Abstract
Background:
We investigated selumetinib (AZD6244, ARRY-142886), an oral, potent, and highly selective, allosteric MEK1/2 inhibitor, plus platinum-doublet chemotherapy for patients with advanced/metastatic non-small cell lung cancer.
Methods:
In this Phase I, open-label study (NCT01809210), treatment-naïve patients received selumetinib (50, 75, 100 mg BID PO) plus standard doses of gemcitabine or pemetrexed plus cisplatin or carboplatin. Primary objectives were safety, tolerability, and determination of recommended Phase II doses.
Results:
Fifty-five patients received treatment: selumetinib 50 or 75 mg plus gemcitabine/cisplatin (n=10); selumetinib 50 mg plus gemcitabine/carboplatin (n=9); selumetinib 50, 75 or 100 mg plus pemetrexed/carboplatin (n=21); selumetinib 75 mg plus pemetrexed/cisplatin (n=15). Most frequent adverse events (AEs) were fatigue, nausea, diarrhoea and vomiting. Grade ⩾3 selumetinib-related AEs were reported in 30 (55%) patients. Dose-limiting toxicities (all n=1) were Grade 4 anaemia (selumetinib 75 mg plus gemcitabine/cisplatin), Grade 4 thrombocytopenia/epistaxis and Grade 4 thrombocytopenia (selumetinib 50 mg plus gemcitabine/carboplatin), Grade 4 febrile neutropenia (selumetinib 100 mg plus pemetrexed/carboplatin), and Grade 3 lethargy (selumetinib 75 mg plus pemetrexed/cisplatin). Partial responses were confirmed in 11 (20%) and unconfirmed in 9 (16%) patients.
Conclusions:
Standard doses of pemetrexed/carboplatin or pemetrexed/cisplatin were tolerated with selumetinib 75 mg BID. The selumetinib plus gemcitabine-containing regimens were not tolerated.
Similar content being viewed by others
Main
Despite advances in the diagnosis, imaging, staging, and treatment of non-small cell lung cancer (NSCLC), the estimated overall 5-year survival rate for patients in Europe is only 11% (D'Addario et al, 2010). A number of molecular abnormalities have been shown to be characteristic of certain lung cancers and are used to guide first-line treatment. Patients with tumours harbouring activating epidermal growth factor receptor (EGFR) mutations receive particular benefits from selective treatment with an EGFR tyrosine kinase inhibitor, while patients with tumours that contain the fusion oncogene EML4-ALK will benefit from targeting its tyrosine kinase activity using an ALK inhibitor, such as crizotinib (Novello et al, 2016). However, there are no approved targeted therapies for the majority of advanced NSCLC patients that have no known or characterised molecular abnormalities and platinum-based doublet chemotherapy is the first-line treatment for the vast majority of patients.
Activation of the RAS/RAF/MEK/ERK (RAS-ERK) mitogen-activated protein kinase pathway is implicated in cellular proliferation and is central to driving cancer growth and progression (Davies et al, 2002; Roberts and Stinchcombe, 2013). Activation of this pathway can be driven by somatic mutations, and KRAS mutations are found in up to 34% of NSCLC (Shepherd et al, 2013). MEK1/2 are critical components of the RAS-ERK pathway and therefore inhibition of MEK1/2 may be effective in patients with NSCLC. Selumetinib (AZD6244, ARRY-142886) is an oral, potent, and highly selective, allosteric MEK1/2 inhibitor (Yeh et al, 2007), with a short half-life (Banerji et al, 2010; Denton and Gustafson, 2011). In a prospective study, selumetinib in combination with docetaxel, as second-line treatment for patients with KRAS-mutant (KRASm) advanced NSCLC, improved progression-free survival (PFS) and objective response rate compared with placebo combined with docetaxel (Jänne et al, 2013). The combination safety profile was consistent with those of the individual components and adverse events (AEs) were manageable with appropriate guidance and clinical practice (Shepherd et al, 2000; Hanna et al, 2004; Hainsworth et al, 2010; Jänne et al, 2013). Following these results, selumetinib was evaluated in combination with docetaxel as second-line treatment in patients with KRASm NSCLC in the Phase III SELECT-1 study (NCT01933932) (Jänne et al, 2016c).
Following the promising Phase II results of second-line selumetinib, and in parallel to the Phase III SELECT-1 study, the potential use of selumetinib in the first-line setting was investigated in patients unselected for KRAS mutation status, to test the hypothesis of MEK inhibition in the context of other non-KRASm modes of pathway activation. To do this, the appropriate treatment combinations of selumetinib plus chemotherapy were investigated using platinum-doublet regimens that are standard of care for treatment-naïve patients, namely cisplatin or carboplatin, in combination with either pemetrexed or gemcitabine (Reck et al, 2014). Here we report results from a dose-finding Phase I study (NCT01809210), which assessed the safety, tolerability, and preliminary efficacy of selumetinib in combination with first-line chemotherapy regimens, in patients with NSCLC, unselected for KRAS mutation status.
Patients and methods
Patients
Patients aged 18 years or older with histologically or cytologically confirmed, locally advanced (stage IIIB) or metastatic (stage IV) NSCLC, eligible for standard first-line platinum-doublet treatment for NSCLC but unsuitable for radical treatment were included in the study. Other eligibility criteria included World Health Organization performance status (WHO-PS) of 0–1 and radiologically measurable disease. Patients were not selected based on KRAS mutation status, but local KRAS test results were recorded if known.
Patients were excluded if they had received prior systemic anti-cancer treatment for advanced NSCLC. Previous adjuvant chemotherapy, prior surgery, or radiotherapy for curative intent was permitted if they occurred >6 months prior to starting study treatment. Other exclusion criteria included: treatment with potent inhibitors or inducers of cytochrome P450 (CYP) 3A4/5, CYP2C19 and CYP1A2 within 2 weeks of the first dose of study treatment; symptomatic brain metastases or spinal cord compression; history of central serous retinopathy or retinal vein occlusion; uncontrolled glaucoma or intraocular pressure >21 mm Hg.
Study design and treatment
This was a Phase I/Ib, open-label, multicentre study of selumetinib in combination with platinum-doublet chemotherapy regimens, following a ‘rolling six’ design with cohorts of at least three and up to six evaluable patients. The study was designed to allow an investigation of the optimal combination dose while ensuring the safety of patients with intensive safety monitoring.
The primary study objective was to investigate the safety and tolerability, and to determine the recommended Phase II dose (RP2D) of selumetinib when administered in combination with first-line chemotherapy regimens. Secondary objectives included assessment of pharmacokinetics (PK) of selumetinib, its metabolite N-desmethyl selumetinib, gemcitabine/pemetrexed and cisplatin/carboplatin when administered in combination and evaluation of tumour response to assess preliminary efficacy of the treatment combinations using Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST v1.1).
Selumetinib was administered orally twice-daily (BID) in continuous 21-day cycles. The starting dose of selumetinib was chosen as 50 mg being two-thirds of the combination dose used in two Phase II studies (Kirkwood et al, 2012; Jänne et al, 2013), increasing in 25 mg increments. Doses administered were selumetinib 50 or 75 mg BID plus standard doses (for first-line treatment of NSCLC) of gemcitabine (1250 mg m−2) or pemetrexed (500 mg m−2) plus cisplatin (75 mg m−2) or carboplatin (AUC=5). Only patients with non-squamous histology received pemetrexed as per the approved indication. An additional dose-finding cohort of selumetinib 100 mg BID plus pemetrexed and carboplatin was included. Primary prophylactic use of granulocyte colony stimulating factors (GCSF) was not permitted, but GCSF was permitted after Cycle 1.
Treatment was continued until a treatment or study discontinuation criterion was met. Patients who discontinued one, or both, chemotherapy agents were able to continue receiving selumetinib monotherapy if there was evidence of continuing clinical benefit as assessed by the investigator. The study was designed to include an optional dose expansion study at the recommended Phase II combination dose. The safety review committee recommended that the pemetrexed/cisplatin cohort be expanded to ascertain the safety and tolerability of this regimen, in combination with the recommended Phase II dose of selumetinib 75 mg BID.
The study followed the principles of the Declaration of Helsinki and Good Clinical Practice guidelines of the International Conference on Harmonisation. All patients provided written informed consent prior to their participation in the study. Approval was obtained from the local institutional review board at each participating site and complied with local country regulations.
Assessments
Safety was assessed in terms of AEs, laboratory data, vital signs, electrocardiogram changes, physical examinations, echocardiogram/multigated acquisition scan, and ophthalmologic examinations. AEs were graded using the National Cancer Institute CTCAE version 4.0. Dose-limiting toxicity (DLT) was assessed during the first treatment cycle (a full definition of DLT is provided in Supplementary Digital Content 1, Supplementary Methods). Patients were followed up for 28±7 days following discontinuation of selumetinib.
Plasma samples were collected for PK assessments at baseline and on Cycle 1 Day 8 and Cycle 2 Day 1 for selumetinib and its metabolite N-desmethyl selumetinib, gemcitabine and its metabolite deoxy-1,1-difuorouridine (dFdu), pemetrexed, cisplatin (total and/or unbound platinum) and carboplatin (total and/or unbound platinum) (full details of the PK analysis are given in Supplementary Digital Content 1, Supplementary Methods) (Severin et al, 2016).
Tumour response to treatment was assessed using RECIST v1.1 assessment of computed tomography or magnetic resonance imaging scans at screening and then every 6 weeks for 6 months and every 12 weeks thereafter until discontinuation of selumetinib.
Statistical analyses
Safety data were summarised for all patients who received at least one dose of selumetinib. The PK analysis was summarised for all patients with sufficient samples to provide an adequate profile, with no important AEs or protocol deviations that may have impacted PK. Plasma PK parameters were derived using standard non-compartmental methods and actual elapsed time from dosing. Efficacy data were summarised for all patients who received at least one dose of selumetinib with a baseline tumour assessment. Statistical analyses were performed by Phastar (London, UK) under the direction of the Biostatistics Group, AstraZeneca, (London, UK) using SAS software Version 9.1.3 or later (SAS Institute, Inc. Cary, NC, USA).
Results
Patient disposition
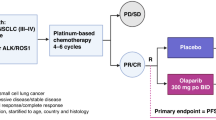
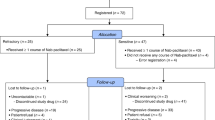
Between 4 April 2013 and 30 September 2015, 76 patients were enrolled; 21 failed to meet the eligibility criteria and 55 received study treatment with selumetinib and first-line chemotherapy regimens across seven dose escalation cohorts (Figure 1). Ten patients were treated with gemcitabine and cisplatin; nine with gemcitabine and carboplatin; 21 with pemetrexed and carboplatin and 15 with pemetrexed and cisplatin. Median treatment duration of selumetinib was 84 days (range, 4–266); median number of cycles of chemotherapy received are displayed in Supplementary Table 1. All patients discontinued selumetinib, due to the following reasons: AE (23 patients, 41.8%), condition under investigation worsened (21 patients, 38.2%), subject decision (11 patients, 20.0%). Nine patients died during the study; two deaths were attributed to serious AEs of myocardial infarction, two to disease progression and AEs (both colonic perforation; one considered to be causally related to gemcitabine and cisplatin) and five to disease progression alone. No deaths were considered related to selumetinib.
Demographics and baseline disease characteristics
Overall, demographics were as expected in patients with advanced NSCLC and were generally balanced between treatment groups (Table 1), with the exception of the male:female ratio of patients treated with pemetrexed-cisplatin (2 : 1; n=15). This was due to the sequential enrolment process and the variable number of patients assigned to each cohort. Most patients (66%) had a WHO-PS of 1 and the majority had adenocarcinoma (67%). Fifty patients (91%) had metastatic disease. KRAS mutation status was determined retrospectively using archival tumour samples in 28 patients (51%); six (11%) had confirmed KRASm NSCLC. Of these six patients, five had adenocarcinoma histology and for one patient the histology could not be determined.
Safety
In total, five DLTs were reported (Supplementary Table 2). The gemcitabine and cisplatin combination was tolerated at selumetinib 50 mg dose level. In the selumetinib 75 mg plus gemcitabine and cisplatin group, one of four evaluable patients experienced a DLT of Grade 4 anaemia; enrolment at selumetinib 75 mg dose level was stopped by the study sponsor when two serious AEs of large bowel perforation (at selumetinib dose levels 50 and 75 mg), considered not related to selumetinib by the investigators, were reported for this combination. The combination of selumetinib 50 mg plus gemcitabine and carboplatin was declared non-tolerated, and two of seven evaluable patients experienced DLTs: one Grade 4 thrombocytopenia, and one Grade 4 thrombocytopenia plus Grade 4 epistaxis. The pemetrexed and carboplatin combination was tolerated at selumetinib 50 and 75 mg dose levels; no DLTs were reported. One of six evaluable patients in the selumetinib 100 mg plus pemetrexed and carboplatin group experienced a DLT of Grade 4 febrile neutropenia. Although DLT criteria were not reached for the selumetinib 100 mg cohort, nine (75%) patients required a dose modification and therefore this was not considered suitable for evaluation in subsequent Phase II studies. The combination of pemetrexed and cisplatin was not explored at selumetinib 50 mg dose level due to emerging data from a Phase Ib trial study (NCT01783197) investigating selumetinib (50 or 75 mg BID) in combination with cisplatin and pemetrexed or carboplatin and paclitaxel in patients with previously untreated metastatic NSCLC. The trial demonstrated that selumetinib 75 mg BID was generally well tolerated in these combinations (Nicholas et al, 2015). In the current study, selumetinib in combination with pemetrexed and cisplatin was found to be tolerated at 75 mg from an expanded cohort of a total of 12 evaluable patients: one patient in this group experienced a DLT of Grade 3 lethargy. The RP2Ds were identified as selumetinib 75 mg BID plus standard doses of pemetrexed/carboplatin and pemetrexed/cisplatin. No RP2Ds were defined for treatment with gemcitabine; the carboplatin combination was declared non-tolerated, and the combinations with cisplatin were discontinued due to concerns about potential tolerability of this regimen and the fatalities related to large bowel perforation.
The most commonly reported AEs overall were nausea (73%), diarrhoea (55%), fatigue (55%), and vomiting (55%) (Table 2). These were the most common AEs in each treatment arm except for selumetinib plus gemcitabine/carboplatin, in which patients reported fatigue, neutropenia, and thrombocytopenia most commonly (all 67%). In total, 44 (80%) patients experienced an AE of Grade ⩾3; the most common, regardless of causality, were neutropenia (14, 26%), anaemia (12, 22%), and thrombocytopenia (11, 20%). Thirty (55%) patients experienced an AE of Grade ⩾3 causally related to selumetinib. AEs leading to a dose interruption or discontinuation of selumetinib were observed in 29 (53%) and 23 (42%) patients, respectively. Serious AEs were observed in 33 (60%) patients. In 17 (31%) patients, serious AEs were considered causally related to selumetinib by the investigator, of which 6 (11%) were thrombocytopenia.
AEs of particular interest due to their causal relationship to selumetinib (as assessed by investigator) included facial oedema, rash, retinal events, and decreases in left ventricular ejection fraction (LVEF). Six patients experienced maculo-papular rash (all Grade 1/2) with one patient discontinuing treatment due to this AE; however, there were no cases of rash leading to a DLT. Twelve patients experienced peripheral oedema with one instance leading to treatment discontinuation; two patients experienced facial oedema. Retinal vein occlusion, retinal pigment epithelial detachment, and central serous retinopathy were each reported in one patient receiving pemetrexed and cisplatin plus selumetinib 75 mg BID. No AEs of cardiac failure were reported. Decreased LVEF causally related to selumetinib was reported in two patients (both Grade 2). One patient who received gemcitabine and cisplatin plus selumetinib 50 mg BID experienced decreased LVEF 85 days after the first dose of study treatment. LVEF was 64% at screening and selumetinib was permanently discontinued due to the event, which was assessed by the investigator as causally related to selumetinib, when LVEF decreased to 51%. Another patient who received pemetrexed and carboplatin plus selumetinib 50 mg BID experienced decreased LVEF with onset 170 days after the first dose of study treatment. Echocardiography at screening showed an LVEF of 62% with atrial dilation, which decreased to 33% and selumetinib was interrupted. Selumetinib 50 mg was continued after 44 days when LVEF had increased to 41%. At the time of treatment discontinuation, LVEF was 49% and the event was recorded as ongoing (78 days after onset). Echocardiography showed a mildly dilated left ventricular cavity with mildly impaired systolic function and moderate dilation. Selumetinib was permanently discontinued due to the event which was assessed by the investigator as causally related to selumetinib.
Pharmacokinetics
PK analyses showed that the steady-state PK of selumetinib and N-desmethyl selumetinib were generally similar when administered with chemotherapy across the combination regimens (Figure 2). Following oral administration of 50, 75, and 100 mg BID, selumetinib was rapidly absorbed with a median time to reach maximum plasma concentration (tmax) of 1.00–1.75 h post-dose. No marked trend in time to reach maximum plasma concentration at steady state (tss,max) was observed across selumetinib dose or combination chemotherapies. With a low number of evaluable PK parameters in some treatment groups, selumetinib inter-patient variability of systemic exposure to selumetinib was generally moderate to high, with geometric mean CV% for the area under the plasma concentration time curve in the dosing interval (AUCτ) and the maximum observed plasma concentration at steady state (Css,max) ranging from 15%–57% and 23%–76%, respectively, across treatment arms on Cycle 1 Day 8 and Cycle 2 Day 1. Visual assessment of PK parameters across all treatment groups did not reveal any major differences in systemic exposure, although there was a trend towards lower AUCτ and Css,max in patients receiving selumetinib 50 mg plus gemcitabine and cisplatin, with individual estimates ranging from 1590 to 2240 ng h ml−1 and 276–686 ng ml−1, respectively, across both treatment cycles. However, this trend was not apparent in patients receiving selumetinib 75 mg plus gemcitabine and cisplatin. Mean metabolite:parent AUCτ ratios indicated that N-desmethyl selumetinib represented approximately 3–8% of selumetinib systemic exposure, with no apparent trend in PK across treatment arms. The PK of gemcitabine, dFdu, pemetrexed, cisplatin, and carboplatin were generally similar across the doses of selumetinib administered for the various combination chemotherapy regimens.
Scatter plots of selumetinib (A–C) and N -desmethyl selumetinib (D–E) PK parameters (PK analysis set). AUCT = area under the plasma concentration time curve in the dosing interval; Carb = carboplatin; Css,max = maximum observed plasma concentration at steady state; Cis = cisplatin; CL/F = apparent oral plasma clearance; Gem = gemcitabine; Pem = pemetrexed; Sel = selumetinib.
Efficacy
All 55 patients treated were evaluable for response, a confirmed partial response was observed in 11 (20%) patients, and an unconfirmed partial response in 9 (16%), resulting in an estimated response rate of 36%. Figure 3 shows best percentage change in tumour size. In addition, 21 (38%) patients had stable disease at ⩾6 weeks (Supplementary Table 3). Confirmed partial responses were seen in: 3/10 (30%) patients receiving selumetinib plus gemcitabine/cisplatin, 2/9 (22%) patients receiving selumetinib plus gemcitabine/carboplatin (unconfirmed partial response in 3/9, 33%), 4/21 (19%) patients receiving selumetinib plus pemetrexed/carboplatin (unconfirmed complete or partial response in 4/21, 19%), and 2/15 (13%) patients in the selumetinib plus pemetrexed/cisplatin treatment arm (unconfirmed complete or partial response in 2/15, 13%). Of the six patients with KRASm NSCLC detected using a local test, best objective response was 1 partial response; 3 stable disease; 2 progressive disease.
Best percentage change in tumour size. Abbreviations: carb=carboplatin; cis=cisplatin; gem=gemcitabine; pem=pemetrexed; sel=selumetinib. n=47. Eight patients were excluded due to incomplete post-baseline assessments of tumour response. Best change in target lesion size is the maximum reduction from baseline or the minimum increase from baseline in the absence of a reduction. *Patients with detected KRAS mutation.
Discussion
In the first-line setting, platinum-doublet chemotherapy represents the standard of care for patients with advanced NSCLC without EGFR activating mutation or ALK gene rearrangement, but objective response rates are low (15–31%) and median survival is generally up to approximately 10 months (Schiller et al, 2002; Sandler et al, 2006; Scagliotti et al, 2008). Selumetinib, given in combination with docetaxel, improved response rates and PFS in the second-line setting (Jänne et al, 2013); therefore, we investigated whether selumetinib could be safely and effectively combined with platinum-doublet chemotherapy in the first-line setting.
In the SELECT-3 study presented here, we identified recommended Phase II doses of selumetinib 75 mg BID when combined with standard doses of pemetrexed and cisplatin or pemetrexed and carboplatin, which were tolerated with AE profiles consistent with the individual agents. The combinations with gemcitabine were not tolerated and a recommended Phase II dose was not determined.
The overall safety profile of selumetinib in combination with pemetrexed plus carboplatin or cisplatin was acceptable, and there were no selumetinib-related deaths in any treatment arm. Many of the AEs were those that would be anticipated from the administration of platinum-doublet chemotherapy. The safety profile presented here is consistent with a Phase Ib trial by the National Cancer Institute of Canada (NCIC) investigating selumetinib (50 or 75 mg BID) combined with cisplatin and pemetrexed or carboplatin and paclitaxel in patients with previously untreated metastatic NSCLC (n=22) (Nicholas et al, 2015). In the NCIC study, the most common selumetinib-related toxicities were mild gastrointestinal and skin-related AEs. We also observed generally mild skin and gastrointestinal toxicities, although in the current study, six patients in the cisplatin-containing treatment groups experienced ⩾Grade 3 nausea (three each in gemcitabine and cisplatin plus selumetinib 75 mg, and pemetrexed and cisplatin plus selumetinib 75 mg groups). Owing to the known emetogenic properties of cisplatin, we subsequently agreed to a standardised anti-emetic regimen between participating trial centres to include 3 days of steroids, a 5-HT3 receptor antagonist, and aprepitant, and this would be recommended for any subsequent studies of these combinations.
In our study the rate of Grade 3–4 neutropenia was lower than that reported in the NCIC study (25% vs 44%) (Nicholas et al, 2015). In a previous Phase II study of selumetinib in combination with docetaxel, rates of Grades 3–4 neutropenia were 67% in the selumetinib plus docetaxel group, and 55% in the placebo plus docetaxel group, without prophylactic GCSF treatment (Jänne et al, 2013). In the current study, AEs were managed using safety management guidelines according to standard clinical practice, hence commonly occurring AEs were effectively managed using specific treatment algorithms and GCSF was permitted after Cycle 1. Prophylactic GCSF was also used in the Phase III SELECT-1 study (Jänne et al, 2016b). In the present study, two patients experienced Grade 2 decreased LVEF considered causally related to selumetinib. Reversible, asymptomatic reductions in LVEF have been reported in a small number of patients in some studies of selumetinib (Banerji et al, 2010). As such, mandatory safety monitoring of LVEF with scheduled echocardiography assessments and guidance to assist in the early diagnosis and management of decreased LVEF have been incorporated into trial protocols, including that of the SELECT-3 trial.
The recommended Phase II dose was not determined for the gemcitabine-containing regimens, due to fatalities of unknown relationship to the combinations and therefore a tolerable regimen was not identified for patients with squamous NSCLC in this study. The carboplatin combination was not tolerated, while the combinations with cisplatin were discontinued due to fatalities related to colonic perforation: two patients (one receiving selumetinib 50 mg plus gemcitabine/cisplatin; one receiving selumetinib 75 mg plus gemcitabine/cisplatin) experienced large intestine perforation leading to death 50 days and 25 days after the first dose of selumetinib, respectively. These AEs were not deemed by the investigator to be related to selumetinib in the present study, although this effect has been reported with other MEK inhibitors (Minor et al, 2015). By contrast, a manageable toxicity profile was reported at a dose of 75 mg BID selumetinib plus gemcitabine 1000 mg m−2 and cisplatin 25 mg m−2 in a Phase Ib trial in patients with advanced or metastatic biliary tract cancer (Bridgewater et al, 2016). However, this may be due to the lower doses of both gemcitabine and cisplatin, and the fractioned regimen of cisplatin, or the variation in comorbidities of the patients enrolled.
Combination therapy did not appear to show any marked effect on the PK profile of selumetinib or its metabolite N-desmethyl selumetinib. It was noted that there was a trend for lower systemic exposure to selumetinib in the selumetinib 50 mg plus gemcitabine and cisplatin treatment group, but due to the limited data in this study and high variability of selumetinib PK, no conclusions can be made regarding the significance of this finding. While the study was not designed to assess whether selumetinib affects the exposure of the chemotherapies investigated, the available data did not find any marked differences in the PK of gemcitabine, pemetrexed, cisplatin and carboplatin, across the doses of selumetinib administered for the various combination chemotherapy regimens.
Preliminary anti-tumour activity was observed across all treatment arms. Confirmed partial responses were detected in 20% of patients and 38% of patients had stable disease at ⩾6 weeks. Data for each arm were consistent with previous reports of chemotherapy alone (Karampeazis et al, 2016; Langer et al, 2016; Park et al, 2017a,2017b). Six patients (40%) in the pemetrexed plus cisplatin group opted to continue with the standard maintenance therapy of pemetrexed. Maintenance therapy with selumetinib was not robustly explored in this study.
This trial was initiated before immunomodulatory therapies were approved for the treatment of patients with NSCLC in the second-line setting. Based on encouraging results from studies of these agents (Besse et al, 2015; Gettinger et al, 2016; Rizvi et al, 2016), several Phase III trials are currently evaluating immunotherapies in the first-line setting as monotherapy, in combination with different immunotherapies, or with platinum-based chemotherapy. The Keynote-024 study has shown higher response rate, PFS and overall survival for pembrolizumab when compared with standard platinum-based doublet chemotherapy as first-line treatment for patients with advanced NSCLC with high levels (>50%) of PD-L1 expression (Reck et al, 2016). Despite the rapidly changing treatment landscape, it is not anticipated that all patients will benefit from immunotherapy, particularly those patients whose tumours are PD-L1 negative or low (Qin et al, 2016). Therefore, it is expected that platinum-doublet chemotherapy will continue to be used in the first-line setting for certain patient populations, especially if PD-L1 testing becomes more widely used, and will likely be used in relapse for patients following first-line immunotherapy. However, it should be noted that the efficacy and safety profile of subsequent treatments may be altered following first-line immune checkpoint inhibition. Selumetinib is being investigated in combination with the PD-L1 inhibitor durvalumab for patients with advanced solid tumours, including lung cancer, in the Phase I SELECT-4 trial (NCT02586987).
A limitation of the present study is that patients were not prospectively evaluated for KRAS mutation status, therefore sub-populations of patients deriving clinical benefit could not be identified. Limited KRAS mutation information was obtained from local test results using different methodologies with various limits of detection and coverage. The rate of KRASm in adenocarcinoma and squamous NSCLC is approximately 34% and 6%, respectively (Shepherd et al, 2013), with a higher incidence in Western compared with Asian populations (Dogan et al, 2012; Dearden et al, 2013). Although many agents have been developed to target this element of the RAS-ERK pathway, clinical efficacy data have been mixed (Kempf et al, 2016). Direct inhibition of RAS activation using salirasib failed to show clinical efficacy in patients with stage IIIB/IV lung adenocarcinoma KRAS mutations (Riely et al, 2011). In patients with NSCLC who were treated with the multitarget tyrosine sorafenib in the third or fourth-line setting, post-hoc analyses found that KRAS mutation status was not predictive of efficacy (Mok et al, 2012).
The Phase I NCIC study has been expanded into a Phase II trial investigating selumetinib in patients receiving pemetrexed and platinum-based chemotherapy in advanced or metastatic non-squamous NSCLC without a detected KRAS mutation or with an unknown KRAS mutation status (NCT02337530). Selumetinib has also been explored in combination with docetaxel as a second-line treatment in patients with KRASm advanced NSCLC in the SELECT-1 trial. However, no difference in PFS (primary endpoint), overall survival, or objective response rate was observed (Jänne et al, 2016c). Owing to the large number of co-mutations in patients with KRASm NSCLC, the specific patient subgroup that may derive benefit from selumetinib remains to be determined. Consequently, no further clinical trials are currently planned with selumetinib in this setting. Exploratory analyses from the SELECT-1 trial demonstrated that there was no evidence that treatment effect on PFS differed by specific KRAS mutation status (determined by next-generation sequencing) (Jänne et al, 2016a). Similarly, PD-L1 status did not significantly impact PFS, overall survival, or objective response rate in either the selumetinib plus docetaxel or docetaxel alone treatment groups (Jänne et al, 2016a). However, selumetinib monotherapy has demonstrated clinical benefit in patients with neurofibromatosis type 1 (Dombi et al, 2016), which may warrant investigation of the utility of selumetinib for neurofibromatosis type 1 mutant NSCLC tumours (Redig et al, 2016).
In conclusion, our study demonstrates that selumetinib can be combined with standard doses of pemetrexed plus carboplatin or cisplatin in the first-line setting with an AE profile consistent with the individual agents.
References
Banerji U, Camidge DR, Verheul HM, Agarwal R, Sarker D, Kaye SB, Desar IM, Timmer-Bonte JN, Eckhardt SG, Lewis KD, Brown KH, Cantarini MV, Morris C, George SM, Smith PD, van Herpen CM (2010) The first-in-human study of the hydrogen sulfate (Hyd-sulfate) capsule of the MEK1/2 inhibitor AZD6244 (ARRY-142886): a phase I open-label multicenter trial in patients with advanced cancer. Clin Cancer Res 16: 1613–1623.
Besse B, Johnson M, Janne PA, Garassino M, Eberhardt WEE, Besse B, Johnson M, Janne PA, Garassino M, Eberhardt WEE, Peters S, Toh CK, Kurata T, Li Z, Kowanetz M, Mocci S, Sandler A, Rizvi NA (2015) 16LBA Phase II, single-arm trial (BIRCH) of atezolizumab as first-line or subsequent therapy for locally advanced or metastatic PD-L1-selected non-small cell lung cancer (NSCLC). Eur J Cancer 51: S717–S718.
Bridgewater J, Lopes A, Beare S, Duggan M, Lee D, Ricamara M, McEntee D, Sukumaran A, Wasan H, Valle JW (2016) A phase 1b study of selumetinib in combination with cisplatin and gemcitabine in advanced or metastatic biliary tract cancer: the ABC-04 study. BMC Cancer 16: 153.
D'Addario G, Fruh M, Reck M, Baumann P, Klepetko W, Felip E (2010) Metastatic non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21 (Suppl 5): v116–v119.
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, Davis N, Dicks E, Ewing R, Floyd Y, Gray K, Hall S, Hawes R, Hughes J, Kosmidou V, Menzies A, Mould C, Parker A, Stevens C, Watt S, Hooper S, Wilson R, Jayatilake H, Gusterson BA, Cooper C, Shipley J, Hargrave D, Pritchard-Jones K, Maitland N, Chenevix-Trench G, Riggins GJ, Bigner DD, Palmieri G, Cossu A, Flanagan A, Nicholson A, Ho JW, Leung SY, Yuen ST, Weber BL, Seigler HF, Darrow TL, Paterson H, Marais R, Marshall CJ, Wooster R, Stratton MR, Futreal PA (2002) Mutations of the BRAF gene in human cancer. Nature 417: 949–954.
Dearden S, Stevens J, Wu YL, Blowers D (2013) Mutation incidence and coincidence in non small-cell lung cancer: meta-analyses by ethnicity and histology (mutMap). Ann Oncol 24: 2371–2376.
Denton CL, Gustafson DL (2011) Pharmacokinetics and pharmacodynamics of AZD6244 (ARRY-142886) in tumor-bearing nude mice. Cancer Chemother Pharmacol 67: 349–360.
Dogan S, Shen R, Ang DC, Johnson ML, D'Angelo SP, Paik PK, Brzostowski EB, Riely GJ, Kris MG, Zakowski MF, Ladanyi M (2012) Molecular epidemiology of EGFR and KRAS mutations in 3026 lung adenocarcinomas: higher susceptibility of women to smoking-related KRAS-mutant cancers. Clin Cancer Res 18: 6169–6177.
Dombi E, Baldwin A, Marcus LJ, Fisher MJ, Weiss B, Kim A, Whitcomb P, Martin S, Aschbacher-Smith LE, Rizvi TA, Wu J, Ershler R, Wolters P, Therrien J, Glod J, Belasco JB, Schorry E, Brofferio A, Starosta AJ, Gillespie A, Doyle AL, Ratner N, Widemann BC (2016) Activity of selumetinib in neurofibromatosis Type 1-related plexiform neurofibromas. N Engl J Med 375: 2550–2560.
Gettinger S, Rizvi NA, Chow LQ, Borghaei H, Brahmer J, Ready N, Gerber DE, Shepherd FA, Antonia S, Goldman JW, Juergens RA, Laurie SA, Nathan FE, Shen Y, Harbison CT, Hellmann MD (2016) Nivolumab monotherapy for first-line treatment of advanced non-small-cell lung cancer. J Clin Oncol 34: 2980–2987.
Hainsworth JD, Cebotaru CL, Kanarev V, Ciuleanu TE, Damyanov D, Stella P, Ganchev H, Pover G, Morris C, Tzekova V (2010) A phase II, open-label, randomized study to assess the efficacy and safety of AZD6244 (ARRY-142886) versus pemetrexed in patients with non-small cell lung cancer who have failed one or two prior chemotherapeutic regimens. J Thorac Oncol 5: 1630–1636.
Hanna N, Shepherd FA, Fossella FV, Pereira JR, de MF, von PJ, Gatzemeier U, Tsao TC, Pless M, Muller T, Lim HL, Desch C, Szondy K, Gervais R, Shaharyar Manegold C, Paul S, Paoletti P, Einhorn L, Bunn PA Jr (2004) Randomized phase III trial of pemetrexed versus docetaxel in patients with non-small-cell lung cancer previously treated with chemotherapy. J Clin Oncol 22: 1589–1597.
Jänne P, Van den Heuvel M, Barlesi F, Cobo M, Mazieres J, Crinò L, Orlov S, Blackhall F, Wolf J, Garrido P, Mariani G, Poltoratskiy A, Ghiorghiu D, McKeown A, Kilgour E, Angell H, Smith P, Kohlmann A, Lawrence D, Bowen K, Vansteenkiste J (2016a) Impact of PD-L1 status on clinical response in SELECT-1: selumetinib+docetaxel in KRASm advanced NSCLC. J Thorac Oncol 12: S952–S953.
Jänne PA, Mann H, Ghiorghiu D (2016b) Study design and rationale for a randomized, placebo-controlled, double-blind study to assess the efficacy and safety of selumetinib in combination with docetaxel as second-line treatment in patients with KRAS-mutant advanced non-small cell lung cancer (SELECT-1). Clin Lung Cancer 17: e1–e4.
Jänne PA, Shaw AT, Pereira JR, Jeannin G, Vansteenkiste J, Barrios C, Franke FA, Grinsted L, Zazulina V, Smith P, Smith I, Crino L (2013) Selumetinib plus docetaxel for KRAS-mutant advanced non-small-cell lung cancer: a randomised, multicentre, placebo-controlled, phase 2 study. Lancet Oncol 14: 38–47.
Jänne PA, van den Heuvel M, Barlesi F, Cobo M, Mazieres J, Crinò L, Orlov S, Blackhall F, Wolf J, Garrido P, Poltoratskiy A, Mariani G, Ghiorghiu D, Kilgour E, Smith P, Kohlmann A, Carlile D, Lawrence D, Bowen K, Vansteenkiste JF (2016c) Selumetinib in combination with docetaxel as second-line treatment for patients with KRAS-mutant advanced NSCLC: Results from the phase III SELECT-1 trial. Ann Oncol 27 (Suppl 6): vi552–vi587.
Karampeazis A, Vamvakas L, Kentepozidis N, Polyzos A, Chandrinos V, Rigas G, Christofyllakis C, Kotsakis A, Hatzidaki D, Pallis AG, Georgoulias V (2016) Biweekly carboplatin plus gemcitabine as first-line treatment of elderly patients with advanced squamous non-small-cell lung cancer: a multicenter phase I-II trial by the Hellenic Oncology Research Group. Clin Lung Cancer 17: 543–549.
Kempf E, Rousseau B, Besse B, Paz-Ares L (2016) KRAS oncogene in lung cancer: focus on molecularly driven clinical trials. Eur respir rev 25: 71–76.
Kirkwood JM, Bastholt L, Robert C, Sosman J, Larkin J, Hersey P, Middleton M, Cantarini M, Zazulina V, Kemsley K, Dummer R (2012) Phase II, open-label, randomized trial of the MEK1/2 inhibitor selumetinib as monotherapy versus temozolomide in patients with advanced melanoma. Clin Cancer Res 18: 555–567.
Langer CJ, Gadgeel SM, Borghaei H, Papadimitrakopoulou VA, Patnaik A, Powell SF, Gentzler RD, Martins RG, Stevenson JP, Jalal SI, Panwalkar A, Yang JC, Gubens M, Sequist LV, Awad MM, Fiore J, Ge Y, Raftopoulos H, Gandhi L (2016) Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol 17: 1497–1508.
Minor DR, Puzanov I, Callahan MK, Hug BA, Hoos A (2015) Severe gastrointestinal toxicity with administration of trametinib in combination with dabrafenib and ipilimumab. Pigment Cell Melanoma Res 28: 611–612.
Mok T, Paz-Ares L, Wu Y-L, Novello S, Juhasz E, Aren O, Sun Y, Hirsh V, Smit Ef, Lathia C, Ong TJ, Pena C (2012) Association between Tumor EGFR and KRAS mutation status and clinical outcomes in NSCLC patients randomized to sorafenib plus best supportive care (BSC) or BSC alone: subanalysis of the phase III MISSION trial. Ann Oncol 23 (Suppl 9): ixe 1–ixe 30.
Nicholas GA, Goffin JR, Laurie SA, Robinson AG, Goss GD, Reaume MN, Mates M, Wheatley-Price P, Ellis PM, Juergens RA, Tomiak AT, Gregg RW, Melosky BL, Tu D, Ritter H, Seymour L, Bradbury PA (2015) A phase Ib study of selumetinib in patients (pts) with previously untreated metastatic non-small cell lung cancer (NSCLC) receiving standard chemotherapy: NCIC Clinical Trials Group IND 215 NCT01783197. J Clin Oncol 33 (Suppl 15): abstr 8046.
Novello S, Barlesi F, Califano R, Cufer T, Ekman S, Levra MG, Kerr K, Popat S, Reck M, Senan S, Simo GV, Vansteenkiste J, Peters S (2016) Metastatic non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 27: v1–v27.
Park CK, Oh IJ, Kim KS, Choi YD, Jang TW, Kim YS, Lee KH, Shin KC, Jung CY, Yang SH, Ryu JS, Jang SH, Yoo SS, Yong SJ, Lee KY, In KH, Lee MK, Kim YC (2017a) Randomized phase III study of docetaxel plus cisplatin versus pemetrexed plus cisplatin as first-line treatment of nonsquamous non-small-cell lung cancer: a TRAIL trial. Clin Lung Cancer 18: e289–e296.
Park K, Cho EK, Bello M, Ahn MJ, Thongprasert S, Song EK, Soldatenkova V, Depenbrock H, Puri T, Orlando M (2017b) Efficacy and safety of first-line necitumumab plus gemcitabine and cisplatin versus gemcitabine and cisplatin in east Asian patients with stage IV squamous non-small cell lung cancer: a subgroup analysis of the phase 3, open-label, randomized SQUIRE study. Cancer Res Treat; e-pub ahead of print 6 January 2017; doi:10.4143/crt.2016.423.
Qin A, Coffey DG, Warren EH, Ramnath N (2016) Mechanisms of immune evasion and current status of checkpoint inhibitors in non-small cell lung cancer. Cancer Med 5: 2567–2578.
Reck M, Popat S, Reinmuth N, De RD, Kerr KM, Peters S (2014) Metastatic non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25 (Suppl 3): iii27–iii39.
Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, Gottfried M, Peled N, Tafreshi A, Cuffe S, O'Brien M, Rao S, Hotta K, Leiby MA, Lubiniecki GM, Shentu Y, Rangwala R, Brahmer JR (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375: 1823–1833.
Redig AJ, Capelletti M, Dahlberg SE, Sholl LM, Mach S, Fontes C, Shi Y, Chalasani P, Janne PA (2016) Clinical and molecular characteristics of NF1-mutant lung cancer. Clin Cancer Res 22: 3148–3156.
Riely GJ, Johnson ML, Medina C, Rizvi NA, Miller VA, Kris MG, Pietanza MC, Azzoli CG, Krug LM, Pao W, Ginsberg MS (2011) A phase II trial of Salirasib in patients with lung adenocarcinomas with KRAS mutations. J Thorac Oncol 6: 1435–1437.
Rizvi NA, Hellmann MD, Brahmer JR, Juergens RA, Borghaei H, Gettinger S, Chow LQ, Gerber DE, Laurie SA, Goldman JW, Shepherd FA, Chen AC, Shen Y, Nathan FE, Harbison CT, Antonia S (2016) Nivolumab in combination with platinum-based doublet chemotherapy for first-line treatment of advanced non-small-cell lung cancer. J Clin Oncol 34: 2969–2979.
Roberts PJ, Stinchcombe TE (2013) KRAS mutation: should we test for it, and does it matter? J Clin Oncol 31: 1112–1121.
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, Lilenbaum R, Johnson DH (2006) Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 355: 2542–2550.
Scagliotti GV, Parikh P, von PJ, Biesma B, Vansteenkiste J, Manegold C, Serwatowski P, Gatzemeier U, Digumarti R, Zukin M, Lee JS, Mellemgaard A, Park K, Patil S, Rolski J, Goksel T, de MF, Simms L, Sugarman KP, Gandara D (2008) Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol 26: 3543–3551.
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J, Zhu J, Johnson DH Eastern Cooperative Oncology Group (2002) Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 346: 92–98.
Severin P, Bailey C, Chen M, Fisher A, Holmes V (2016) Determination of selumetinib, N-desmethyl selumetinib and selumetinib amide in human biological samples by LC-MS/MS. Bioanalysis 8: 1919–1936.
Shepherd FA, Dancey J, Ramlau R, Mattson K, Gralla R, O'Rourke M, Levitan N, Gressot L, Vincent M, Burkes R, Coughlin S, Kim Y, Berille J (2000) Prospective randomized trial of docetaxel versus best supportive care in patients with non-small-cell lung cancer previously treated with platinum-based chemotherapy. J Clin Oncol 18: 2095–2103.
Shepherd FA, Domerg C, Hainaut P, Janne PA, Pignon JP, Graziano S, Douillard JY, Brambilla E, Le Chevalier T, Seymour L, Bourredjem A, Le Teuff G, Pirker R, Filipits M, Rosell R, Kratzke R, Bandarchi B, Ma X, Capelletti M, Soria JC, Tsao MS (2013) Pooled analysis of the prognostic and predictive effects of KRAS mutation status and KRAS mutation subtype in early-stage resected non-small-cell lung cancer in four trials of adjuvant chemotherapy. J Clin Oncol 31: 2173–2181.
Yeh TC, Marsh V, Bernat BA, Ballard J, Colwell H, Evans RJ, Parry J, Smith D, Brandhuber BJ, Gross S, Marlow A, Hurley B, Lyssikatos J, Lee PA, Winkler JD, Koch K, Wallace E (2007) Biological characterization of ARRY-142886 (AZD6244), a potent, highly selective mitogen-activated protein kinase kinase 1/2 inhibitor. Clin Cancer Res 13: 1576–1583.
Acknowledgements
We would like to thank Dr Rafii for his clinical contribution to the delivery of the study. The study was funded by AstraZeneca. All clinical sites received funding from Cancer Research UK and the Departments of Health as Experimental Cancer Medicine Centres. The authors would like to acknowledge Leah Evans, MNeuroSci, of iMed Comms, an Ashfield Company, part of UDG Healthcare plc for medical writing support that was funded by AstraZeneca.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AG received consultancy fees from AstraZeneca. KS, DG and AWD are employees of AstraZeneca, and DG and AWD hold stock options. FB received a grant and personal fees from, and is a Board Member for AstraZeneca. NS has received travel costs from AstraZeneca for her attendance at AstraZeneca-funded meetings. RC, RP and YS have received honorarium for advisory boards from AstraZeneca. H-TA, NMD, CRL, SH and MV have no conflicts of interest to declare.
Additional information
Supplementary Information accompanies this paper on British Journal of Cancer website
Rights and permissions
This work is licensed under the Creative Commons Attribution-Non-Commercial-Share Alike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Greystoke, A., Steele, N., Arkenau, HT. et al. SELECT-3: a phase I study of selumetinib in combination with platinum-doublet chemotherapy for advanced NSCLC in the first-line setting. Br J Cancer 117, 938–946 (2017). https://doi.org/10.1038/bjc.2017.271
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.271
Keywords
This article is cited by
-
Cutaneous toxicities of mitogen-activated protein kinase inhibitors in children and young adults with neurofibromatosis-1
Journal of Neuro-Oncology (2024)
-
Regulation of MEK inhibitor selumetinib sensitivity by AKT phosphorylation in the novel BRAF L525R mutant
International Journal of Clinical Oncology (2023)
-
Randomised, Phase II study of selumetinib, an oral inhibitor of MEK, in combination with cisplatin and gemcitabine chemotherapy for patients with advanced biliary tract cancer
British Journal of Cancer (2022)
-
Selumetinib: a selective MEK1 inhibitor for solid tumor treatment
Clinical and Experimental Medicine (2022)
-
MEK inhibitors for the treatment of non-small cell lung cancer
Journal of Hematology & Oncology (2021)