Abstract
The biguanide drug metformin profoundly affects cell metabolism, causing an impairment of the cell energy balance and triggering a plethora of pleiotropic effects that vary depending on the cellular or environmental context. Interestingly, a decade ago, it was observed that metformin-treated diabetic patients have a significantly lower cancer risk. Although a variety of in vivo and in vitro observations emphasising the role of metformin as anticancer drug have been reported, the underlying mechanisms are still poorly understood. Here, we discuss our current understanding of the molecular mechanisms that are perturbed by metformin treatment and that might be relevant to understand its antitumour activities. We focus on the cell-autonomous mechanisms modulating growth and death of cancer cells.
Similar content being viewed by others
Main
Metformin is the first-line pharmacological treatment for type 2 diabetes (T2D) as its oral administration lowers blood glucose levels and improves insulin sensitivity of diabetic patients (Kirpichnikov et al, 2002). The antihyperglycaemic effect is mediated by different systemic adaptations including inhibition of gluconeogenesis in the liver and of glucose adsorption in the intestine combined with an increase in hexose uptake by adipose tissue and skeletal muscle (Sokolovska et al, 2010; Li et al, 2011). The observation that reduced oxygen consumption by mitochondria accompanies the hypoglycaemic effect suggested that this organelle is a metformin target (Davidoff, 1971). Indeed, in a variety of systems, metformin inhibits complex I in the mitochondrial respiratory chain (El-Mir et al, 2000; Owen et al, 2000), causing a decrease of the ATP/AMP ratio (Viollet et al, 2012). This primary perturbation, causing an impairment of the cell energy balance, triggers a plethora of pleiotropic effects that vary depending on the cellular or environmental context. The complexity of the organismal response to metformin is pictured in the four-word clouds in Figure 1 representing the co-occurrence in PubMed abstracts of the string ‘metformin’ with different terms referring to biological processes, gene names, cell types and diseases. This analysis clearly highlights the role of metformin as caloric restriction mimetics, being associated with biological processes such as glycolysis, autophagy, insulin resistance as well as with master regulators of nutrient response, such as LKB1, mTOR and AMPK1/2 (Figure 1). In agreement with its role as a caloric restriction mimetics, metformin improves lifespan in nematodes, fruit flies and mice (Anisimov, 2013). Consistently with its antiageing effect, metformin treatment promotes neurogenesis and enhances spatial memory formation by activating an atypical PKC-CBP pathway (Wang et al, 2012). In skeletal muscle, metformin attenuates damage by counteracting calcium influx triggered by cardiotoxin (Langone et al, 2014). The clinical applications of metformin have been extended from treatment of T2D to polycystic ovary syndrome, where the biguanide treatment induces a reduction of inflammatory markers (Morin-Papunen et al, 2003).
Word clouds of metformin-related terms. We first extracted all PubMed publications having ‘cancer’ and ‘metformin’ in their titles or abstracts. We next used a text mining approach to count the occurrences of gene mentions in these abstracts (A). Genes were identified by searching gene names and their synonyms, as annotated in UniProtKB. We kept only relevant terms according to a P-value calculated using as a background set of randomly selected publications. The same analysis was done for (B) processes, (C) diseases and (D) cells and tissues using MeSH (Medical Subject Headings) terms from the NLM (National Library of Medicine)-controlled vocabulary thesaurus. The size of each word is proportional to the frequency of their occurrence in the selected abstracts.
Metformin as an antitumour drug
In 2005, it was reported that metformin-treated diabetic patients have a significantly lower cancer risk (Evans et al, 2005). These initial observations prompted many clinical trials in recent years. The results of most of them supported the evidence that metformin decreases the risk to develop a variety of tumours. However, some studies reached conflicting conclusions. Overall, a variety of in vivo and in vitro observations place an emphasis on metformin treatment as a promising therapeutic strategy for cancer prevention and therapy (Sui et al, 2015). Metformin treatment exerts its anticancer role by triggering different processes: it decreases the amount of the Ki67 proliferation marker in biopsy samples of nondiabetic women with breast cancer (DeCensi et al, 2014); it suppresses metastasis formation by preferentially killing stem cells of different cancer types (Hirsch et al, 2009; Vazquez-Martin et al, 2011; Mohammed et al, 2013). The potential of the clinical use of metformin for cancer prevention and treatment have been discussed in recent reviews (Kourelis and Siegel, 2012; Pernicova and Korbonits, 2014; Morales and Morris, 2015). Here, we consider our current understanding of the molecular mechanisms underlying the anticancer activity of metformin, focussing on the cell-autonomous mechanisms modulating growth and death of cancer cells.
Systemic effects of metformin on cancer progression
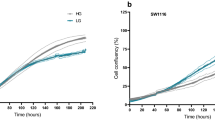
Hyperinsulinaemia and hyperglycaemia have been associated with tumourigenesis risk and poor prognosis in several cancers (Anandakumar et al, 2009; Algire et al, 2010; Nakamura et al, 2012). However, it is not clear whether reduced levels of glucose and insulin are sufficient to explain the antineoplastic effect of metformin. For instance, Eikawa et al (2015) proposed that the chemotherapeutic property of metformin stands on its ability to boost the immune system against neoplastic proliferation. Aside from the direct effect on tumourigenesis, glucose levels also affect tumour cell sensitivity to metformin treatment (Menendez et al, 2012; Wahdan-Alaswad et al, 2013; Zordoky et al, 2014). Cells grown in low glucose rely on increased mitochondrial metabolism and are therefore more sensitive to metformin inhibition of mitochondrial metabolism (Andrzejewski et al, 2014). In addition, apoptosis induced by metformin in triple-negative and ER-high or HER-high breast cancer cell lines depends on AMPK but is suppressed by high concentration of glucose (25 mM) and amino acids (Silvestri et al, 2015). These observations stress the importance of cell environmental and metabolic context on response to metformin treatment. However, our understanding of the systemic anticancer effects of metformin remains limited.
Cell-autonomous mechanisms mediating the anticancer properties of metformin
Many cell-autonomous activities of metformin have been reported. Although this does not lead to a satisfactory integrated picture, here we will schematically summarise our current understanding of the molecular pathways that are modulated by metformin treatment (Figure 2).
Schematic representation of the pathways affected by metformin treatment. The proteins mentioned in this review were linked in a graph representation by using causal relationships extracted from the SIGNOR database (Perfetto et al, 2015). Red hammerheads and blue arrows represent activation and inactivation relationships, respectively. Proteins that are activated or inactivated by metformin are coloured in green and red, respectively.
Activation of AMPK pathway
The Ser/Thr kinase AMPK senses the unbalance in the AMP/ATP ratio and activates and modifies a well-described downstream pathway that modulates cellular metabolism and energy homeostasis. Pertinent to the anticancer role of metformin is the observation that AMPK exerts an antitumourigenic role in cancer, activating two well-known tumour suppressors, TSC2 and p53 (Faubert et al, 2015). Consistently, loss of AMPK activity has been observed in different cancer types. Different molecular mechanisms mediating the metformin-dependent AMPK activation have been described. The first mechanism relies on the ability to act on isolated mitochondria and decrease complex I-dependent respiration and ATP production (Andrzejewski et al, 2014). AMPK senses the AMP/ATP ratio and, as a consequence, it is activated by the decrease of ATP levels following the inhibition of mitochondrial complex 1. On the same line, we recently showed that metformin also inhibits the mitochondrial respiratory complex by decreasing the protein level of complex 1 (NADH-ubiquinone oxidoreductase) subunits as well as five components of complex 3 (cytochrome bc1 complex; Sacco et al, 2016). As a second mechanism, it was proposed that metformin activates AMPK by triggering the activation of the ATM–LKB1–AMPK axis (GoDarts et al, 2011). In a genome-wide association study, the authors show that inhibition of ATM in a rat cancer cell line weakens metformin-mediated activation of the metabolic enzyme AMPK.
Interestingly, after metformin treatment, the phosphoproteome profile of breast cancer cells was significantly enriched for the substrate motif of ATM, supporting the involvement of the activation of this kinase in the cell response to metformin (Sacco et al, 2016). In addition to these two mechanisms, we recently showed that metformin significantly increases the concentration of the regulatory subunit β of AMPK (PRKAB1), whose interaction with the catalytic subunit triggers the enzyme kinase activity. This last observation suggests that full activation of AMPK requires de novo transcription and translation that is consistent with the fact that metformin requires a long-term treatment for complete AMPK activation.
Besides the AMPK-dependent regulation of proteins involved in lipid and glucose metabolism (ACACA and GFPT1), the metformin-mediated activation of AMPK results in the downmodulation of cell proliferation-related proteins, such as RAF1 and TBC1D1 (Sacco et al, 2016).
Inhibition of AKT–mTORC1 pathway
The impairment of target of rapamycin (mTOR) signalling pathway is one of the hallmarks of metformin treatment. The mTOR plays a key role in regulation of cell growth and metabolism, and thus the correlation between the activation of mTOR and tumour progression is not surprising. The activation of the mTOR pathway is involved in the regulation of many cancer hallmarks, including tumour growth, angiogenesis and metastasis (Hanahan and Weinberg, 2011). The mTORC1 activation is limited by metformin in several ways: by increasing the mTOR inhibitor REDD1 (regulated in development and DNA damage responses) (1); it inhibits the Ragulator complex that positively regulates mTOR (2) and it mimics amino acid depletion causing loss of colocalisation between mTOR and its activator Rheb (3) (Kalender et al, 2010; Pierotti et al, 2013). The metformin-mediated mTORC1 complex inhibition exerts a strong impact on key physiological processes, such as autophagy, protein synthesis and cell proliferation.
A deep MS-based phosphoproteomics approach revealed that metformin does not induce a mere inhibition of the whole AKT–mTOR axis, but rather rewires the whole pathway. Analysing the AKT–mTORC1 pathway in breast cancer cells MCF7 treated with metformin, we found that metformin decreases phosphorylation of two mTOR substrates, p70S6K and rpS6 but, contrary to expectation, this is not mediated by a diminished mTOR activity. We find that, in these conditions, the activity of the upstream inducer of mTORC1 complex, the AKT kinase, is increased by metformin. As a consequence, the mTOR inhibitor TSC2 is phosphorylated and therefore inhibited. There are two main logical disconnections in this pathway when perturbed by metformin: the mTOR repressor, TSC2, is inhibited but mTOR remains steadily activated, whereas its downstream effector S6K is inhibited. On the same line, in MCF7 cells treated with metformin, addition of insulin-like growth factor (IGF) triggers IGF1R and AKT phosphorylation, whereas p70S6K substrates (rpS6, IRS1) are not activated, remaining in a constitutive inactive form. We propose that IGF stimulation fails to activate p70S6K because metformin triggers the assembly and activation of the PP2A phosphatase by increasing phosphorylation of the PPP2R5C regulatory subunit (Sacco et al, 2016).
Inhibition of cell cycle progression
Cell cycle progression is often altered in cancer cells, leading to an aberrant regulation of cell division and DNA replication. Many reports demonstrated that the anticancer property of metformin is a consequence of cell cycle perturbation. Specifically, exposure to metformin induced cell cycle arrest in G0/G1 and G2/M phases in different cancer types, including breast cancer cells and oesophageal squamous cancer cells. The molecular mechanisms underlying the metformin-induced cell cycle arrest have been extensively described and involve the upregulation of cyclin-dependent kinase inhibitors (CDKIs), such as p21 or p27 proteins. Although in breast cancer cells (ER positive and negative, erbB2-overexpressing and erbB2-normal) metformin treatment does not affect the expression levels of p21 e p27 CDKIs (Alimova et al, 2009), other authors also report a cyclin D1 reduction with a concomitant increase of p53, p21, Bax and cyclin E expression in metformin-treated MCF7 (Malki and Youssef, 2011). On the same line, in a metformin-treated oesophageal squamous cells carcinoma xenograft model, the authors observed the upregulation of p53, p21 and p27 and the downregulation of cyclin D1 (Cai et al, 2015).
Metformin treatment also affects the activity of cyclin-dependent kinases, such as CDK1 in MCF7 cells as well as CDK2, CDK4 and CDK6 in head and neck squamous cell carcinoma (Sikka et al, 2012; Sacco et al, 2016).
MAPK regulation
The mitogen-activated protein kinases (MAPKs), including the ERK1/2, p38 and JNK kinase branches, control fundamental biological processes, including proliferation, differentiation, survival and death. Although there is a general consensus about the metformin-dependent inhibition of ERK1/2 kinases in different cancer types (Memmott et al, 2010; Gou et al, 2013; Sacco et al, 2016), contrasting evidences have been reported about the modulation of p38 and JNK pathways. This incongruity can be explained by the pro-apoptotic or pro-proliferative roles that these stress-activated kinases may play depending on the cellular context. In lung cancer cells, metformin treatment decreases the activity of JNK and p38 that, on the contrary, is hyperactivated in metformin-treated MCF7 cells (Tseng et al, 2013; Queiroz et al, 2014; Sacco et al, 2016). The molecular mechanisms underlying the metformin-mediated modulation of the MAPK cascades are still poorly understood. We suggest that metformin modulates these pathways by acting on the protein level of the upstream regulatory kinases and phosphatases. Metformin increases the concentration of the tyrosine phosphatase PTPRJ, a negative regulator of ERK1/2 (Sacco et al, 2009, 2012) and concomitantly it decreases the expression level of the upstream kinase ARAF. On the same line, after metformin treatment, the mRNA and protein levels of the MAP3K3 and MAP3K7 kinases are upregulated, resulting in increased phosphorylation of both p38 and the JNK substrate, JunD. Our hypothesis is that metformin puts MCF7 breast cancer cells in a pro-apoptotic state triggering a sustained activation of JNK and p38. If MCF7 cells are treated with metformin they become more sensitive to apoptotic stimuli such as the ones given by staurosporin or other chemotherapeutic drugs (Sacco et al, 2016).
SP1 transcription factor regulation
Metformin treatment induces a radical remodelling of the transcriptome and proteome, and it is not surprising to observe modulation of the activity of different transcription factors. Recent evidences demonstrated that metformin inhibits the SP transcription factor family members in vivo and in different cancer cell lines, such as pancreatic tumour cells or breast cancer cells (Sacco et al, 2016).
Safe and colleagues (Nair et al, 2013) demonstrated that in pancreatic cancer L3.6pL and Panc28 cells, metformin induced proteasome-dependent degradation of Sp1, Sp3 and Sp4 transcription factors, resulting in the downregulation of several pro-oncogenic Sp-regulated genes including bcl-2, survivin, cyclin D1, vascular endothelial growth factor with its receptor and fatty acid synthase. Interestingly, the molecular mechanism through which metformin inhibits Sp transcription factors is context dependent. The authors reported that in a different pancreatic cancer cells, Panc, metformin decreased microRNA-27a and induced the Sp repressor, ZBTB10 (Nair et al, 2013).
The analysis of metformin-induced transcriptome and proteome profiles in breast cancer cells enabled us to identify the SP1 transcription factor as the most significantly modulated, as it is equally depleted at both transcriptome and proteome levels. Our data, combined with the metformin-dependent phosphoproteome profile, are consistent with a model where metformin induces the SP1 degradation by increasing the phosphorylation of Ser51 that destabilises the transcription factor. We inferred that p38 kinase is responsible of the metformin-mediated SP1 phosphorylation. The decrease in the levels of SP1 is mirrored by a significant reduction of many SP1-controlled cancer and metabolic pathways. The expression of Von Hippel Lindau protein (VHL) is also diminished by metformin. The VHL is SP1 controlled and, besides its role as an E3 ligase of HIF-α in normoxia, it can repress the promoter activity of IGF1R by sequestering SP1 (Yuen et al, 2007). The SP1 also controls the expression of pyruvate kinase that is overexpressed in many tumours. We observe a downregulation of the oncogenic isoform pyruvate kinase M2 in MCF7 and SKBR3 breast cancer cells treated with metformin when grown in normoglycaemic condition. On the contrary, if glucose is increased fourfold, metformin does not affect the expression levels of PKM2 (Silvestri et al, 2015).
The unfolded protein response (UPR)
The UPR is triggered by a pathological increase of unfolded or misfolded proteins that is sensed by three receptors on the ER membrane. When these sensors dissociate from the ER chaperon GRP78, they activate signal transductions to stop protein synthesis, to increase proteasomal degradation and, ultimately, undergo apoptosis by overexpressing CHOP. Metformin was found to cause an AMPK-dependent downregulation of GRP78 while increasing the levels of unfolded proteins in the ER lumen. As a consequence, the cell becomes unable to adequately respond to ER stress and dies (Saito et al, 2009).
In prostate cancer cells, metformin also induces CHOP-dependent apoptosis by regulating the expression of numerous miRNAs. Among them, the tumour suppressor miR-708-5p is strongly upregulated. This miR collaborates in increasing the ER stress by suppressing the ER membrane protein neuronatin, NNAT, that controls calcium homeostasis (Yang et al, 2015). It is noteworthy that in cardiomyocytes, metformin activates the UPR but, in spite of a strong upregulation of the pro-apoptotic CHOP protein, cells are not driven to death (Quentin et al, 2012), stressing once more that metformin modulates cell death and survival in a cell-specific manner.
Conclusions
The observation that metformin reduces cancer risk in diabetic patients has raised considerable interest and has stimulated a variety of studies. Despite the wealth of information, we are still far from a clear consistent picture that could support rational strategies for cancer prevention and treatment. Metformin has a profound impact on the organism energy balance and metabolism, and the cells in the different organs, by sensing these signals, respond differently, depending on the molecular and cellular context. Tumour cell growth is affected by both changes in the environmental cues and a direct action of metformin on the molecular pathways that regulate cell growth and death. Here we have discussed the cell-autonomous mechanisms that are affected by metformin treatment combining the results of a high-content genome-wide study on a breast cancer cell line with more focussed reports on different tumour systems. After metformin treatment, the transcriptome and proteome of MCF7 breast cancer cells are remodelled and the signalling pathways are rewired. Transcription, translation and post-translational modifications are profoundly affected. The resulting picture is revealing and complex at the same time and partly explains why metformin has such pleiotropic effects depending on context (Figure 2). These studies have opened the path to a systems understanding of the molecular mechanisms underlying metformin effects, but at the same time call for more such studies in different systems and in different conditions. Only such a genome-wide understanding of the subtle differences in the response of different systems in different conditions will eventually offer a rational basis for designing new strategies to potentiate the action of metformin by combining it with different antitumour treatments.
References
Algire C, Amrein L, Zakikhani M, Panasci L, Pollak M (2010) Metformin blocks the stimulative effect of a high-energy diet on colon carcinoma growth in vivo and is associated with reduced expression of fatty acid synthase. Endocr Relat Cancer 17 (2): 351–360.
Alimova IN, Liu B, Fan Z, Edgerton SM, Dillon T, Lind SE, Thor AD (2009) Metformin inhibits breast cancer cell growth, colony formation and induces cell cycle arrest in vitro. Cell Cycle 8 (6): 909–915.
Anandakumar P, Kamaraj S, Jagan S, Ramakrishnan G, Devaki T (2009) Effect of capsaicin on glucose metabolism studied in experimental lung carcinogenesis. Nat Prod Res 23 (8): 763–774.
Andrzejewski S, Gravel SP, Pollak M, St-Pierre J (2014) Metformin directly acts on mitochondria to alter cellular bioenergetics. Cancer Metabol 2: 12.
Anisimov VN (2013) Metformin: do we finally have an anti-aging drug? Cell Cycle 12 (22): 3483–3489.
Cai X, Hu X, Tan X, Cheng W, Wang Q, Chen X, Guan Y, Chen C, Jing X (2015) Metformin induced AMPK activation, G0/G1 phase cell cycle arrest and the inhibition of growth of esophageal squamous cell carcinomas in vitro and in vivo. PLoS One 10 (7): e0133349.
Davidoff F (1971) Effects of guanidine derivatives on mitochondrial function. 3. The mechanism of phenethylbiguanide accumulation and its relationship to in vitro respiratory inhibition. J Biol Chem 246 (12): 4017–4027.
DeCensi A, Puntoni M, Gandini S, Guerrieri-Gonzaga A, Johansson HA, Cazzaniga M, Pruneri G, Serrano D, Schwab M, Hofmann U, Mora S, Aristarco V, Macis D, Bassi F, Luini A, Lazzeroni M, Bonanni B, Pollak MN (2014) Differential effects of metformin on breast cancer proliferation according to markers of insulin resistance and tumor subtype in a randomized presurgical trial. Breast Cancer Res Treat 148 (1): 81–90.
Eikawa S, Nishida M, Mizukami S, Yamazaki C, Nakayama E, Udono H (2015) Immune-mediated antitumor effect by type 2 diabetes drug, metformin. Proc Natl Acad Sci USA 112 (6): 1809–1814.
El-Mir MY, Nogueira V, Fontaine E, Averet N, Rigoulet M, Leverve X (2000) Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I. J Biol Chem 275 (1): 223–228.
Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD (2005) Metformin and reduced risk of cancer in diabetic patients. BMJ 330 (7503): 1304–1305.
Faubert B, Vincent EE, Poffenberger MC, Jones RG (2015) The AMP-activated protein kinase (AMPK) and cancer: many faces of a metabolic regulator. Cancer Lett 356 (2 Pt A): 165–170.
GoDARTS and UKPDS Diabetes Pharmacogenetics Study Group, Wellcome Trust Case Control Consortium, Zhou K, Bellenguez C, Spencer CC, Bennett AJ, Coleman RL, Tavendale R, Hawley SA, Donnelly LA, Schofield C, Groves CJ, Burch L, Carr F, Strange A, Freeman C, Blackwell JM, Bramon E, Brown MA, Casas JP, Corvin A, Craddock N, Deloukas P, Dronov S, Duncanson A, Edkins S, Gray E, Hunt S, Jankowski J, Langford C, Markus HS, Mathew CG, Plomin R, Rautanen A, Sawcer SJ, Samani NJ, Trembath R, Viswanathan AC, Wood NW, investigators M, Harries LW, Hattersley AT, Doney AS, Colhoun H, Morris AD, Sutherland C, Hardie DG, Peltonen L, McCarthy MI, Holman RR, Palmer CN, Donnelly P, Pearson ER (2011) Common variants near ATM are associated with glycemic response to metformin in type 2 diabetes. Nat Genet 43 (2): 117–120.
Gou S, Cui P, Li X, Shi P, Liu T, Wang C (2013) Low concentrations of metformin selectively inhibit CD133(+) cell proliferation in pancreatic cancer and have anticancer action. PLoS One 8 (5): e63969.
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144 (5): 646–674.
Hirsch HA, Iliopoulos D, Tsichlis PN, Struhl K (2009) Metformin selectively targets cancer stem cells, and acts together with chemotherapy to block tumor growth and prolong remission. Cancer Res 69 (19): 7507–7511.
Kalender A, Selvaraj A, Kim SY, Gulati P, Brule S, Viollet B, Kemp BE, Bardeesy N, Dennis P, Schlager JJ, Marette A, Kozma SC, Thomas G (2010) Metformin, independent of AMPK, inhibits mTORC1 in a rag GTPase-dependent manner. Cell Metabol 11 (5): 390–401.
Kirpichnikov D, McFarlane SI, Sowers JR (2002) Metformin: an update. Ann Intern Med 137 (1): 25–33.
Kourelis TV, Siegel RD (2012) Metformin and cancer: new applications for an old drug. Med Oncol 29 (2): 1314–1327.
Langone F, Cannata S, Fuoco C, Lettieri Barbato D, Testa S, Nardozza AP, Ciriolo MR, Castagnoli L, Gargioli C, Cesareni G (2014) Metformin protects skeletal muscle from cardiotoxin induced degeneration. PLoS One 9 (12): e114018.
Li Y, Xu S, Mihaylova MM, Zheng B, Hou X, Jiang B, Park O, Luo Z, Lefai E, Shyy JY, Gao B, Wierzbicki M, Verbeuren TJ, Shaw RJ, Cohen RA, Zang M (2011) AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice. Cell Metab 13 (4): 376–388.
Malki A, Youssef A (2011) Antidiabetic drug metformin induces apoptosis in human MCF breast cancer via targeting ERK signaling. Oncol Res 19 (6): 275–285.
Memmott RM, Mercado JR, Maier CR, Kawabata S, Fox SD, Dennis PA (2010) Metformin prevents tobacco carcinogen—induced lung tumorigenesis. Cancer Prev Res 3 (9): 1066–1076.
Menendez JA, Oliveras-Ferraros C, Cufi S, Corominas-Faja B, Joven J, Martin-Castillo B, Vazquez-Martin A (2012) Metformin is synthetically lethal with glucose withdrawal in cancer cells. Cell cycle 11 (15): 2782–2792.
Mohammed A, Janakiram NB, Brewer M, Ritchie RL, Marya A, Lightfoot S, Steele VE, Rao CV (2013) Antidiabetic drug metformin prevents progression of pancreatic cancer by targeting in part cancer stem cells and mTOR signaling. Transl Oncol 6 (6): 649–659.
Morales DR, Morris AD (2015) Metformin in cancer treatment and prevention. Annu Rev Med 66: 17–29.
Morin-Papunen L, Rautio K, Ruokonen A, Hedberg P, Puukka M, Tapanainen JS (2003) Metformin reduces serum C-reactive protein levels in women with polycystic ovary syndrome. J Clin Endocrinol Metabol 88 (10): 4649–4654.
Nair V, Pathi S, Jutooru I, Sreevalsan S, Basha R, Abdelrahim M, Samudio I, Safe S (2013) Metformin inhibits pancreatic cancer cell and tumor growth and downregulates Sp transcription factors. Carcinogenesis 34 (12): 2870–2879.
Nakamura A, Tajima K, Zolzaya K, Sato K, Inoue R, Yoneda M, Fujita K, Nozaki Y, Kubota KC, Haga H, Kubota N, Nagashima Y, Nakajima A, Maeda S, Kadowaki T, Terauchi Y (2012) Protection from non-alcoholic steatohepatitis and liver tumourigenesis in high fat-fed insulin receptor substrate-1-knockout mice despite insulin resistance. Diabetologia 55 (12): 3382–3391.
Owen MR, Doran E, Halestrap AP (2000) Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem J 348 (Pt 3): 607–614.
Perfetto L, Briganti L, Calderone A, Perpetuini AC, Iannuccelli M, Langone F, Licata L, Marinkovic M, Mattioni A, Pavlidou T, Peluso D, Petrilli LL, Pirro S, Posca D, Santonico E, Silvestri A, Spada F, Castagnoli L, Cesareni G (2015) SIGNOR: a database of causal relationships between biological entities. Nucleic Acids Res 44: D548–D554.
Pernicova I, Korbonits M (2014) Metformin—mode of action and clinical implications for diabetes and cancer. Nat Rev Endocrinol 10 (3): 143–156.
Pierotti MA, Berrino F, Gariboldi M, Melani C, Mogavero A, Negri T, Pasanisi P, Pilotti S (2013) Targeting metabolism for cancer treatment and prevention: metformin, an old drug with multi-faceted effects. Oncogene 32 (12): 1475–1487.
Queiroz EA, Puukila S, Eichler R, Sampaio SC, Forsyth HL, Lees SJ, Barbosa AM, Dekker RF, Fortes ZB, Khaper N (2014) Metformin induces apoptosis and cell cycle arrest mediated by oxidative stress, AMPK and FOXO3a in MCF-7 breast cancer cells. PLoS One 9 (5): e98207.
Quentin T, Steinmetz M, Poppe A, Thoms S (2012) Metformin differentially activates ER stress signaling pathways without inducing apoptosis. Dis Model Mech 5 (2): 259–269.
Sacco F, Gherardini PF, Paoluzi S, Saez-Rodriguez J, Helmer-Citterich M, Ragnini-Wilson A, Castagnoli L, Cesareni G (2012) Mapping the human phosphatome on growth pathways. Mol Syst Biol 8: 603.
Sacco F, Silvestri A, Posca D, Pirrò S, Gherardini P, Castagnoli L, Mann M, Cesareni G (2016) Deep proteomics of breast cancer cells reveals that metformin rewires signaling networks away from a pro-growth state. Cell Syst 3: 2–13.
Sacco F, Tinti M, Palma A, Ferrari E, Nardozza AP, Hooft van Huijsduijnen R, Takahashi T, Castagnoli L, Cesareni G (2009) Tumor suppressor density-enhanced phosphatase-1 (DEP-1) inhibits the RAS pathway by direct dephosphorylation of ERK1/2 kinases. J Biol Chem 284 (33): 22048–22058.
Saito S, Furuno A, Sakurai J, Sakamoto A, Park HR, Shin-Ya K, Tsuruo T, Tomida A (2009) Chemical genomics identifies the unfolded protein response as a target for selective cancer cell killing during glucose deprivation. Cancer Res 69 (10): 4225–4234.
Sikka A, Kaur M, Agarwal C, Deep G, Agarwal R (2012) Metformin suppresses growth of human head and neck squamous cell carcinoma via global inhibition of protein translation. Cell Cycle 11 (7): 1374–1382.
Silvestri A, Palumbo F, Rasi I, Posca D, Pavlidou T, Paoluzi S, Castagnoli L, Cesareni G (2015) Metformin induces apoptosis and downregulates pyruvate kinase M2 in breast cancer cells only when grown in nutrient-poor conditions. PLoS One 10 (8): e0136250.
Sokolovska J, Isajevs S, Sugoka O, Sharipova J, Lauberte L, Svirina D, Rostoka E, Sjakste T, Kalvinsh I, Sjakste N (2010) Influence of metformin on GLUT1 gene and protein expression in rat streptozotocin diabetes mellitus model. Arch Physiol Biochem 116 (3): 137–145.
Sui X, Xu Y, Wang X, Han W, Pan H, Xiao M (2015) Metformin: a novel but controversial drug in cancer prevention and treatment. Mol Pharm 12 (11): 3783–3791.
Tseng SC, Huang YC, Chen HJ, Chiu HC, Huang YJ, Wo TY, Weng SH, Lin YW (2013) Metformin-mediated downregulation of p38 mitogen-activated protein kinase-dependent excision repair cross-complementing 1 decreases DNA repair capacity and sensitizes human lung cancer cells to paclitaxel. Biochem Pharmacol 85 (4): 583–594.
Vazquez-Martin A, Oliveras-Ferraros C, Cufi S, Del Barco S, Martin-Castillo B, Lopez-Bonet E, Menendez JA (2011) The anti-diabetic drug metformin suppresses the metastasis-associated protein CD24 in MDA-MB-468 triple-negative breast cancer cells. Oncol Rep 25 (1): 135–140.
Viollet B, Guigas B, Sanz Garcia N, Leclerc J, Foretz M, Andreelli F (2012) Cellular and molecular mechanisms of metformin: an overview. Clin Sci 122 (6): 253–270.
Wahdan-Alaswad R, Fan Z, Edgerton SM, Liu B, Deng XS, Arnadottir SS, Richer JK, Anderson SM, Thor AD (2013) Glucose promotes breast cancer aggression and reduces metformin efficacy. Cell Cycle 12 (24): 3759–3769.
Wang J, Gallagher D, DeVito LM, Cancino GI, Tsui D, He L, Keller GM, Frankland PW, Kaplan DR, Miller FD (2012) Metformin activates an atypical PKC-CBP pathway to promote neurogenesis and enhance spatial memory formation. Cell Stem Cell 11 (1): 23–35.
Yang J, Wei J, Wu Y, Wang Z, Guo Y, Lee P, Li X (2015) Metformin induces ER stress-dependent apoptosis through miR-708-5p/NNAT pathway in prostate cancer. Oncogenesis 4: e158.
Yuen JS, Cockman ME, Sullivan M, Protheroe A, Turner GD, Roberts IS, Pugh CW, Werner H, Macaulay VM (2007) The VHL tumor suppressor inhibits expression of the IGF1R and its loss induces IGF1R upregulation in human clear cell renal carcinoma. Oncogene 26 (45): 6499–6508.
Zordoky BN, Bark D, Soltys CL, Sung MM, Dyck JR (2014) The anti-proliferative effect of metformin in triple-negative MDA-MB-231 breast cancer cells is highly dependent on glucose concentration: implications for cancer therapy and prevention. Biochim Biophys Acta 1840 (6): 1943–1957.
Acknowledgements
This work was supported by the DEPTH project of the European Research Council (Grant Agreement 322749) by the Italian Association for Cancer Research Grant (N.14135) to GC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-Non-Commercial-Share Alike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Sacco, F., Calderone, A., Castagnoli, L. et al. The cell-autonomous mechanisms underlying the activity of metformin as an anticancer drug. Br J Cancer 115, 1451–1456 (2016). https://doi.org/10.1038/bjc.2016.385
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.385
Keywords
This article is cited by
-
A multi-centered trial investigating gestational treatment with ursodeoxycholic acid compared to metformin to reduce effects of diabetes mellitus (GUARD): a randomized controlled trial protocol
Trials (2022)
-
Metformin exerts anti-AR-negative prostate cancer activity via AMPK/autophagy signaling pathway
Cancer Cell International (2021)
-
Pharmacological Management of Gestational Diabetes Mellitus
Drugs (2017)