Abstract
Background:
Diabetes mellitus has been associated with an increased risk of bladder cancer, although the evidence is still open to discussion.
Methods:
We examined this association using data from a multicentre Italian case–control study, conducted between 2003 and 2014 on 690 bladder cancer cases and 665 frequency-matched hospital controls. Odds ratios (ORs) for diabetes were estimated by unconditional multiple logistic regression models, after allowance for major known risk factors for bladder cancer.
Results:
One hundred and twelve (16.2%) cases and 57 (8.6%) controls reported a diagnosis of diabetes mellitus, corresponding to a multivariate OR of 2.09 (95% confidence interval (CI): 1.46–3.01). Bladder cancer risk increased with duration of diabetes (OR 1.92 for 1–<5 years, 1.63 for 5–<10 years, 2.39 for 10–<15 years, and 2.58 for ⩾15 years). The increased risk of bladder cancer was consistent in strata of age and education, whereas it was somewhat lower (although not significantly) in women (OR 1.18), in never (OR 1.31) and current (OR 1.42) smokers, and in subjects with a body mass index <25 kg m−2 (OR 1.48).
Conclusion:
The present study provides further support of a role of diabetes in bladder cancer aetiology, although some residual confounding by tobacco, body mass index, or other unmeasured covariates may partly explain the association observed.
Similar content being viewed by others
Main
In the European Union, bladder cancer is the fifth most common cancer type and the ninth leading cause of cancer mortality, with about 40 000 deaths every year (Ferlay et al, 2013; Bosetti et al, 2013a). Its major recognised risk factor is tobacco smoking, with smokers having a three- to four-fold excess risk as compared with never smokers (Zeegers et al, 2000; IARC, 2004). Other known risk factors for bladder cancer include exposures to a few industrial chemicals (mainly aromatic amines in the past), drinking water contaminants, phenacetin-containing analgesics, and possibly selected aspects of diet (Villanueva et al, 2004; Silverman et al, 2006; World Cancer Research Fund and American Institute for Cancer Research, 2007; Letasiova et al, 2012).
Diabetes mellitus – an important determinant of various common neoplasms (Renehan et al, 2010) – has also been associated with an increased risk of bladder cancer, although the evidence is still open to discussion (Larsson et al, 2006; Newton et al, 2013; Prizment et al, 2013; Zhu et al, 2013a, 2013b; Cantiello et al, 2015). A meta-analysis conducted in 2006 on seven case–control studies, three cohort studies, and six cohort studies in diabetic patients reported an overall relative risk (RR) of 1.24 (95% confidence interval (CI): 1.08–1.42), with a consistent RR in case–control studies (RR 1.37) and in cohort studies (RR 1.43), but no association in the cohorts of diabetic patients (RR 1.01) (Larsson et al, 2006). Consistent results were reported in two subsequent meta-analyses based on at least 9 case–control studies and 29 cohort studies, with pooled RRs ranging between 1.35 and 1.45 (Zhu et al, 2013a, 2013b). A few studies examining the duration-risk relationship reported conflicting results (Atchison et al, 2011; MacKenzie et al, 2011; Tseng, 2011; Newton et al, 2013; Prizment et al, 2013).
We further examined the association between diabetes and bladder cancer risk using data from a multicentre Italian case–control study (Polesel et al, 2014), where information was also available on age at diabetes diagnosis.
Materials and methods
Study participants and data collection
Between 2003 and 2014, we conducted a case–control study on bladder cancer within an established Italian network of collaborating centres, including Aviano and Milan in northern Italy, and Naples and Catania in southern Italy (Polesel et al, 2014). Cases were 690 subjects (median age 67 years; range 25–84 years) with incident transitional cell carcinoma of the bladder admitted to major general hospitals in the study areas. Nearly all bladder cancers (n=642, 93.0%) were confirmed by histological testing on tumour tissue specimen from biopsy or surgery and three additional cases were confirmed by cytology only. Overall, 268 cancers (38.8%) were noninvasive (i.e., TNM pTis/Ta) and 351 (50.9%) locally invasive (other T); 307 (44.5%) were well or moderately differentiated (grading, G1–G2) and 312 (45.2%) poorly differentiated or undifferentiated (G3–G4). Controls were subjects admitted to the same network of hospitals as cases for a wide spectrum of acute, non-neoplastic conditions unrelated to tobacco, and alcohol consumption or long-term diet modification. The control group included 690 patients frequency-matched to cases by study centre, sex, and 5-year age group. Twenty-five controls were excluded after enrolment because of inappropriate admission diagnosis, thus leaving 665 eligible controls (median age 66 years; range 27–84 years). Overall, 28.9% of controls were admitted for traumas, 22.1% for non-traumatic orthopaedic disorders, 39.3% for acute surgical conditions, and 9.8% for miscellaneous other illnesses. All study subjects signed an informed consent, according to the recommendations of the Board of Ethics of the study hospitals.
Trained interviewers administered a structured questionnaire to cases and controls during their hospital stay. Refusal was below 5% for both cases and controls. The questionnaire collected information on sociodemographic factors, lifetime smoking and alcohol drinking habits, habitual diet before diagnosis/interview, a problem-oriented medical history, family history of cancer, lifetime occupational history, and exposure to selected chemical substances. Diagnosis of diabetes mellitus and selected other medical conditions (confirmed by a physician) was self-reported and included age at first diagnosis.
Statistical analysis
Odds ratios (OR) according to diabetes, and the corresponding 95% CI, were estimated by unconditional multiple logistic regression models (Breslow and Day, 1980), including terms for study centre, sex, quinquennia of age, year of interview, education (<7, 7–11, ⩾12 years), and tobacco smoking (never, ex-smokers, current smokers of <15, current smokers of 15–24, current smokers of ⩾25 cigarettes per day). Additional models were used to assess the potential modifying effect of selected covariates and heterogeneity was tested computing the difference in −2 log-likelihood of the models with and without the interaction terms. Percent attributable risks were computed using the distribution of risk factors among bladder cases (Bruzzi et al, 1985). All statistical analyses were performed with SAS 9.2 statistical software (SAS Institute, Cary, NC, USA).
Results
Table 1 gives the distribution of bladder cancer cases and controls according to selected variables. Cases and controls had a similar distribution by study centre, sex, and education; cases were slightly older and more frequently smokers than controls.
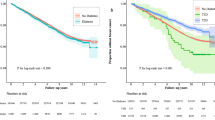
One hundred and twelve (16.2%) cases and 57 (8.6%) controls reported a diagnosis of diabetes mellitus, corresponding to a multivariate OR of 2.09 (95% CI: 1.46–3.01; Table 2). Further adjustments for body mass index (BMI), alcohol drinking, history of cystitis, and family history of bladder cancer did not meaningfully modify our results. The ORs for diabetes were similar for well/moderately differentiated (OR 2.11; 95% CI: 1.34–3.33) and poorly differentiated/not differentiated (OR 1.98; 95% CI: 1.28–3.06) bladder cancers and for noninvasive (OR 2.39; 95% CI: 1.52–3.75) or locally invasive (OR 1.75; 95% CI: 1.13–2.71) ones. Similar ORs were observed for those with a diagnosis before age 40 years (OR 2.81; 95% CI: 0.52–15.1) or at age 40 years or more (OR 2.06; 95% CI: 1.43–2.99), although the former OR was based on very few diabetic subjects (six cases and two controls). Bladder cancer risk increased with duration of diabetes (OR 1.92, 95% CI: 1.06–3.48 for 1–<5 years; 1.63, 95% CI: 0.77–3.44 for 5–<10 years; 2.39, 95% CI: 1.07–5.33 for 10–<15 years; and 2.58, 95% CI: 1.32–5.03 for ⩾15 years).
The risk of bladder cancer was consistent in the strata of age and education, whereas it was somewhat lower (although not significantly) in women (OR 1.18; 95% CI: 0.39–3.63) compared with that in men (OR 2.29; 95% CI: 1.55–3.39), in never (OR 1.31; 95% CI: 0.56–3.06) and current (OR 1.42; 95% CI: 0.68–2.97) smokers compared with that in ex-smokers (OR 2.89; 95% CI: 1.75–4.76), and in subjects with a BMI <25 kg m−2 (OR 1.48; 95% CI: 0.79–2.80) compared with that in subjects with a BMI ⩾25 kg m−2 (OR 2.55; 95% CI: 1.62–4.01; data not shown in tables). In this population, 8.4% of all bladder cancers were attributable to diabetes.
Discussion
The present study provides further evidence of the importance of diabetes in bladder cancer risk, diabetics having about two-fold excess risk as compared with non-diabetics. A duration-risk relationship was also observed, which supports a causal role of diabetes on this neoplasm.
The RR of bladder cancer found in our study is somewhat higher than the overall risk estimates reported in some meta-analyses (Larsson et al, 2006; Zhu et al, 2013a, 2013b), which ranged between 1.2 and 1.5. Tobacco smoking – which is the major recognised risk factor for bladder cancer (IARC, 2004) and has been directly associated with diabetes (Willi et al, 2007) – was allowed for in the models and did not appear to confound appreciably the association between diabetes and bladder cancer risk in this dataset. However, a stronger excess risk of bladder cancer for diabetes was found in former smokers – likely subjects quitting because of cancer or other health conditions (Gallus et al, 2013) – pointing to a possible residual confounding of tobacco smoking. Overweight is a strong determinant of type 2 diabetes, although it has not been strongly associated with bladder cancer risk (Holick et al, 2007; World Cancer Research Fund and American Institute for Cancer Research, 2007), and thus cannot explain the association found with diabetes. In our study, the association with diabetes was apparently, although not significantly, stronger in overweight subjects compared to those with regular weight. In any case, adjustment for BMI did not meaningfully modify our risk estimates. As reported previously (Zhu et al, 2013a, 2013b), the association between diabetes and bladder cancer was apparently stronger in men compared with that in women, but this may be because of chance, giving the low number of diabetic women in our study.
In our study, we were able to analyse the relation with duration of diabetes, which has been examined in a limited number of studies. Consistently with previous studies (MacKenzie et al, 2011; Newton et al, 2013; Prizment et al, 2013), we found that the excess risk of bladder cancer increases with duration of diabetes, although a few other investigations reported no consistent trend in risk (Atchison et al, 2011; Tseng, 2011).
The possible mechanisms explaining the association between diabetes and bladder cancer are unclear. Insulin resistance and hyperinsulinaemia, which characterise diabetes, have been shown to stimulate tumour growth by increasing insulin-like growth factor-1 levels, which in turn may stimulate cell proliferation and inhibit apoptosis (Zhao et al, 2003; Vigneri et al, 2009). Alternatively, diabetes increases the risk of urinary tract infections (Chen et al, 2009), which are directly associated with bladder cancer risk (La Vecchia et al, 1991; Michaud, 2007).
Cases and controls in the present study came from comparable catchment areas, were interviewed by uniformly trained interviewers in their hospital settings, had an almost complete participation rate, and were unaware of any particular hypothesis relating diabetes to bladder cancer, thereby reducing the likelihood of potential selection and recall bias. Diagnosis of diabetes and other medical conditions was self-reported and we had no measure of HbA1c levels for diabetic patients, thus some misclassification is possible. However, reliability of information on diabetes provided by hospital controls has been shown to be satisfactory in this network of studies (Bosetti et al, 2001). Although hospital controls may not be representative of the general population, the prevalence of diabetes among our controls was consistent with estimates from national population-based surveys (Asciutto et al, 2014; National Institute of Health). We were also able to allow for major confounding factors for bladder cancer, including, in particular, careful allowance for tobacco. A further limitation of this study is the lack of information on drugs used for diabetes control, which have been shown to have variable effects on bladder cancer risk (Soranna et al, 2012; Bosetti et al, 2013b). Moreover, we could not distinguish between type 1 and type 2 diabetes, although most (95%) of our subjects had a diagnosis after age 40 years, thus being likely affected by type 2 diabetes mellitus.
In conclusion, our data support a role of diabetes in bladder cancer aetiology, although some residual confounding by tobacco smoking, BMI, or other unmeasured covariates may partly explain the association observed.
Change history
30 June 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Asciutto R, Lugo A, Gallus S, Roncaglioni M, La Vecchia C, Bosetti C (2014) Prevalence and determinants of diabetes mellitus in a representative sample of Italian adults. Epidemiol Biostat Public Health 11: e9980.9981–e9980.9988.
Atchison EA, Gridley G, Carreon JD, Leitzmann MF, McGlynn KA (2011) Risk of cancer in a large cohort of U.S. veterans with diabetes. Int J Cancer 128: 635–643.
Bosetti C, Bertuccio P, Malvezzi M, Levi F, Chatenoud L, Negri E, La Vecchia C (2013a) Cancer mortality in Europe, 2005–2009, and an overview of trends since 1980. Ann Oncol 24: 2657–2671.
Bosetti C, Rosato V, Buniato D, Zambon A, La Vecchia C, Corrao G (2013b) Cancer risk for patients using thiazolidinediones for type 2 diabetes: a meta-analysis. Oncologist 18: 148–156.
Bosetti C, Tavani A, Negri E, Trichopoulos D, La Vecchia C (2001) Reliability of data on medical conditions, menstrual and reproductive history provided by hospital controls. J Clin Epidemiol 54: 902–906.
Breslow NE, Day NE (1980) Statistical Methods in Cancer Research. Vol. I. The Analysis of Case–Control Studies IARC Sci Publ No. 32 IARC: Lyon, France.
Bruzzi P, Green SB, Byar DP, Brinton LA, Schairer C (1985) Estimating the population attributable risk for multiple risk factors using case–control data. Am J Epidemiol 122: 904–914.
Cantiello F, Cicione A, Salonia A, Autorino R, De Nunzio C, Briganti A, Gandaglia G, Dell'Oglio P, Capogrosso P, Damiano R (2015) Association between metabolic syndrome, obesity, diabetes mellitus and oncological outcomes of bladder cancer: a systematic review. Int J Urol 22: 22–32.
Chen SL, Jackson SL, Boyko EJ (2009) Diabetes mellitus and urinary tract infection: epidemiology, pathogenesis and proposed studies in animal models. J Urol 182: S51–S56.
Ferlay J, Soerjomataram I, Ervik M, Dikshit RP, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2013) GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide IARC CancerBase No. 11 [Internet] International Agency for Research on Cancer: Lyon, France, Available at http://globocan.iarc.fr (last accessed on 10 June 2014).
Gallus S, Muttarak R, Franchi M, Pacifici R, Colombo P, Boffetta P, Leon ME, La Vecchia C (2013) Why do smokers quit? Eur J Cancer Prev 22: 96–101.
Holick CN, Giovannucci EL, Stampfer MJ, Michaud DS (2007) Prospective study of body mass index, height, physical activity and incidence of bladder cancer in US men and women. Int J Cancer 120: 140–146.
IARC (2004) IARC Monographs on the Evaluation of the Carcinogenic Risks to Humans. Vol. 83. Tobacco Smoke and Involuntary Smoking. IARC: Lyon, France.
La Vecchia C, Negri E, D'Avanzo B, Savoldelli R, Franceschi S (1991) Genital and urinary tract diseases and bladder cancer. Cancer Res 51: 629–631.
Larsson SC, Orsini N, Brismar K, Wolk A (2006) Diabetes mellitus and risk of bladder cancer: a meta-analysis. Diabetologia 49: 2819–2823.
Letasiova S, Medve'ova A, Sovcikova A, Dusinska M, Volkovova K, Mosoiu C, Bartonova A (2012) Bladder cancer, a review of the environmental risk factors. Environ Health 11 (Suppl 1): S11.
MacKenzie T, Zens MS, Ferrara A, Schned A, Karagas MR (2011) Diabetes and risk of bladder cancer: evidence from a case–control study in New England. Cancer 117: 1552–1556.
Michaud DS (2007) Chronic inflammation and bladder cancer. Urol Oncol 25: 260–268.
National Institute of Health Rapporto nazionale Passi 2012: diabete. Available at http://www.epicentro.iss.it/passi/rapporto2012/diabete.asp (last accessed 15 April 2014).
Newton CC, Gapstur SM, Campbell PT, Jacobs EJ (2013) Type 2 diabetes mellitus, insulin-use and risk of bladder cancer in a large cohort study. Int J Cancer 132: 2186–2191.
Polesel J, Bosetti C, di Maso M, Montella M, Libra M, Garbeglio A, Zucchetto A, Turati F, Talamini R, La Vecchia C, Serraino D (2014) Duration and intensity of tobacco smoking and the risk of papillary and non-papillary transitional cell carcinoma of the bladder. Cancer Causes Control 25: 1151–1158.
Prizment AE, Anderson KE, Yuan JM, Folsom AR (2013) Diabetes and risk of bladder cancer among postmenopausal women in the Iowa Women’s Health Study. Cancer Causes Control 24: 603–608.
Renehan A, Smith U, Kirkman MS (2010) Linking diabetes and cancer: a consensus on complexity. Lancet 375: 2201–2202.
Silverman D, Devesa S, Moore L, Rothman N (2006) Bladder cancer. In: Cancer Epidemiology and PreventionD Schottenfeld, JF Fraumeni, (eds), pp 1101–1127. Oxford University Press: Oxford, UK.
Soranna D, Scotti L, Zambon A, Bosetti C, Grassi G, Catapano A, La Vecchia C, Mancia G, Corrao G (2012) Cancer risk associated with use of metformin and sulfonylurea in type 2 diabetes: a meta-analysis. Oncologist 17: 813–822.
Tseng CH (2011) Diabetes and risk of bladder cancer: a study using the National Health Insurance database in Taiwan. Diabetologia 54: 2009–2015.
Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R (2009) Diabetes and cancer. Endocr Relat Cancer 16: 1103–1123.
Villanueva CM, Cantor KP, Cordier S, Jaakkola JJ, King WD, Lynch CF, Porru S, Kogevinas M (2004) Disinfection byproducts and bladder cancer: a pooled analysis. Epidemiology 15: 357–367.
Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J (2007) Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 298: 2654–2664.
World Cancer Research Fund and American Institute for Cancer Research (2007) Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective. American Institute for Cancer Research: Washington, DC, USA.
Zeegers MP, Tan FE, Dorant E, van Den Brandt PA (2000) The impact of characteristics of cigarette smoking on urinary tract cancer risk: a meta-analysis of epidemiologic studies. Cancer 89: 630–639.
Zhao H, Grossman HB, Spitz MR, Lerner SP, Zhang K, Wu X (2003) Plasma levels of insulin-like growth factor-1 and binding protein-3, and their association with bladder cancer risk. J Urol 169: 714–717.
Zhu Z, Wang X, Shen Z, Lu Y, Zhong S, Xu C (2013a) Risk of bladder cancer in patients with diabetes mellitus: an updated meta-analysis of 36 observational studies. BMC Cancer 13: 310.
Zhu Z, Zhang X, Shen Z, Zhong S, Wang X, Lu Y, Xu C (2013b) Diabetes mellitus and risk of bladder cancer: a meta-analysis of cohort studies. PLoS One 8: e56662.
Acknowledgements
This work was partially supported by the Italian Association for Research on Cancer (AIRC, Grant No. 13203) and by the Italian Ministry of Health, General Directorat of European and International Relations. F Turati was supported by a fellowship from the Italian Foundation for Cancer Research (FIRC). M Di Maso was supported by a grant from Fondazione Umberto Veronesi, Italy. We thank Mrs Ivana Garimoldi for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Turati, F., Polesel, J., Di Maso, M. et al. Diabetes mellitus and the risk of bladder cancer: an Italian case–control study. Br J Cancer 113, 127–130 (2015). https://doi.org/10.1038/bjc.2015.178
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.178
Keywords
This article is cited by
-
Long-term ambient hydrocarbon exposure and incidence of urinary bladder cancer
Scientific Reports (2022)
-
Prognostic Value of Progranulin in Patients with Colorectal Cancer Treated with Curative Resection
Pathology & Oncology Research (2020)
-
Flavonoids and bladder cancer risk
Cancer Causes & Control (2019)