Abstract
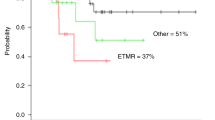
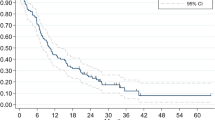
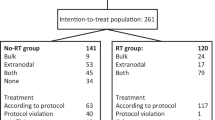
In an effort to improve survival and reduce late adverse effects of radiation therapy (RT), 25 children <3 years of age with malignant brain tumors received tandem high-dose chemotherapy (HDCT) and auto-SCT following six cycles of induction chemotherapy. RT was either not given or deferred until 3 years of age if the patient was in CR after tandem HDCT/auto-SCT. Tumors relapsed or progressed in nine patients (five during induction treatment), and two of these patients survived after receiving salvage treatment, including RT. Two patients died due to toxicities during tandem HDCT/auto-SCT. A total of 16 patients survived to a median follow-up period of 52 months (range 18–96) from the time of diagnosis. Four of these patients did not receive RT, two received local RT (L-RT), three received craniospinal RT (CSRT), and seven received both L-RT and CSRT. The 5-year OS and EFS rates were 67.8±9.4% and 55.5±10.0%, respectively. Neuroendocrine and neurocognitive functions evaluated 3 years after tandem HDCT/auto-SCT were acceptable. Our results indicate that tandem HDCT/auto-SCT may improve survival in young children with malignant brain tumors with an acceptable level of risk of long-term toxicity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Copeland DR, deMoor C, Moore BD, Ater JL . Neurocognitive development of children after a cerebellar tumor in infancy: a longitudinal study. J Clin Oncol 1999; 17: 3476–3486.
Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE . Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol 2004; 5: 399–408.
Lannering B, Marky I, Lundberg A, Olsson E . Long-term sequelae after pediatric brain tumors: their effect on disability and quality of life. Med Pediatr Oncol 1990; 18: 304–310.
Duffner PK . Long-term effects of radiation therapy on cognitive and endocrine function in children with leukemia and brain tumors. Neurologist 2004; 10: 293–310.
Duffner PK, Horowitz ME, Krischer JP, Friedman HS, Burger PC, Cohen ME et al. Postoperative chemotherapy and delayed radiation in children less than three years of age with malignant brain tumors. N Engl J Med 1993; 328: 1725–1731.
Geyer JR, Zeltzer PM, Boyett JM, Rorke LB, Stanley P, Albright AL et al. Survival of infants with primitive neuroectodermal tumors or malignant ependymomas of the CNS treated with eight drugs in 1 day: a report from the Childrens Cancer Group. J Clin Oncol 1994; 12: 1607–1615.
Grill J, Sainte-Rose C, Jouvet A, Gentet JC, Lejars O, Frappaz D et al. Treatment of medulloblastoma with postoperative chemotherapy alone: an SFOP prospective trial in young children. Lancet Oncol 2005; 6: 573–580.
Matthay KK, Reynolds CP, Seeger RC, Shimada H, Adkins ES, Haas-Kogan D et al. Long-term results for children with high-risk neuroblastoma treated on a randomized trial of myeloablative therapy followed by 13-cis-retinoic acid: a children's oncology group study. J Clin Oncol 2009; 27: 1007–1013.
Berthold F, Boos J, Burdach S, Erttmann R, Henze G, Hermann J et al. Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomised controlled trial. Lancet Oncol 2005; 6: 649–658.
Marachelian A, Butturini A, Finlay J . Myeloablative chemotherapy with autologous hematopoietic progenitor cell rescue for childhood central nervous system tumors. Bone Marrow Transplant 2008; 41: 167–172.
Mason WP, Grovas A, Halpern S, Dunkel IJ, Garvin J, Heller G et al. Intensive chemotherapy and bone marrow rescue for young children with newly diagnosed malignant brain tumors. J Clin Oncol 1998; 16: 210–221.
Fangusaro J, Finlay J, Sposto R, Ji L, Saly M, Zacharoulis S et al. Intensive chemotherapy followed by consolidative myeloablative chemotherapy with autologous hematopoietic cell rescue (AuHCR) in young children with newly diagnosed supratentorial primitive neuroectodermal tumors (sPNETs): report of the Head Start I and II experience. Pediatr Blood Cancer 2008; 50: 312–318.
Chi SN, Gardner SL, Levy AS, Knopp EA, Miller DC, Wisoff JH et al. Feasibility and response to induction chemotherapy intensified with high-dose methotrexate for young children with newly diagnosed high-risk disseminated medulloblastoma. J Clin Oncol 2004; 22: 4881–4887.
Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE et al. Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St Jude Medulloblastoma-96): long-term results from a prospective, multicentre trial. Lancet Oncol 2006; 7: 813–820.
Sung KW, Yoo KH, Cho EJ, Koo HH, Lim do H, Shin HJ et al. High-dose chemotherapy and autologous stem cell rescue in children with newly diagnosed high-risk or relapsed medulloblastoma or supratentorial primitive neuroectodermal tumor. Pediatr Blood Cancer 2007; 48: 408–415.
Tekautz TM, Fuller CE, Blaney S, Fouladi M, Broniscer A, Merchant TE et al. Atypical teratoid/rhabdoid tumors (ATRT): Improved survival in children 3 years of age and older with radiation therapy and high-dose alkylator-based chemotherapy. J Clin Oncol 2005; 23: 1491–1499.
Chen YW, Wong TT, Ho DM, Huang PI, Chang KJ, Shiau CY et al. Impact of radiotherapy for pediatric CNS atypical teratoid/rhabdoid tumor (single institute experience). Int J Radiat Oncol Biol Phys 2006; 64: 1038–1043.
Chi SN, Zimmerman MA, Yao X, Cohen KJ, Burger P, Biegel JA et al. Intensive multimodality treatment for children with newly diagnosed CNS atypical teratoid rhabdoid tumor. J Clin Oncol 2009; 27: 385–389.
Rutkowski S, Bode U, Deinlein F, Ottensmeier H, Warmuth-Metz M, Soerensen N et al. Treatment of early childhood medulloblastoma by postoperative chemotherapy alone. N Engl J Med 2005; 352: 978–986.
Acknowledgements
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (No. 0520300).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sung, K., Lim, D., Lee, S. et al. Tandem high-dose chemotherapy and auto-SCT for malignant brain tumors in children under 3 years of age. Bone Marrow Transplant 48, 932–938 (2013). https://doi.org/10.1038/bmt.2012.263
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2012.263