Abstract
Background:
The purpose of this study was to develop a nomogram to predict ‘poor prognosis recurrence’ (PPR) in women treated for endometrial cancer (EC).
Methods:
The data of 861 women who received primary surgical treatment between January 2001 and December 2013 were abstracted from a prospective multicenter database. Data were randomly split into two sets: training and validation with a predefined 2/3 ratio. A Cox proportional hazards multivariate model of selected prognostic features was performed in the training cohort (n=574) to develop a nomogram predicting PPRs. The nomogram was validated in the validation cohort of 287 patients.
Results:
In the training cohort, 82 (14.3%) developed subsequent PPR. Age, histologic type and grade, lymphovascular space invasion status, FIGO stage, and nodal staging (SLN±pelvic and/or para-aortic lymphadenectomy) were independently associated with subsequent PPR. The nomogram showed an area under the receiver operating characteristic curve (AUC) of 0.82 (95% confidence interval (CI), 0.73–0.89) in the training set. The validation set showed a good discrimination with an AUC of 0.75 (95% CI, 0.65–0.83).
Conclusions:
We have developed a robust tool that is able to predict subsequent PPRs in women with FIGO I–III EC.
Similar content being viewed by others
Main
Endometrial cancer (EC) is the most common gynaecological cancer in developed countries. It generally has a favourable prognosis, with a 5-year overall survival reaching 80% mainly because most women are diagnosed at an early stage and managed by surgery alone with a low risk of recurrence (Amant et al, 2005). Adjuvant radiotherapy and systemic treatment are options for women at increased risk of recurrence. In this specific setting, several studies have demonstrated that women’s age, histological type and grade, depth of myometrial invasion, cervical involvement, and lymphovascular space involvement (LVSI) status can predict recurrence and survival (Morrow et al, 1991). Hence, risk groups for recurrence have been described based on these clinicopathological prognostic factors to identify women with poor prognosis who may benefit from adjuvant therapy.
Although relatively few women with EC experience recurrence, it accounts for most EC-related deaths. Moreover, there are several types of recurrence with different impact on survival and for which management may be based on either surgery or systemic treatment, or a combination of both. However, the various types of recurrence in EC have not been clearly defined to date although authors agree that the development of distant metastases (i.e., brain, lung, liver, bone metastases, and supra-diaphragmatic nodal metastases) results in a significant reduction in overall survival (Creasman et al, 1987). It would be of particular interest to identify women with a ‘poor prognosis recurrence’ (PPR) for EC for whom surgical treatment is rarely an option. These women could then benefit from more individualised counselling in terms of prognosis, therapeutic options at initial management, monitoring strategies, and lifestyle modifications.
In this French retrospective multicenter study, we developed a nomogram based on selected clinical and histological variables to predict the likelihood of 3-year PPR in women with early stage EC.
Materials and Methods
Study population
From January 2001 to December 2013, the data of all women who had undergone primary surgical treatment for EC were retrospectively abstracted from prospectively maintained databases of eight institutions in France (Tours University hospital, Creteil Hospital, Reims University Hospital, Jeanne de Flandre University Hospital, Dijon Cancer Center, Rennes University Hospital, and Tenon University Hospital), and from the Senti-Endo trial (Ballester et al, 2011; Daraï et al, 2015). All the women had presumed early stage EC and final 2009 International Federation of Gynecology and Obstetrics (FIGO) (Pecorelli and Sergio, 2009) stages I–III cancer (with primary tumour confined to the corpus uteri). The medical records were reviewed to determine age, body mass index (BMI, calculated as weight in kilograms divided by the square of height in metres), surgical procedure, final pathological analysis (histologic type and grade, depth of myometrial invasion, LVSI status, and final nodal status), and adjuvant treatments. Histologic type 1 included endometrioid tumours (whatever the grade) and histologic type 2 included serous carcinomas, clear cell carcinomas, and carcinosarcomas (Colombo et al, 2016a). Lymphovascular space involvement was considered positive if lymphatic, vascular, or angiolymphatic invasion was reported. Patients were included if they had all these data available. The research protocol was approved by the institutional review board of the French College of Obstetricians and Gynecologists (CEROG 2014-GYN-020).
Treatment and follow-up
Women were included if they had undergone primary surgical treatment, including at least total hysterectomy with bilateral salpingo-oophorectomy, with or without nodal staging (sentinel lymph node (SLN)±pelvic±para-aortic lymphadenectomy). Some aspects of the management of EC changed during the study period. Before 2010, nodal staging was recommended for all women and included pelvic±para-aortic lymphadenectomy; after 2010, both pelvic and para-aortic lymphadenectomy were exclusively recommended for women with high-risk EC or metastatic pelvic lymph nodes. Since the publication of French guidelines in 2010, lymphadenectomy was no longer recommended for women with low-/intermediate- risk EC. Women with early stage EC who were enrolled in the Senti-Endo trial from July 2007 to August 2009 underwent a pelvic SLN biopsy with systematic pelvic lymphadenectomy. When the pelvic SLN was found to be metastatic at intraoperative histology or after final histology, a para-aortic lymphadenectomy was recommended. (Querleu et al, 2011; Colombo et al, 2013; Colombo et al, 2016a). The decision whether to introduce adjuvant therapy was made by a multidisciplinary oncology committee based on international guidelines; it included vaginal brachytherapy and/or external beam radiotherapy and/or chemotherapy (Querleu et al, 2011; Colombo et al, 2013; Colombo et al, 2016a). Clinical follow-up consisted of physical examination and the use of imaging techniques according to the findings and for high-risk group of recurrence.
Statistical analysis
Development of the nomogram
EC recurrence was diagnosed by biopsy or imaging studies and divided into: (i) vaginal vault recurrence; (ii) isolated locoregional lymph nodes recurrence (pelvic and/or infra-diaphragmatic para-aortic lymph nodes); (iii) local central pelvic recurrence; (iv) peritoneal carcinomatosis, and (v) distant metastases including brain, lung, liver, and bone metastases, as well as supra-diaphragmatic nodal metastases. We assumed that PPR included distant metastases and peritoneal carcinomatosis. To develop a well-calibrated and exportable nomogram for PPRs, data were randomly split into a training set and an external validation set with a predefined 2/3 ratio. This split was expected to provide balanced statistical power to identify and assess predictors (Steyerberg, 2009).
In the training cohort (2 out of 3 of the whole population), we first defined PPR by analysing 3-year overall survival according to recurrence site. Demographics and histological factors were then tested individually for association with PPR using log-rank tests. Factors with a P-value <0.1 were then included in a Cox proportional hazards model. The final model equation was then designed to calculate patient-specific probabilities of PPR. Multivariate analyses were performed by using the Cox proportional hazards model. Hazard ratios were calculated from the model coefficients. The model performance for predicting outcome was evaluated by calculating the concordance index (c-index), which is a generalisation of the area under the curve of the receiver operating characteristics (ROC) curve and can be applied to continuous outcome and censored data (Hanley and McNeil, 1982; Harrell et al, 1988; Heagerty et al, 2000). Complexity of the model was controlled using Akaike information criteria (Akaike, 1985). A P–value <0.05 was considered significant.
For external validation, the nomogram was then applied to the validation cohort (1 out of 3 of the whole population). We performed the calibration (i.e., agreement between observed outcome frequencies and predicted probabilities of subsequent PPR) using graphic representations of the relationship between the observed outcome frequencies and the predicted probabilities. The clinical significance of calibration reflected the accuracy of individual predictions of subsequent PPR. Moreover, we evaluated average and maximal errors between predictions and observations obtained from the calibration curve.
Optimal threshold of the nomogram
The optimal threshold (cutoff points) of the nomogram in terms of clinical utility, sensitivity, specificity, negative predictive values, positive predictive values, and its overall diagnostic accuracy (i.e., probability for a woman to be correctly classified by the nomogram) was evaluated by the ROC curve area and the Youden Index (Schisterman et al, 2005).
Poor prognosis recurrence-free survival estimates were based on Kaplan–Meier calculations and recurrence-free survival (RFS) defined as the time from the date of surgery to the date of PPR. The difference in RFS was assessed by a log-rank test.
Other statistical analyses
The categorical and numerical variables were analysed using the χ2-test and the Student t-test, respectively. P–values <0.05 were considered to denote significant differences. Data were managed with an Excel database (Microsoft, Redmond, WA, USA) and analysed using R 2.15 software, available online with caTools, rms, presence/absence, and verification libraries (https://www.r-project.org/).
Results
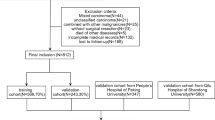
During the study period, 1207 women with presumed early stage EC were documented as having received primary surgical treatment. Women with incomplete pathological data or with a follow-up <12 months without recurrence were excluded. About 861 women were included in the analysis according to the following distribution: Tours University Hospital (n=240, 27.9%), Creteil Hospital (n=112; 13.0%), Reims University Hospital (n=101; 11.7%), Dijon Cancer Center (n=97; 11.2%), Jeanne de Flandre University hospital (n=95; 11.0%), Rennes University Hospital (n=56; 6.5%), Tenon University Hospital (n=54; 6.3%), and Senti-Endo trial (n=106; 12.3%). The demographics and clinicopathological characteristics of women in the training cohort (n=574) and the validation cohort (n=287; Figure 1) are reported in Table 1.
Analysis of overall survival from time of EC diagnosis in the training cohort according to recurrence site revealed marked differences (Figure 2). Three-year overall survival was 96.2% for women with no recurrence; 73.4% women with vaginal vault recurrence, locoregional nodal recurrence, local central pelvic recurrence; and 38.1% for women with distant metastases and peritoneal carcinomatosis. Therefore, distant metastases and peritoneal carcinomatosis were confirmed as PPR. In the training set, 137 women did not undergo lymphadenectomy: 52 high-risk EC, 17 high-intermediate-risk EC, 15 intermediate-risk EC and 53 low-risk EC. Of the 52 high-risk women, 49 were older than 75 years, 21 had severe obesity with inherent morbidities (BMI⩾40).
Prediction of the probability of PPR in women with EC
Of the 574 women in the training cohort, 82 (14.3%) experienced PPR (Table 2). Treatment characteristics of women with PPR are reported on Table 3. The median time between initial diagnosis and PPR was 9.0 months (range, 1–114 months). Table 4 summarises univariate and multivariate analyses. In the Cox proportional hazard model, the occurrence of PPR was independently associated with older age, EC histological type (2 vs 1), a higher histological grade (1 or 2 vs 3), FIGO stage, LVSI status (positive vs negative), and the performance of surgical nodal staging.
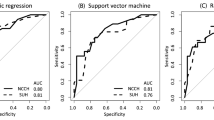
On the basis of the covariates independently associated with PPR, we constructed a nomogram and probabilities of PPR were reported at 3 years (Figure 3A). The prediction model had a concordance index of 0.82 (95% confidence interval (CI), 0.73–0.89).
Nomogram presentation. (A) Nomogram for predicting 3-year probability of poor prognosis recurrence (PPR) for women with I–III FIGO stage endometrial cancer. To estimate risk, calculate points for each variable by drawing a straight line from patient’s variable value to the axis labelled ‘Points’. Sum all points and draw a straight line from the total point axis to the 3-year recurrence axis. (B) Recurrence-free survival according to nomogram optimal threshold. (C) Graph showing how the prediction model could be used to design a clinical trial testing the efficacy of systemic chemotherapy with or without radiation in endometrial cancer.
External validation of the nomogram
The concordance index of the nomogram in the external validation model was 0.75 (95% CI, 0.65–0.83). Of note, the nomogram was well calibrated. The mean absolute error in predicted probabilities was 1.9%, and the maximum error was <0.001%.
Optimal threshold of the nomogram
According to the PPR distribution at each probability of the nomogram, two groups were identified: a low-risk PPR group (PPR probability <0.15, 73.5% of the validation cohort, and PPR rate=5.1%) and a high-risk PPR group (PPR probability ⩾0.15, 26.5% of the validation cohort, and PPR rate=29.6%). A PPR probability ⩾0.15 corresponded to the optimal threshold of the Risk Stratification System (RSS) in terms of clinical utility with an overall diagnostic accuracy of 77.6%. At this threshold, sensitivity and specificity of the nomogram were 67.7% and 78.9%, respectively.
RFS and overall survival according to the optimal threshold of the nomogram
The median follow-up and initial recurrence time were 29 (range 1–165) and 10 (range 2–61) months, respectively. For the low-risk PPR group, median follow-up and initial PPR time were 36 (range 1–165) and 27 (3–50) months. For the high-risk PPR group, median follow-up and initial PPR time were 25 (3–124) and 9 (2–61) months (Figure 3B).
The 3-year RFS rates were 98.1% (95% CI, 92.8–99.9) and 65.7% (95% CI, 55.5–74.9) for the low- and high-risk PPR groups, respectively (P<0.0001; Figure 3B). The 3-year overall survival rates were 94.4% (95% CI, 87.9–98.0) and 57.8% (95% CI, 47.5–67.6) for the low- and high-risk PPR groups.
Evaluation of existing risk stratification systems used in EC management
The current RSS were tested to evaluate their accuracy to predict PPR (Table 5). The concordance indexes of the FIGO classification, ESMO/ESGO/ESTRO classification, GOG-99 criteria, PORTEC 1 criteria, and SEPAL study were 0.69 (0.59–0.779), 0.70 (0.60–0.788), 0.61(0.507–0.706), 0.58 (0.474–0.678), and 0.685 (0.584–0.774), respectively.
Clinical utility of our prediction model
Our model could be used to design a clinical trial to test the efficacy of systemic chemotherapy or chemoradiation therapy to reduce the risk of PPR. We assumed a 50% risk reduction by adjuvant treatment. If a trial included all patients without any selection criteria, then 92.75% of patients would receive unnecessary treatment and suffer from severe complications. However, a scenario can be suggested based on our risk model. If we enrolled cases with an estimated risk of more than 15%, then the percentage of unnecessarily treated patients and the required size of the study population would both be reduced by 56.5%, whereas the proportion of benefited patients among enrolled patients would increase by 49%. Figure 3C shows how the model could be used to design a clinical trial to test the efficacy of adjuvant treatment to reduce the risk of PPR after adjuvant treatment.
Discussion
The results of the present study demonstrate that our nomogram accurately predicts which women with FIGO stage I–III EC are at risk of PPR. It would appear to be more accurate than the current RSS that are used worldwide to adapt surgical strategies and indications for adjuvant treatments. On the basis of these results, women may be divided into two groups that are highly predictive of PPR. We believe this tool can help select candidates for trials designed to evaluate the efficacy of adjuvant treatment in EC.
Several RSS based on clinical and pathological factors have been developed to standardise EC management (Creutzberg et al, 2000; Keys et al, 2004; Todo et al, 2010). These RSS guide clinicians in their decision-making by grouping women according to their risk group for recurrence. They also form the basis of international guidelines for surgical staging and adjuvant therapies (Todo et al, 2010; Querleu et al, 2011; Colombo et al, 2013; Colombo et al, 2016a). However, such an approach is based on the assumption that all women within a risk group are at equal risk, whereas recent studies have demonstrated that the RSS are not accurate enough to predict recurrence (Bendifallah et al, 2015). To address this limitation, individual characteristics of the woman (such as age and genetic susceptibility) should be taken into account when deciding on a treatment option in addition to tumour biology. In this specific setting, predictive models such as nomograms have been shown to provide reasonable personalised risk estimates that facilitate management-related decisions (Shariat et al, 2009). Hence, optimising outcome in women with EC will require individualised tailoring of care based on multiple clinical and biological risk factors.
Approximately 70% of all EC recurrence occurs within the first 3 years after primary surgery (Fung-Kee-Fung et al, 2006; Ben Arie et al, 2012; Kilgore et al, 2013). We found that women with PPR decline rapidly during the initial 2 years (median time to PPR was 9 months), whereas those with other recurrence sites decline gradually over the years. In fact, more than 50% of women with PPR die during the first year and fewer than 30% survive more than 5 years after recurrence (Bouros et al, 1996; Salani et al, 2011). However, although authors agree that distant metastases are associated with reduced overall survival (Creutzberg et al, 2003), there is no clear consensus to define PPR. In the current study, the PPR group, consisting of women with distant metastases and peritoneal carcinomatosis, had the lowest 3-year overall survival when compared with other sites of recurrence. There are limited data about prognostic factors and outcomes of women whose EC recurs with peritoneal carcinomatosis. This recurrence site has been previously grouped with other sites under the terms: extravaginal (Moschiano et al, 2014), abdominal (Esselen et al, 2011), and extrapelvic (Odagiri et al, 2011; Robbins et al, 2012). When considering peritoneal carcinomatosis as a separate entity, we found a 3-year survival rate of 33.1%. Indeed, the finding that these women had the lowest overall survival rate suggests that further intensification of systemic treatment and exploration of novel therapies may be needed for this group. Women with PPR are generally considered incurable except in the setting of operable situations (e.g., isolated metastases to the liver or lung that can be resected and women with peritoneal carcinomatosis who can undergo successful cytoreduction and have no macroscopic residual disease (Morice et al, 2016). In fact, most of these women are candidates for systemic palliative therapy, but the choice between hormonal treatment and chemotherapy rely on histopathological and clinical features at an individual level. Indeed, progestogens, tamoxifen alternated with megestrol, gonadotropin-releasing hormone analogues, selective oestrogen receptor modulators, and aromatase inhibitors have been used with response rates ranging from 11 to 56% (Panici et al, 2008).
There is a persistent debate about the rationale of adjuvant chemotherapy in standard management of high-intermediate- and high-risk ECs. Although chemotherapy seems to be recommended for high-risk women with lymph node metastasis, its indication for those without is more questionable. The recent European guidelines state that adjuvant systemic therapy is still under investigation for women with type 1 EC at increased risk of recurrence with negative nodal staging or without nodal staging. The results of both ongoing and future trials are expected to further clarify the place of adjuvant chemotherapy or chemoradiation for this subgroup of women. In this specific setting, the current prediction model may be useful to select candidates for such clinical trials, for example, a women who’s age is over 60 years (50 points) in whom lymphadenectomy was not performed (75 points) could be identified with a probability of not having a PPR probability of 25% (or a probability of 75% of having a PPR) based on the definitive pathology results if the tumour was type I (0 points), grade 2 (60 points) with LVSI (100 points) and a FIGO stage II. The personalised risk estimate is of particular interest in that case if substantial comorbidities are present because it informs the discussion of the benefits of adjuvant treatment based on her health status and PPR risk. Indeed, in our scenario, we could reduce unnecessary treatment by 60% using a probability of 15% as a cutoff for study enrolment. Moreover, this selective enrolment strategy could also reduce the number of women to be enrolled by 56.5% as well as reducing the required sample size and the population size to be screened. If all women at high risk were enrolled, 377 would be required for each arm at a power of 90% and an alpha error of 0.25. However, if we only enrolled high-risk women with a probability of recurrence >15% according to the reported optimal threshold, the required sample size would decrease to 164 women for each arm at the same power. Thus, our prediction model may help to reduce the resources required for trials.
The strengths of our study lie in its multicenter nature and the large number of women included. However, some limits deserve to be mentioned. First, we cannot exclude an inherent bias linked to its retrospective nature. Second, during the data collection period, modifications occurred in staging modalities (FIGO classification) and surgical techniques such as lymph node staging (Panici et al, 2008; Pecorelli and Sergio, 2009; Ballester et al, 2011). Finally, our cohort included women from several centres and discrepancies in patient management might have affected our results. However, all included centres were regional referral centres applying the current French guidelines.
In conclusion, we have developed a nomogram to predict PPR in women with FIGO stage I–III EC. It could be used as an additional tool to better select women requiring adjuvant treatment. Our model may also facilitate the design of clinical trials for systemic chemotherapy in EC by selecting a population at high risk of PPR in high-risk EC women.
Change history
22 November 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Akaike H (1985) Prediction and entropy. In AC Atkinson, SE Fienberg, (eds), A Celebration of Statistics Springer: New York, NY, USA, pp 1–24.
Amant F, Moerman P, Neven P, Timmerman D, Van Limbergen E, Vergote I (2005) Endometrial cancer. Lancet 366 (9484): 491–505.
Ballester M, Dubernard G, Lécuru F, Heitz D, Mathevet P, Marret H, Querleu D, Golfier F, Leblanc E, Rouzier R, Darai E (2011) Detection rate and diagnostic accuracy of sentinel-node biopsy in early stage endometrial cancer: a prospective multicentre study (SENTI-ENDO). Lancet Oncol 12 (5): 469–476.
Ben Arie A, Lavie O, Gdalevich M, Voldarsky M, Barak F, Schneider D, Levy T, Anteby E, Gemer O (2012) Temporal pattern of recurrence of stage I endometrial cancer in relation to histological risk factors. Eur J Surg Oncol 38 (2): 166–169.
Bendifallah S, Canlorbe G, Collinet P, Arsène E, Huguet F, Coutant C, Hudry D, Graesslin O, Raimond E, Touboul C, Darai E, Ballester M (2015) Just how accurate are the major risk stratification systems for early-stage endometrial cancer? Br J Cancer 112 (5): 793–801.
Benedetti Panici P, Basile S, Maneschi F, Alberto Lissoni A, Signorelli M, Scambia G, Angioli R, Tateo S, Mangili G, Katsaros D, Garozzo G, Campagnutta E, Donadello N, Greggi S, Melpignano M, Raspagilesi F, Ragni N, Cormio G, Grassi R, Franchi M, Giannarelli D, Fossati R, Torri V, Amoroso M, Crocè C, Mangioni C (2008) Systematic pelvic lymphadenectomy vs no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Ins 100 (23): 1707–1716.
Bouros D, Papadakis K, Siafakas N, Fuller AF (1996) Natural history of patients with pulmonary metastases from uterine cancer. Cancer 78 (3): 441–447.
Colombo N, Creutzberg C, Amant F, Bosse T, González-Martín A, Ledermann J, Marth C, Nout R, Querleu D, Mirza MR, Sessa C ESMO-ESGO-ESTRO Endometrial Consensus Working Group (2016a) ESMO-ESGO-ESTRO consensus conference on endometrial cancer: diagnosis, treatment and follow-up. Ann Oncol 27 (1): 16–41.
Colombo N, Creutzberg C, Amant F, Bosse T, González-Martín A, Ledermann J, Marth C, Nout R, Querleu D, Mirza MR, Sessa C ESMO-ESGO-ESTRO Endometrial Consensus Working Group (2016b) ESMO-ESGO-ESTRO consensus conference on endometrial cancer: diagnosis, treatment and follow-up. Int J Gynecol Cancer 26 (1): 2–30.
Colombo N, Preti E, Landoni F, Carinelli S, Colombo A, Marini C, Sessa C ESMO Guidelines Working Group (2013) Endometrial cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 24 (Suppl 6): vi33–vi38.
Creasman WT, Morrow CP, Bundy BN, Homesley HD, Graham JE, Heller PB (1987) Surgical pathologic spread patterns of endometrial cancer. a Gynecologic Oncology Group Study. Cancer 60 (8 Suppl): 2035–2041.
Creutzberg CL, van Putten WL, Koper PC, Lybeert ML, Jobsen JJ, Wárlám-Rodenhuis CC, De Winter KA, Lutgens LC, Van den Bergh AC, Van de Steen-Banasik E, Beerman H, Van Lent M PORTEC Study Group (2003) Survival after relapse in patients with endometrial cancer: results from a randomized trial. Gynecol Oncol 89 (2): 201–209.
Creutzberg CL, van Putten WL, Koper PC, Lybeert ML, Jobsen JJ, Wárlám-Rodenhuis CC, De Winter KA, Lutgens LC, Van den Bergh AC, Van de Steen-Banasik E, Beerman H, Van Lent M (2000) Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: multicentre randomised trial. PORTEC Study Group. Post operative radiation therapy in endometrial carcinoma. Lancet 355 (9213): 1404–1411.
Daraï E, Dubernard G, Bats AS, Heitz D, Mathevet P, Marret H, Querleu D, Golfier F, Leblanc E, Rouzier R, Ballester M (2015) Sentinel node biopsy for the management of early stage endometrial cancer: long-term results of the SENTI-ENDO Study. Gynecol Oncol 136 (1): 54–59.
Esselen KM, Boruta DM, del Carmen M, Schorge JO, Goodman A, Growdon WB (2011) Defining prognostic variables in recurrent endometrioid endometrial cancer: a 15-year single-institution review. Int J Gynecol Cancer 21 (6): 1078–1083.
Fung-Kee-Fung M, Dodge J, Elit L, Lukka H, Chambers A, Oliver T Cancer Care Ontario Program in Evidence-based Care Gynecology Cancer Disease Site Group (2006) Follow-up after primary therapy for endometrial cancer: a systematic review. Gynecol Oncol 101 (3): 520–529.
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143 (1): 29–36.
Harrell FE, Lee KL, Pollock BG (1988) Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst 80 (15): 1198–1202.
Heagerty PJ, Lumley T, Pepe MS (2000) Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 56 (2): 337–344.
Keys HM, Roberts JA, Brunetto VL, Zaino RJ, Spirtos NM, Bloss JD, Pearlman A, Maiman MA, Bell JG Gynecologic Oncology Group (2004) A phase III trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma: a Gynecologic Oncology Group Study. Gynecol Oncol 92 (3): 744–751.
Kilgore JE, Jackson AL, Ko EM, Soper JT, Van Le L, Gehrig PA, Boggess JF (2013) Recurrence-free and 5-year survival following robotic-assisted surgical staging for endometrial carcinoma. Gynecol Oncol 129 (1): 49–53.
Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E (2016) Endometrial cancer. Lancet 387 (10023): 1094–1108.
Morrow CP, Bundy BN, Kurman RJ, Creasman WT, Heller P, Homesley HD, Graham JE (1991) Relationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: a Gynecologic Oncology Group Study. Gynecol Oncol 40 (1): 55–65.
Moschiano EJ, Barbuto DA, Walsh C, Singh K, Euscher ED, Roma AA, Ali-Fehmi R, Frauenhoffer EE, Montiel DP, Kim I, Diordjevic B, Malpica A, Hong SR, Silva EG (2014) Risk factors for recurrence and prognosis of low-grade endometrial adenocarcinoma; vaginal versus other sites. Int J Gynecol Pathol 33 (3): 268–273.
Odagiri T, Watari H, Hosaka M, Mitamura T, Konno Y, Kato T, Kobayashi N, Sudo S, Takeda M, Kaneuchi M, Sakuragi N (2011) Multivariate survival analysis of the patients with recurrent endometrial cancer. J Gynecol Oncol 22 (1): 3–8.
Pecorelli Sergio (2009) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol 105 (2): 103–104.
Querleu D, Planchamp F, Narducci F, Morice P, Joly F, Genestie C, Haie-Meder C, Thomas L, Quénel-Tueux N, Darai E, Dorangeon PH, Marret H, Taieb S, Mazeau-Woynar V Institut National du Cancer and the Société Française d'Oncologie Gynécologique (2011) Clinical practice guidelines for the management of patients with endometrial cancer in France: recommendations of the Institut National Du Cancer and the Société Française d’Oncologie Gynécologique. Int J Gynecol Cancer 21 (5): 945–950.
Robbins JR, Yechieli R, Laser B, Mahan M, Rasool N, Elshaikh MA (2012) Is time to recurrence after hysterectomy predictive of survival in patients with early stage endometrial carcinoma? Gynecol Oncol 127 (1): 38–42.
Salani R, Nagel CI, Drennen E, Bristow RE (2011) Recurrence patterns and surveillance for patients with early stage endometrial cancer. Gynecol Oncol 123 (2): 205–207.
Schisterman EF, Perkins NJ, Liu A, Bondell H (2005) Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 16 (1): 73–81.
Shariat SF, Capitanio U, Jeldres C, Karakiewicz PI (2009) Can nomograms be superior to other prediction tools? BJU Int 103 (4): 492–495, ; discussion 495–497.
Steyerberg EW . Clinical prediction models: a practical approach to development validation, and updating (2009) In Statistics for Biology and Health. Springer: New York.
Todo Y, Kato H, Kaneuchi M, Watari H, Takeda M, Sakuragi N (2010) Survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL Study): a retrospective cohort analysis. Lancet 375 (9721): 1165–1172.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Ouldamer, L., Bendifallah, S., Body, G. et al. Predicting poor prognosis recurrence in women with endometrial cancer: a nomogram developed by the FRANCOGYN study group. Br J Cancer 115, 1296–1303 (2016). https://doi.org/10.1038/bjc.2016.337
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.337
Keywords
This article is cited by
-
Development and validation of a prognostic nomogram model incorporating routine laboratory biomarkers for preoperative patients with endometrial cancer
BMC Cancer (2023)
-
Development and validation of a nomogram for predicting recurrence-free survival in endometrial cancer: a multicenter study
Scientific Reports (2023)
-
Development and validation of MRI-based radiomics model to predict recurrence risk in patients with endometrial cancer: a multicenter study
European Radiology (2023)
-
Machine learning methods to predict presence of residual cancer following hysterectomy
Scientific Reports (2022)
-
The Prediction of Recurrence in Low-Risk Endometrial Cancer: Is It Time for a Paradigm Shift in Adjuvant Therapy?
Reproductive Sciences (2022)