. transplantation of UCB we injected UCB through a micro-catheter into the thoracic aorta of rats (n=4). Rats injected by the i.v. route served as a control group (n=4). All rats were observed for weight loss, motility and spontaneous activity. After euthanasia, we performed extensive dissection with macroscopic investigation, followed by histological examination of the heart, lungs, liver, spleen, vastus muscles, kidneys and BM from femurs. We did not observe any negative effect on body weight in any of the animals after 24 h, which is a strong indicator that no important complications had occurred. Furthermore, no signs of peripheral limb ischemia were observed and all the animals showed normal gait, motility and exploratory behavior 2, 4 and 24 h after the operation. We then corroborated these behavioral findings with careful macroscopic and histological analysis of the organs mentioned above, and there was no evidence of infarction or hemorrhage (Table 1).
Next, we developed an animal model with the intention of having a truely selective i.a. approach to the BM (Figure 1). Thus, we employed rabbits as a model for endovascular intervention using clinical routine materials. It was possible to navigate to the FNA without causing any adverse events, using a transfemoral approach and clinical routine microcatheters designed for neurointerventional procedures (Figure 1). Normal flow rates were detected by digital subtraction angiography in the nutrient arteries, both before and after selective transplantation of cells (Figure 1b, c).
Angiography of the arterial system of the hip and thigh in the rabbit and of the femoral nutrient artery (FNA). (a) 3D rotational angiography during iodine contrast injection into the external iliac artery in the rabbit. The FNA (arrow) is seen branching from the femoral artery (FA) and entering the femur. (b) Digital subtraction angiography (DSA) showing a transaxial view of the rabbit femur with iodine contrast-media injection into the FNA opacifying the vascular system of the femoral BM. The FNA is seen traversing the cortical bone and entering the marrow cavity. (c) DSA showing a sagittal view of the rabbit femur with iodine contrast-media injection in the FNA. The arterial BM vascular system along its axis is visualized. The small arrows in (b) and (c) indicate the microcatheter tip position during contrast injection. The same catheter position was used for the superselective i.a. cell injections.
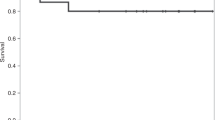
We extracted DNA from the BM of both femoral bones in all animals for analysis of human DNA. After primer design for amplification of human DNA without any amplification of rabbit DNA, qPCRs were performed with subsequent calculation of fold-change values. The baseline was set as the amount of human DNA in the marrow of one animal from the i.v. group. qPCR for human DNA from the targeted i.a. BM showed a significantly higher mean fold-change value of 15.76 vs 2.00 in the corresponding femoral BM in the i.v. group (n=12, P=0.0087) (Figure 3a). Briefly, selective i.a. infusion resulted in an eightfold increase in transplanted cells at 24 h. The morphological integrity of the transplanted cells was verified with immunohistochemical staining (Figures 2c and d). The amount of human DNA in the femoral marrow of i.v. transplanted animals was not significantly differerent from the amount in the contralateral marrow of i.a. injected animals (Figure 3b).
IHC staining of the femoral BM in the rabbit. Intravital microscopy in C57BL/6 mice. (a, b) Intravital microscopy of the cremaster muscle in a C57BL/6 mouse immediately after i.a. injection of 5 × 106 fluorescence-labeled human UCB cells into the iliac artery. (a) Cells entering the capillary bed by an arteriole. Blood flow direction is indicated by the arrow. (b) Cells leaving the capillary bed by a venule. Blood flow direction is indicated by the arrow. The slowly moving cells in the capillary bed are seen in both (a) and (b). In (c) photomicrograph showing immunostaining for HuNu (human nuclear antigen) positive cells in the femoral rabbit BM after injection of human UCB cells into the femoral nutrient artery. The magnification shows the immunohistochemically labeled cells. (d) Photomicrograph showing a section for the IHC from an i.v.-injected animal. Scale bars=20 μm.
Fold change in human DNA levels in rabbit femoral BM after selective i.a. injection into the FNA and after i.v. injection. Human DNA was isolated from BM in rabbits after injection into the left FNA (i.a.) and ear vein (i.v.). DNA levels were measured by qPCR. Level of human DNA in the left femoral BM from one animal in the i.v. group was normalized to a value of 1. (a) The mean level of human DNA was significantly higher in the selectively injected BM (**P=0.0087). (b) The mean levels of human DNA in the contralateral BM did not differ from the BMs after i.v. injection.
Furthermore, we used an in vivo microscopy mouse model to assess UCB cell behavior in the capillary bed following i.a. delivery (n=2). By infusing 5 million UCB cells with a fivefold higher concentration than in rabbit BM injections, into the iliac artery, we exposed the capillary bed of the cremaster muscle to a large number of cells, thus mimicking selective arterial infusion in the rabbit experiments. We detected cells entering the arterioles, with dispersion of the cells in the capillary bed and with cells leaving by the venules at different time points after the injection (Figures 2a and b). The number of cells exposed to the cremaster capillary bed was dramatically higher as compared with the conventional set-up using this technique with i.v. injections. We could follow the cellular-endothelial interaction and visualized rolling and adhesion of cells, which preceded cellular diapedesis. There was no evidence of acute mechanical obstruction of the capillaries due to the heavy cell load. This finding was corroborated by histological examination of the rabbit BM and rat organs, where no indications of adverse events—in the form of infarction or hemorrhaging—were detected (Table 1), thus indicating the safety of the procedure.
Discussion
We were able to amplify human DNA by qPCR from the BM of all 24 femurs from 12 rabbits that were injected with human UCB using either the i.v. or the marrow-selective arterial route. The BM from the animals in the i.v. group and the BM contralateral to injection in the i.a. group contained comparable levels of human DNA. This finding is expected, assuming that only a fraction of cells will engage the targeted BM in the first passage and that the remaining fraction of cells is given the same probability of BM homing as cells subjected to i.v. transplantation. The i.a. injected BM contained an eightfold increase in the amount of human DNA in immunohistochemically detected cells compared with that of i.v. controls.
These findings may be explained by improved homing in the i.a. injected BM due to increased exposure of UCB graft to the marrow niche. The cellular homing to the contralateral BM and homing to BM in the i.v. group supports this theory. It may also be explained by unspecific cell residence in the vascular bed of the BM, caused by capillary congestion from the heavy cell load or immunocomplex formation. Arguing against this is the fact that we were unable to detect any evidence for capillary congestion by cells using immunostaining for human nuclei, where we saw human nuclei-positive cells evenly scattered in regions containing marrow cells and not inside blood vessels. In addition, the in vivo microscopy experiments in mice did not reveal any capillary congestion using the same cell dose in a fivefold higher concentration.
Selective i.a. infusion requires endovascular intervention, a procedure associated with a very low frequency of intrinsic risk—although higher than for i.v. and intraosseous (i.o.) injection. The overall incidence of vascular complications in the adult population is <1%.21,22 Infectious complications following endovascular procedures are exceedingly rare in general, and there is antibiotic prophylaxis established for high-risk groups such as immunocompromized patients.23 In most adults, i.a. infusion can be performed using local anesthesia, but in pediatrics general anesthesia will be required. Pediatric patients are the most frequent recipients of UCB grafts.6, 7, 8, 9, 10 Among children in good condition at the time of transplant, general anesthesia is a low-risk procedure. I.o. infusion for UCB is also given during general anesthesia.18 However, in adults i.o. infusion may also be given using local anesthesia, but is associated with mild pain and some discomfort.24
I.o. UCB grafts have been given with a higher frequency of engraftment (96%) and a low incidence of acute GVHD in a study performed by Frassoni et al.18 However, the group from Minnesota did not find any advantage of i.o. infusion of UCB as compared with i.v. infusion.24 This was also in line with our randomized study using BM grafts.25 Therefore, an i.o. group would not add to our knowledge from i.v. infusion. The comparison was made between i.v., which is the gold standard and i.a., which was the experimental arm. One explanation for negative findings in the aforementioned i.o. and i.v comparisons may be that an intrabone injection actually targets the venous sinusoids within the marrow, that is, downstream of the vessels of the endosteal niche in the trabecular metaphysis, which is the suggested micro-anatomic target for hematopoietic cell homing.9,26 A marrow-selective i.a. approach is fundamentally different from i.o. infusion, as it allows natural passage of all injected cells throughout the full length of the marrow vasculature, thereby allowing full interaction between the hematopoietic niches and the injected cells.
In the present study, we chose not to include i.o. injection, since our experimental design does not allow assessment of functional engraftment. To be sure whether the i.a. or the i.o. approach outperforms i.v. injection in terms of functional engraftment and other outcome parameters such as survival using UCB grafts, a prospective randomized study is required. However, before this is undertaken, a pilot feasibility and safety study of clinical i.a. infusion of UCB grafts needs to be performed.
I.v. is certainly easier and less invasive than i.a. or i.o. infusion of any stem cell graft. Therefore, benefits like faster engraftment of neutrophils, platelets and erythrocytes, and better outcome with regard to fewer infections, and a lower TRM are required to make the i.a. procedure more attractive than the generally used i.v. approach. I.a. may bypass ‘pulmonary trapping’ as opposed to i.v. and i.o. infusion, and this may be a major advantage although it needs to be proven as stated above.15 I.a. infusion may also challenge other approaches to improve engraftment of UCB grafts, such as expansion of the cell number in the UCB graft which also hold some promise.27
Graft failure following UCB transplantation is estimated to be between 10 and 20%.8, 9, 10,13,16 Milder therapies for graft failure, such as boost of hematopoietic stem cells or donor lymphocyte infusion, are not possible with UCB transplants. Use of G-CSF may be attempted, but if this is unsuccessful, re-transplantation with a new UCB donor or haploidentical donor are the only possibilities.28 Re-transplantation is associated with high mortality, and is also expensive.29
In the present study, we started by comparing intra-aortal and i.v. injection of UCB in the rat to evaluate possible thromboembolic or other injection-related side effects in different organs. No adverse side effects were detected in assessments of vegetative behavior or histological organ analysis by hematoxylin-eosin staining. We assessed the effects of selective arterial infusion in a mouse model by intravital microscopy. Here we saw a large bolus of injected cells entering the capillary bed, with subsequent passage to the venules. Although we were able to load the capillary bed with a high number of cells, there was no evidence of cell congestion or entrapment, further confirming the safety of this procedure and suggesting that cell homing was the explanation for the increase in transplanted cells following i.a. delivery. This is primarily a feasibility and safety study and as we did not detect any thromboembolic or other injection-related side effects in the small animal models we moved on to the more clinically relevant rabbit model. Since no adverse reactions were detected and since statistically significant differences in engraftment were seen between i.v. and i.a. infusion even with 12 rabbits, the number of animals was considered to be sufficient.
In conclusion, we show that selective i.a. transplantation is a useful method for transplantation of UCB. We have also shown that it is possible to perform cell infusion into the nutrient arteries of the femoral BM and that this technique significantly increases organ exposure to the injected cells compared with i.v. infusion. In the clinical setting, it would be possible to use patient-tailored protocols with multiple injections to several deep marrow sites such as the vertebrae and the pelvis.
References
Humble JG, Newton KA . Technique of human bone-marrow transplants. Lancet 1958; 1: 142.
Tocantins LM . Special section-transplantation of bone marrow. Blood 1958; 13: 266–301.
Boncoraglio GB, Bersano A, Candelise L, Reynolds BA, Parati EA . Stem cell transplantation for ischemic stroke. Cochrane Database Syst Rev 2010; CD007231; doi:10.1002/14651858.CD007231.pub2.
Makkar RR, Smith RR, Cheng KE, Malliaras K, Thomson LE, Berman D et alIntracoronary cardiosphere-derived cells for heart regeneration after myocardial infarction (CADUCEUS): a prospective, randomised phase 1 trial. Lancet 2012; 379: 895–904.
Walter DH, Krankenberg H, Balzer JO, Kalka C, Baumgartner I, Schluter M et alIntraarterial administration of bone marrow mononuclear cells in patients with critical limb ischemia: a randomized-start, placebo-controlled pilot trial (PROVASA). Circ Cardiovasc Interv 2011; 4: 26–37.
Cohen Y, Nagler A . Umbilical cord blood transplantation—how, when and for whom? Blood Rev 2004; 18: 167–179.
Gluckman E, Rocha V, Arcese W, Michel G, Sanz G, Chan K-W et alFactors associated with outcomes of unrelated cord blood transplant: guidelines for donor choice. Exp Hematol 2004; 32: 397–407.
Wagner JE, Rosenthal J, Sweetman R, Shu XO, Davies SM, Ramsay NK et alSuccessful transplantation of HLA-matched and HLA-mismatched umbilical cord blood from unrelated donors: analysis of engraftment and acute graft-versus-host disease. Blood 1996; 88: 795–802.
Ballen KK . New trends in umbilical cord blood transplantation. Blood Rev 2005; 105: 3786–3792.
Rubinstein P, Carrier C, Scaradavou A, Kurtzberg J, Adamson J, Migliaccio AR et alOutcomes among 562 recipients of placental-blood transplants from unrelated donors. New Engl J Med 1998; 339: 1565–1577.
McKenzie JL . Human short-term repopulating stem cells are efficiently detected following intrafemoral transplantation into NOD/SCID recipients depleted of CD122+ cells. Blood 2005; 106: 1259–1261.
Lapidot T . How do stem cells find their way home? Blood 2005; 106: 1901–1910.
Staba Kelly S, Parmar S, De Lima M, Robinson S, Shpall E . Overcoming the barriers to umbilical cord blood transplantation. Cytotherapy 2010; 12: 121–130.
van der Loo JC, Ploemacher RE . Marrow- and spleen-seeding efficiencies of all murine hematopoietic stem cell subsets are decreased by preincubation with hematopoietic growth factors. Blood 1995; 85: 2598–2606.
Fischer UM, Harting MT, Jimenez F, Monzon-Posadas WO, Xue H, Savitz SI et alPulmonary passage is a major obstacle for intravenous stem cell delivery: the pulmonary first-pass effect. Stem Cells Dev 2009; 18: 683–692.
Barker JN, Weisdorf DJ, DeFor TE, Blazar BR, McGlave PB, Miller JS et alTransplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood 2005; 105: 1343–1347.
Panoskaltsis-Mortari A . In vivo imaging of graft-versus-host-disease in mice. Blood 2004; 103: 3590–3598.
Frassoni F, Gualandi F, Podestà M, Raiola AM, Ibatici A, Piaggio G et alDirect intrabone transplant of unrelated cord-blood cells in acute leukaemia: a phase I/II study. Lancet Oncol 2008; 9: 831–839.
Bancroft JD, FRCPath ASM . Theory and Practice of Histological Techniques, 4th edn. Churchill Livingstone, Edinburgh, 1996.
Thorlacius H, Lindbom L, Raud J . Cytokine-induced leukocyte rolling in mouse cremaster muscle arterioles in P-selectin dependent. Am J Physiol 1997; 272: H1725–H1729.
Hessel SJ, Adams DF, Abrams HL . Complications of angiography. Radiology 1981; 138: 273–281.
Nehler MR, Taylor LM, Porter JM . Iatrogenic vascular trauma. Semin Vasc Surg 1998; 11: 283–293.
Beddy P, Ryan JM . Antibiotic prophylaxis in interventional radiology—anything new? Tech Vasc Interv Radiol 2006; 9: 69–76.
Ramirez PA, Wagner JE, Brunstein CG . Going straight to the point: intra-BM injection of hematopoietic progenitors. Bone Marrow Transplant 2010; 45: 1127–1133.
Hagglund H, Ringden O, Agren B, Wennberg L, Remberger M, Rundquist L et alIntraosseous compared to intravenous infusion of allogeneic bone marrow. Bone Marrow Transplant 1998; 21: 331–335.
Ellis SL, Grassinger J, Jones A, Borg J, Camenisch T, Haylock D et alThe relationship between bone, hemopoietic stem cells, and vasculature. Blood 2011; 118: 1516–1524.
Shpall EJ, Quinones R, Giller R, Zeng C, Baron AE, Jones RB et alTransplantation of ex vivo expanded cord blood. Biol Blood Marrow Transplant 2002; 8: 368–376.
Mattsson J, Ringdén O, Storb R . Graft failure after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2008; 14: 165–170.
Svahn BM, Remberger M, Alvin O, Karlsson H, Ringden O . Increased costs after allogeneic haematopoietic SCT are associated with major complications and re-transplantation. Bone Marrow Transplant 2012; 47: 706–715.
Acknowledgements
Financial support was provided by Karolinska Institutet, the Stockholm County Council, the Swedish Society of Medicine, the Cancer Foundation, the Swedish Research Council, Hjärnfonden, the Children's Cancer Foundation, the Stockholm Cancer Society and Söderbergska Stiftelserna. This study is also a part of the project Fighting Stroke (Uppdrag Besegra Stroke), supported by the Swedish Heart-Lung Foundation, Karolinska Institutet, Friends of Karolinska Institutet USA and the Swedish Order of St John Scientific Committee of Fighting Stroke (Uppdrag Besegra Stroke): Nils Wahlgren (Chair), Niaz Ahmed, Maaret Castrén, Ulf Eriksson, Jonas Frisén, Ulf Hedin, Staffan Holmin, Mikael Svensson and Mia von Euler. The authors wish to thank Johanna Doshé, Gunilla Nilsson and Pellina Jansson for excellent support with animal endovascular intervention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Arnberg, F., Lundberg, J., Kenne, E. et al. Superselective intra-arterial umbilical cord blood administration to BM in experimental animals. Bone Marrow Transplant 49, 1486–1491 (2014). https://doi.org/10.1038/bmt.2014.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2014.190