Abstract
Background:
Angiogenesis is crucial for glioblastoma growth, and anti-vascular endothelial growth factor agents are widely used in recurrent glioblastoma patients. The number of circulating endothelial cells (CECs) is a surrogate marker for endothelial damage. We assessed their kinetics and explored their prognostic value in patients with recurrent glioblastoma.
Methods:
In this side study of the BELOB trial, 141 patients with recurrent glioblastoma were randomised to receive single-agent bevacizumab or lomustine, or bevacizumab plus lomustine. Before treatment, after 4 weeks and after 6 weeks of treatment, CECs were enumerated.
Results:
The number of CECs increased during treatment with bevacizumab plus lomustine, but not during treatment in the single-agent arms. In patients treated with lomustine single agent, higher absolute CEC numbers after 4 weeks (log10CEC hazard ratio (HR) 0.41, 95% CI 0.18–0.91) and 6 weeks (log10CEC HR 0.16, 95% CI 0.05–0.56) of treatment were associated with improved overall survival (OS). Absolute CEC numbers in patients receiving bevacizumab plus lomustine or bevacizumab single agent were not associated with OS.
Conclusion:
CEC numbers increased during treatment with bevacizumab plus lomustine but not during treatment with either agent alone, suggesting that this combination induced the greatest vascular damage. Although the absolute number of CECs was not associated with OS in patients treated with bevacizumab either alone or in combination, they could serve as a marker in glioblastoma patients receiving lomustine single agent.
Similar content being viewed by others
Main
Glioblastoma is the most common and most aggressive malignant primary brain tumour in adults. Angiogenesis is crucial for glioblastoma growth, and the presence of endothelial proliferation is a key WHO criterion for diagnosing glioblastoma (Louis et al, 2007). Tumour vessels in glioblastoma are morphologically and functionally different from normal blood vessels and are characterised by their high complexity, disorganisation and leakiness (Jain et al, 2007). Hypoxic glioblastoma tumour cells are able to interact with endothelial cells and promote angiogenesis by producing high numbers of vascular endothelial growth factor (VEGF; Plate et al, 1992; Salmaggi et al, 2003). Therefore, a strong rationale exists for using anti-VEGF agents such as bevacizumab, a humanised monoclonal antibody against circulating VEGF, in the treatment of glioblastoma. Accordingly, numerous clinical trials have explored the value of bevacizumab in glioblastoma patients (Friedman et al, 2009; Chinot et al, 2014; Gilbert et al, 2014), but none of them showed clear survival benefit of single-agent bevacizumab in newly diagnosed or recurrent glioblastoma.
Treatment response is critical in these studies and in daily clinical practice and is generally assessed by radiographic response on MRI. However, besides interobserver (Hayward et al, 2008) and intraobserver (Provenzale and Mancini, 2012) variability in radiographic assessments, clear limitations are encountered with current treatment response evaluation in glioblastoma, especially in patients treated with anti-VEGF monoclonal antibodies. Most importantly, the administration of anti-VEGF monoclonal antibodies may result in radiographic pseudoresponse caused by the rapid normalisation of abnormally permeable blood vessels (van den Bent et al, 2009). Although these issues were taken into account in the revised response assessment criteria proposed by the Response Assessment in Neuro-Oncology (RANO) working group (Wen et al, 2010), alternative methods of response assessment focusing on the extent of angiogenesis could be helpful to guide prognosis and treatment success in glioblastoma.
Circulating endothelial cells (CECs) are mature endothelial cells that are present in the peripheral circulation and are presumed to be a marker of vascular injury (Blann et al, 2005) and angiogenesis. CECs were shown to have a clinically relevant prognostic value in various solid tumours (Kraan et al, 2012a). Given the high rate of angiogenesis in glioblastomas and the lack of prognostic markers for anti-VEGF treatments in general, we prospectively assessed the kinetics and prognostic relevance of CECs in the BELOB trial (Taal et al, 2014). In this randomised phase II trial, patients were treated for recurrent glioblastoma with bevacizumab plus lomustine, or with bevacizumab or lomustine single agent.
Materials and Methods
Patients and treatment
This prospective study was a side study of the randomised multi-centre phase II trial from the Dutch Neuro-Oncology Group (LWNO) ‘BELOB’ (Netherlands Trial Register ID NTR1929). In-depth information regarding eligibility criteria, treatment and outcome assessments were described in the paper regarding the primary clinical end points of the study (Taal et al, 2014). In brief, patients with recurrent glioblastoma were stratified according to centre, ECOG performance status and age, to be subsequently randomised between bevacizumab in combination with lomustine, bevacizumab single agent or lomustine single agent.
Lomustine was given orally every 6 weeks, for a maximum of six cycles. Bevacizumab was given intravenously every 2 weeks until disease progression. One treatment cycle was defined as 6 weeks. Overall survival (OS) was measured from the day of randomisation until death from any cause.
The central and local institutional review boards approved the protocol and all patients provided written informed consent. Peripheral blood samples for CEC analyses were acquired in CellSave tubes (Janssen Diagnostics, Raritan, NJ, USA) before the start of treatment (baseline) and after 4 and 6 weeks of treatment. Samples were maintained at room temperature and processed within 96 h of blood collection.
Enumeration of CECs
CECs were enumerated according to our previously reported flow cytometric approach (Kraan et al, 2012b), in which we demonstrated excellent reproducibility of the assay between duplicate CEC samples. The following directly conjugated monoclonal antibodies were used to identify CEC – CD34-FITC (clone 8G12; BD Biosciences, San Jose, CA, USA), CD146-APC (clone 541–10B2; Miltenyi Biotec GmbH, Bergisch Gladbach, Germany) and CD45-PerCP (clone 2D1; BD Biosciences). DRAQ5 (Biostatus Ltd, Shepshed, UK) was used as a cell permeable nuclear dye to exclude platelets and microparticles. The definition of a CEC was CD34+, CD146+, CD45− and DRAQ5+.
Samples were acquired on an FACS Canto II or Fortessa flow cytometer (BD Biosciences) and were later analysed using FCS Express (De Novo Software, Los Angeles, CA, USA). One experienced technician (JK) evaluated and checked all the analyses before the result of the CEC enumeration were considered final to minimise inter-rater variability.
Statistical analysis
Several time intervals were constructed to minimise interpatient variability regarding the time of CEC measurement. For a sample to be eligible as a baseline sample, the blood should have been drawn at least within 2 weeks before the start of treatment. A sample was eligible as a 4 weeks sample if the sample was drawn between days +25 and +31 after treatment start, whereas a sample was eligible as a 6 weeks sample if the sample was drawn before the administration of the second cycle and between days +39 and +45 after treatment start.
For comparisons between CEC numbers at baseline versus during treatment in the same treatment arm, the Wilcoxon signed-rank test was used. Correlation between corticosteroid use and CEC numbers was assessed using point biserial correlation. Correlation between maximum tumour diameter and CEC numbers was assessed using the Spearman correlation. CEC values were log10-normalised before inclusion in Cox regression analyses. For the increase or decrease of CECs relative to baseline, the logarithm was calculated of the quotient between baseline (t0) and the appropriate time point (tx), formula: log10(tx/t0).
In case a statistically significant result was observed in the univariate Cox regression crude hazard ratio (HR) calculation, an adjusted HR was calculated adjusting for maximum tumour diameter and corticosteroid use at baseline or after 6 weeks of treatment. These parameters were not available for 4 weeks after the start of treatment sample and thus no adjusted HRs were calculated for this sample. Maximum enhancing tumour diameter was assessed by RANO criteria (Wen et al, 2010). For a maximum diameter to be eligible for adjustment in the multivariate model after 6 weeks of treatment, the corresponding MRI should have been performed before the administration of the second cycle of lomustine (only if applicable). All reported P-values are two sided, and a significance level α=0.05 was used. All data analyses were done using Stata/SE version 12 (StataCorp LP, College Station, TX, USA).
Results
Patient and treatment characteristics
A total of 153 patients were enrolled in the BELOB study between December 2009 and November 2011. From the 148 eligible patients as reported in the paper regarding the primary end point (Taal et al, 2014), 141 patients were included in this side study. Patient and treatment characteristics are presented in Table 1. Fifty-one patients were randomised in the bevacizumab plus lomustine arm, 48 patients received bevacizumab single-agent therapy, whereas 42 patients received lomustine single-agent therapy. Only four patients were still alive at the end of follow-up, and these patients had a median follow-up of 35.3 months (range 28.9–41.5 months).
CEC measurements and kinetics
A total of 382 samples were evaluated for the presence of CECs. Thirty samples were excluded from the analysis because they were not drawn in the appropriate time interval (n=28) or because they were drawn after the administration of the second cycle (n=2). Consequently, out of 423 expected samples, 352 samples (83% of expected samples) were included in the final analysis, of which 129 were eligible as baseline samples, 119 were eligible as 4 weeks samples and 104 were eligible as 6 weeks samples (Table 2).
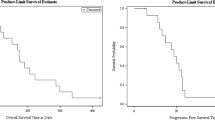
Baseline CEC numbers were not significantly correlated with corticosteroid use (r=0.06, P=0.54) or the maximum diameter of the tumour lesion (r=−0.11, P=0.22). As we expected that CEC kinetics would differ between the three treatment arms, we analysed CEC kinetics separately in each treatment arm (Figure 1). In patients receiving bevacizumab plus lomustine combination therapy, patients had higher CECs after 4 weeks (P<0.001) and 6 weeks (P<0.001) of treatment compared with the baseline value. In contrast, in patients receiving bevacizumab single agent and in patients receiving lomustine single agent, CECs at baseline were similar to CECs after 4 weeks and 6 weeks of treatment.
Association of CEC numbers with OS
The prognostic relevance of CECs with respect to overall survival in this study was explored using a Cox regression model. No association was found between the absolute number of CECs at baseline and overall survival. As we observed that CEC kinetics differed between the three treatment arms, Cox regression for absolute CEC counts after 4 weeks and 6 weeks of treatment with respect to OS was performed separately for each treatment arm (Table 3). In patients receiving bevacizumab plus lomustine and bevacizumab single agent, no significant associations between absolute CEC counts and OS were observed. However, in patients receiving lomustine single agent, an association between OS and higher absolute CEC counts at 4 weeks (log10CEC 4 weeks HR 0.41, 95% CI 0.18–0.91) and 6 weeks (log10CEC 6 weeks HR 0.16, 95% CI 0.05–0.56) was observed. After addition of data regarding corticosteroid use and the maximum tumour diameter after 6 weeks of treatment to the model, the CEC count after 6 weeks was still significantly associated with OS (log10CEC 6 weeks HR 0.18, 95% CI 0.05–0.74).
Besides the absolute threshold model as described above, we also analysed whether changes in CECs from baseline to 4 weeks and baseline to 6 weeks were associated with OS in the Cox regression model. In contrast to our findings using the absolute CEC numbers after 4 weeks and 6 weeks of treatment, we did not observe any association between CEC changes and OS.
Discussion
There is a clear clinical unmet need for alternative response evaluation during the treatment of glioblastoma. As glioblastomas are highly angiogenic tumours, we proposed CEC enumeration as a surrogate marker for endothelial damage and assessed CEC kinetics and explored their possible prognostic relevance during the randomised BELOB trial. We observed that CECs increased only during treatment in patients receiving combination treatment with bevacizumab plus lomustine. We also found an association between higher absolute CEC numbers and improved overall survival during treatment with lomustine single agent, but not in bevacizumab-treated patients.
Our observation of increased CECs during treatment with bevacizumab plus lomustine in contrast to the single-agent treatment arms suggests that there is a synergistic effect of bevacizumab and lomustine in triggering endothelial damage. The results from the BELOB study suggested survival benefit from the combination of bevacizumab and lomustine, as the primary end point (OS at 9 months) was reached to justify the exploration of this combination treatment in a phase III trial (Taal et al, 2014). Our results indicate that this treatment combination may have had a positive effect in triggering endothelial damage in the glioblastoma tumour itself. Our observation of increased CECs during treatment with bevacizumab and lomustine cytotoxic chemotherapy is in accordance with previous reports in metastatic breast cancer and advanced colorectal cancer (Bidard et al, 2010; Simkens et al, 2010), in which CEC numbers were increased after combination treatment with cytotoxic chemotherapy and bevacizumab.
During treatment with the single-agent lomustine cytotoxic chemotherapy, CEC numbers remained stable. Reynes et al (2013) observed a similar pattern in glioblastoma patients before and after treatment with cytotoxic chemotherapy and radiotherapy. To our knowledge, no other studies have reported on CEC changes during bevacizumab single-agent therapy; therefore, our finding of stable CECs during bevacizumab single-agent therapy remains to be confirmed by other studies.
We did not observe an association between baseline CEC counts and OS. In addition, we explored whether or not absolute CEC numbers during treatment or the relative changes during treatment were associated with outcome. During single-agent therapy with lomustine, an association was revealed between improved OS and higher absolute CEC numbers after 4 weeks and 6 weeks of treatment. As we observed the association between CECs and OS in the patients receiving single-agent lomustine after both 4 weeks and 6 weeks of treatment, and this association remained statistically significant in multivariable Cox regression analysis, it is unlikely that these findings are false positives. Our findings that CEC changes relative to baseline did not correlate with OS, suggests that the absolute CEC number, which reflects the extent of endothelial damage during treatment at a specific point in time, is more important than the actual pattern of endothelial damage over time.
The lack of association between baseline CECs and OS is in contrast to two other glioblastoma studies (Cuppini et al, 2013; Reynes et al, 2013). It should, however, be noted that in these studies other CEC enumeration techniques were used. It is known that the CEC compartment in patients with solid tumours consists of both tumour-derived endothelial cells (tumour CECs; tCECs) and normal tissue-derived endothelial cells (normal CECs; nCECs). There are a few potential pitfalls associated with measuring the nCEC compartment. Since the nCEC compartment is relatively large, smaller changes taking place in the tCEC compartment may be masked. In addition, changes in the nCEC compartment because of non-tumour-related causes might lead to incorrect interpretations regarding the tCEC compartment. The use of tumour-endothelial markers therefore allows more precise tCEC measurement. Cuppini et al (2013) used a putative tumour-endothelial-specific marker (CD109) to detect CECs in their study.
The study by Cuppini et al reported decreased CD109-positive CECs in patients who responded to bevacizumab plus irinotecan and bevacizumab single agent after 2 months of treatment, whereas we could not find such associations for the bevacizumab-containing regimens in our study. Interestingly, although the study by Cuppini et al did not observe such an association between CD109-CECs and response in patients receiving cytotoxic chemotherapy, we observed that higher CEC numbers were associated with improved OS only in the single-agent lomustine cytotoxic chemotherapy group. It should be realised, however, that there are important differences between the used CEC enumeration method by Cuppini et al and our CEC enumeration method, which may explain differences in prognostic value between our studies. Cuppini et al investigated an entirely different CEC population than we did, with no CD146 expression (Mancuso et al, 2014). While they used CD31 to identify a CD109-positive, CD146-negative CEC population and a separate CD146-positive, CD109-negative CEC population with no overlap of both markers, we used CD34 to identify CD146-positive CECs. Apart from these differences in CEC enumeration techniques, differences in the chosen fixed time points and differences in treatment regimens may also explain the differences between our studies. Another explanation for the differences between our studies may be that single-agent irinotecan has no proven efficacy in glioblastoma (Friedman et al, 2009), in contrast to lomustine.
The most likely explanation that can be thought of as to why we observed prognostic value of CECs in the patients receiving lomustine single agent but not in patients receiving bevacizumab-based therapy is our sample size. Although the number of patients per treatment arm was relatively large for any study evaluating recurrent glioblastoma patients, only a limited number of patients were evaluated per treatment arm. This may have provided insufficient statistical power to associate CEC numbers with OS in the bevacizumab-based treatment arms. However, we can speculate on biological mechanisms that may have accounted for the lack of prognostic value in the bevacizumab-based treatment arms as well. As CEC numbers remained stable in the whole group of lomustine single-agent-treated patients, high CEC numbers during treatment in the lomustine single-agent arm may represent only those patients in whom a larger extent of endothelial damage was present as a consequence of more lomustine-induced damage of the tumour. In contrast to the lomustine single-agent arm, CECs increased in the whole group of patients receiving bevacizumab plus lomustine, suggesting that endothelial damage occurred in the majority of these patients. The origin of CECs responsible for the increased CEC counts (from the tumour vasculature or the normal vasculature) is however unknown. Endothelial damage of tumour vessels might have occurred in the majority of patients because of an improved penetration of lomustine into the tumour, which has been demonstrated in preclinical experiments using neuroblastoma xenografts treated with bevacizumab and systemic chemotherapy (Dickson et al, 2007). Alternatively, combination treatment with lomustine and bevacizumab might have triggered significant endothelial damage in normal tissues in addition to tumour tissue, consequently masking changes in the tCEC compartment. Both these mechanisms may have made it more challenging to associate CECs with outcome in the bevacizumab plus lomustine combination arm, which further stresses the high need for robust assays to discriminate tCECs from nCECs. The lack of association between CEC numbers and outcome in the bevacizumab single-agent arm is probably due to the fact that bevacizumab as a single agent has low activity in glioblastoma (Taal et al, 2014).
There are several strong points of our study including the randomised set-up of our study, the high number of collected samples and the use of OS as the end point for associations with CECs. However, our study also had some limitations. The number of patients per treatment was relatively limited. In addition to limiting the statistical power of associating CEC numbers with OS in the bevacizumab-based treatment arms as mentioned before, the limited number of patients prevented a definition of CEC cutoff points associated with prognosis and did not allow intergroup comparisons.
Another limitation is that the CEC assay used in our study does not specifically detect tumour-derived CECs. Our observation that CECs increased during treatment with bevacizumab plus lomustine but were not associated with prognosis, may have been caused by changes occurring in the nCEC compartment, therefore masking changes in the tCEC compartment. We recently reported that CD276 is a putative tCEC marker that was expressed more highly in CECs from patients with glioblastoma than in CECs from healthy donors (Kraan et al, 2014). We are currently participating in an EORTC phase III study that compares outcomes following bevacizumab plus lomustine versus lomustine single agent in recurrent glioblastoma (trial registry number NCT01290939); it includes a side study to evaluate the clinical value of CD276+ tCECs. This will enable us to validate our findings regarding the prognostic value of CECs and possibly CD276+ tCECs in glioblastoma patients receiving lomustine single agent. In addition, as we believe CD276+ tCECs are more sensitive for measuring the tCEC compartment, we hope to identify the true clinical value in patients receiving bevacizumab plus lomustine combination therapy.
Altogether, the results from our study indicate that it may be worthwhile to further explore CEC enumeration as a marker in recurrent glioblastoma, as was also suggested by Cuppini et al. Given the heterogeneity of tumour types and patient populations, different antitumour agents administered and different CEC enumeration techniques used, one should nonetheless be careful in interpreting CEC data between studies (Strijbos et al, 2008; Kraan et al, 2012a). Consensus is needed on the optimal CEC enumeration technique, as this would enable researchers to compare the findings between studies and ultimately take the application of CECs to the next level. In addition, the initiation of studies using promising tCEC markers will be essential for CECs to eventually make it as a reliable and robust biomarker in clinical oncology.
Change history
14 July 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bidard FC, Mathiot C, Degeorges A, Etienne-Grimaldi MC, Delva R, Pivot X, Veyret C, Bergougnoux L, de Cremoux P, Milano G, Pierga JY (2010) Clinical value of circulating endothelial cells and circulating tumor cells in metastatic breast cancer patients treated first line with bevacizumab and chemotherapy. Ann Oncol 21: 1765–1771.
Blann AD, Woywodt A, Bertolini F, Bull TM, Buyon JP, Clancy RM, Haubitz M, Hebbel RP, Lip GY, Mancuso P, Sampol J, Solovey A, Dignat-George F (2005) Circulating endothelial cells. Biomarker of vascular disease. Thromb Haemost 93: 228–235.
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea D, Brandes AA, Hilton M, Abrey L, Cloughesy T (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370: 709–722.
Cuppini L, Calleri A, Bruzzone MG, Prodi E, Anghileri E, Pellegatta S, Mancuso P, Porrati P, Di Stefano AL, Ceroni M, Bertolini F, Finocchiaro G, Eoli M (2013) Prognostic value of CD109+ circulating endothelial cells in recurrent glioblastomas treated with bevacizumab and irinotecan. PLoS One 8: e74345.
Dickson PV, Hamner JB, Sims TL, Fraga CH, Ng CY, Rajasekeran S, Hagedorn NL, McCarville MB, Stewart CF, Davidoff AM (2007) Bevacizumab-induced transient remodeling of the vasculature in neuroblastoma xenografts results in improved delivery and efficacy of systemically administered chemotherapy. Clin Cancer Res 13: 3942–3950.
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27: 4733–4740.
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, Jeraj R, Brown PD, Jaeckle KA, Schiff D, Stieber VW, Brachman DG, Werner-Wasik M, Tremont-Lukats IW, Sulman EP, Aldape KD, Curran WJ Jr., Mehta MP (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370: 699–708.
Hayward RM, Patronas N, Baker EH, Vezina G, Albert PS, Warren KE (2008) Inter-observer variability in the measurement of diffuse intrinsic pontine gliomas. J Neurooncol 90: 57–61.
Jain RK, di Tomaso E, Duda DG, Loeffler JS, Sorensen AG, Batchelor TT (2007) Angiogenesis in brain tumours. Nat Rev Neurosci 8: 610–622.
Kraan J, Sleijfer S, Foekens JA, Gratama JW (2012a) Clinical value of circulating endothelial cell detection in oncology. Drug Discov Today 17: 710–717.
Kraan J, Strijbos MH, Sieuwerts AM, Foekens JA, den Bakker MA, Verhoef C, Sleijfer S, Gratama JW (2012b) A new approach for rapid and reliable enumeration of circulating endothelial cells in patients. J Thromb Haemost 10: 931–939.
Kraan J, van den Broek P, Verhoef C, Grunhagen DJ, Taal W, Gratama JW, Sleijfer S (2014) Endothelial CD276 (B7-H3) expression is increased in human malignancies and distinguishes between normal and tumour-derived circulating endothelial cells. Br J Cancer 111: 149–156.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114: 97–109.
Mancuso P, Calleri A, Gregato G, Labanca V, Quarna J, Antoniotti P, Cuppini L, Finocchiaro G, Eoli M, Rosti V, Bertolini F (2014) A subpopulation of circulating endothelial cells express CD109 and is enriched in the blood of cancer patients. PLoS One 9: e114713.
Plate KH, Breier G, Weich HA, Risau W (1992) Vascular endothelial growth factor is a potential tumour angiogenesis factor in human gliomas in vivo. Nature 359: 845–848.
Provenzale JM, Mancini MC (2012) Assessment of intra-observer variability in measurement of high-grade brain tumors. J Neurooncol 108: 477–483.
Reynes G, Vila V, Fleitas T, Reganon E, Font de Mora J, Jorda M, Martinez-Sales V (2013) Circulating endothelial cells and procoagulant microparticles in patients with glioblastoma: prognostic value. PLoS One 8: e69034.
Salmaggi A, Eoli M, Frigerio S, Silvani A, Gelati M, Corsini E, Broggi G, Boiardi A (2003) Intracavitary VEGF, bFGF, IL-8, IL-12 levels in primary and recurrent malignant glioma. J Neurooncol 62: 297–303.
Simkens LH, Tol J, Terstappen LW, Teerenstra S, Punt CJ, Nagtegaal ID (2010) The predictive and prognostic value of circulating endothelial cells in advanced colorectal cancer patients receiving first-line chemotherapy and bevacizumab. Ann Oncol 21: 2447–2448.
Strijbos MH, Gratama JW, Kraan J, Lamers CH, den Bakker MA, Sleijfer S (2008) Circulating endothelial cells in oncology: pitfalls and promises. Br J Cancer 98: 1731–1735.
Taal W, Oosterkamp HM, Walenkamp AM, Dubbink HJ, Beerepoot LV, Hanse MC, Buter J, Honkoop AH, Boerman D, de Vos FY, Dinjens WN, Enting RH, Taphoorn MJ, van den Berkmortel FW, Jansen RL, Brandsma D, Bromberg JE, van Heuvel I, Vernhout RM, van der Holt B, van den Bent MJ (2014) Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): a randomised controlled phase 2 trial. Lancet Oncol 15: 943–953.
van den Bent MJ, Vogelbaum MA, Wen PY, Macdonald DR, Chang SM (2009) End point assessment in gliomas: novel treatments limit usefulness of classical Macdonald's Criteria. J Clin Oncol 27: 2905–2908.
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, Degroot J, Wick W, Gilbert MR, Lassman AB, Tsien C, Mikkelsen T, Wong ET, Chamberlain MC, Stupp R, Lamborn KR, Vogelbaum MA, van den Bent MJ, Chang SM (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28: 1963–1972.
Acknowledgements
This study was financially supported by Roche Netherlands. The study was also supported by grant number DDHK 2010–4678 from the ‘KWF Kankerbestrijding’ (Dutch Cancer Society).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
MJvdB has done paid consultancy for Roche, Abbvie, Celldex, Amgen, and Merck Ag; has received research grants from Roche and AbbVie; and has been on the speakers' bureau for MSD. HMO has received personal fees from Roche for consultancy. The other authors declare no competing interests.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Beije, N., Kraan, J., Taal, W. et al. Prognostic value and kinetics of circulating endothelial cells in patients with recurrent glioblastoma randomised to bevacizumab plus lomustine, bevacizumab single agent or lomustine single agent. A report from the Dutch Neuro-Oncology Group BELOB trial. Br J Cancer 113, 226–231 (2015). https://doi.org/10.1038/bjc.2015.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.191
Keywords
This article is cited by
-
Improved diagnosis and prognostication of patients with pleural malignant mesothelioma using biomarkers in pleural effusions and peripheral blood samples – a short report
Cellular Oncology (2017)
-
RETRACTED ARTICLE: CD109 Mediates Cell Survival in Hepatocellular Carcinoma Cells
Digestive Diseases and Sciences (2016)