Abstract
Background:
This study aimed to determine whether the BRCA1 haplotype was associated with trabectedin efficacy in soft-tissue sarcoma (STS) patients.
Methods:
We analysed BRCA1 single-nucleotide polymorphisms (SNPs) in tumour specimens from 135 advanced STS patients enrolled in published phase 2 trials or in a compassionate-use programme of trabectedin. Forty-four advanced STS patients treated with doxorubicin and 85 patients with localised STS served as controls. The 6-month nonprogression rate and overall survival (OS) were analysed according to BRCA1 haplotype using log-rank tests.
Results:
A favourable BRCA1 haplotype (presence of at least one AAAG allele) was significantly associated with an improved 6-month nonprogression rate. It was the only variable significantly associated with OS. No correlations were found between outcomes for patients with localised or advanced STS treated with doxorubicin.
Conclusions:
The BRCA1 haplotype represents a potential DNA repair biomarker that can be used for the prediction of response to trabectedin in STS patients.
Similar content being viewed by others
Main
Trabectedin is approved in Europe for the treatment of patients with advanced soft-tissue sarcoma (STS) after failure of anthracyclines and ifosfamide, or when they are not eligible to receive these agents. In this setting, the 6-month progression-free rate is about 35–40% (Garcia-Carbonero et al, 2004; Yovine et al, 2004; Le Cesne et al, 2005; Demetri et al, 2009; Blay et al, 2013).The identification of predictive biomarkers of the clinical benefit of trabectedin in STS patients is thus a crucial issue to identify potential responders.
Even though the exact action mechanisms of trabectedin are not yet fully known, previous in vitro studies have demonstrated that the action depends on the status of both nucleotide excision repair and homologous recombination (HR) DNA repair pathways (Damia et al, 2001; Erba et al, 2001; Takebayashi et al, 2001; Herrero et al, 2006; Soares et al, 2007). It was shown that cells deficient in HR were more sensitive to trabectedin than their nondeficient counterparts owing to the persistence of DNA lesions and increased formation of double-strand breaks (DSBs) (Soares et al, 2007). BRCA1, a key regulator involved in DNA-end resection during HR (Huen et al, 2010), was part of the gene expression signature, associated with sensitivity to trabectedin in human sarcoma cells explanted from patients not previously treated by chemotherapy (Martinez et al, 2005). Consistent with other publications (Schoffski et al, 2011), we have reported that the expression of ERCC1 and ERCC5 genes may be associated with clinical benefits of trabectedin (Italiano et al, 2011). However, the identification of a genomic DNA-based signature would be more adapted to routine practice than biomarkers including RNA expression data. RNA is less stable than DNA and consensual definition of cut-off levels for low or high expression is challenging. We have previously shown preliminary data from 44 patients suggesting that a specific BRCA1 haplotype composed of four single-nucleotide polymorphisms (SNPs) may be associated with clinical benefit of trabectedin in STS patients (Italiano et al, 2011). We report here a larger study exploring the predictive value of such a DNA-based biomarker.
Materials and methods
Patients
This study included four cohorts of consenting patients, with advanced STS treated between 1999 and 2012.
-
Cohort 1 (Table 1): a cohort of 135 patients treated with trabectedin as part of two published phase 2 trials (Le Cesne et al, 2005; Demetri et al, 2009) or during a compassionate-use programme open to patients with all types of STS who had failed conventional chemotherapy for advanced disease (Blay et al, 2013).
Table 1 Patient characteristics (n=135) -
Cohort 2 (Supplementary Table 1): a cohort of 44 patients with advanced STS treated with an anthracycline-based chemotherapy. This cohort was used as an independent control cohort in order to validate the specific predictive value of the BRCA1 haplotype for trabectedin response.
-
Cohort 3 (Supplementary Table 2): an independent cohort of 85 patients with localised STS treated with surgery and adjuvant radiotherapy that was used to explore an intrinsic prognostic value of BRCA1 haplotype.
-
Cohort 4: a validation cohort of 11 patients that was used to explore the feasibility of BRCA1 haplotype testing from blood samples by comparing the constitutional and the tumour BRCA1 haplotypes of consenting patients for whom blood and tumour samples were available.
The design of this study was exploratory. Therefore, no sample size calculation was performed and the inclusion of patients was based on availability of tumour material and/or blood for molecular experiments. This study was approved by the institutional review board (IRB) of each participating institution. All patients provided informed consent.
Treatment and response assessment
Trabectedin was given to cohort 1 patients as previously described at a dose of 1.3–1.5 mg m−2 in the majority of cases with either a 3-h infusion or a 24-h continuous infusion schedule (Garcia-Carbonero et al, 2004; Le Cesne et al, 2005; Demetri et al, 2009). Tumour assessment (by computed tomography or magnetic resonance imaging) was usually performed every 8 weeks for all patients using the Response Evaluation Criteria in Solid Tumors (RECIST) 1.0 (Therasse et al, 2000).
Genotyping of BRCA1 SNPs
Genomic DNA was extracted from paraffin-embedded tissues according to previously published procedures (Italiano et al, 2011). For Holland Bouin-fixed tissues, sections were washed with lithium carbonate to remove picric acid. Tissues were then washed with 1 × TNE (10 mM Tris, pH 8; 1 mM EDTA, pH 8; and 100 mM NaCl). DNA was then purified on GFX columns (GE Healthcare Europe GmbH, Saclay, France) following digestion with proteinase K (2 mgml−1, 55 °C for at least 2 h).
For the first cohort, genotyping of the four BRCA1 SNPs (Gly742Glu, rs16941; Arg1183Lys, rs16942; Gly1613Ser, rs1799966 and Pro871Leu, and rs799917) was carried out using the GoldenGate technology from Illumina (San Diego, CA, USA) on the BeadArray platform following the manufacturer’s recommendations using 150 ng of genomic DNA per patient as starting material. Raw hybridisation intensity data processing, clustering, and genotype calling were carried out using the genotyping module in the GenomeStudio package (Illumina).
BRCA1 SNP genotyping was also carried out via pyrosequencing. Briefly, 100 ng of genomic DNA were amplified with specific primers. Pyrosequencing primers were designed using the Pyrosequencing SNP Primer Design (V 1.01) software (Qiagen, Courtaboeuf, France). For PCR, 10 pmol of each primer (forward 5′-biotinylated: 5′-CACCACTTTTTCCCATCAAGTC-3′, reverse primer: 5′-TGGCCCTCTGTTTCTACCTAGTT-3′, for rs16941;forward: 5′-AGCCTATGGGAAGTAGTCATGC-3′, reverse 5′-biotinylated primer: 5′ GCCAAATGTGTATGGGTGAAAG-3′, for rs16942; forward 5′-biotinylated: 5′-TGGCAACATACCATCTTCAACC-3′, reverse: 5′-GGCTTCTCCCTGCTCACACTTT-3′ for rs179966; forward: 5′-AAGGTTTCAAAGCGCCAGTC-3′, reverse 5′-biotinylated: 5′-CTCTTCTGCATTTCCTGGATTTGA-3′ for rs 799 917) were used. The reaction was completed in a buffer containing 3 mM MgCl2 and 0.5 U Taq polymerase Platinum (Invitrogen, Cergy Pontoise, France) in a 50 μl final volume. The mixture was denatured for 5 min at 95 °C and then 50 cycles were carried out: 30 s at 95 °C, 30 s at 60 °C, or 62 °C; and 30 s at 72 °C for rs16941 and rs16942, or rs179966 and rs799917, respectively. For pyrosequencing, ssDNA was prepared from 40 μl of biotinylated PCR product using streptavidin-coated sepharose beads (GE Healthcare), and 0.37 μ M of the adequate sequencing probe (5′-CATTAATATTGCTTGAGCTG-3′ for rs16941, 5′-GCAAAAGCGTCCAGA-3′ for rs16942, 5′-GAGCAGCAGCTGGAC-3′ for rs179966 and 5′-CGCCAGTCATTTGCTC-3′ for rs799917) for analysis. Sequencing was performed with the SNP Gold reagent kit (Qiagen) according to the manufacturer’s instructions.
For BRCA1, haplotypes and frequency estimation were obtained using the Haploview software (Barrett et al, 2005). DNA extractions and SNP determination were centralised at the INSERM U916 research laboratory.
Statistical analyses
The statistical analyses on baseline demographics and clinical outcomes are based on all data available up to the cut-off date of 31 December 2013. Descriptive statistics were used to show the distribution of variables in the population. The 6-month nonprogression rate (clinical benefit rate, CBR) was defined as the number of patients whose tumours did not progress according to RECIST criteria during the first 6 months. Patients who died within 6 months of treatment onset were considered as events (progressive disease).
Progression-free survival (PFS) was defined as the interval between the date of the first cycle of chemotherapy (cohorts 1 and 2) and the time of progression according to RECIST criteria, death or last follow-up. Overall survival was defined as the interval between the date of the first cycle of chemotherapy (cohorts 1 and 2) or surgery (cohort 3), and the time of death or last follow-up. Overall survival rates were estimated with the Kaplan–Meier method and compared using the log-rank test. Univariate analyses of the association between OS and tumour characteristics included the following variables: age (<52/⩾52), gender, grade (⩽2/3), histological subtype (liposarcoma or leiomyosarcoma/ other), number of metastatic sites (⩽1/⩾2), and BRCA1 haplotype (at least one AAG allele/no AAG allele).
Pearson's correlation coefficient was used to assess the relationship between germline and tumour BRCA1 haplotype (r=1, perfect correlation). Analyses were performed using SPSS 19.0 statistical software (IPSS Inc., Chicago, IL, USA). All statistical tests were two sided, and P<0.05 was considered as statistically significant.
Results
Patients and treatment
The main study population included 135 patients. Their characteristics are described in Table 1. A total of 704 trabectedin cycles were administered. The median number of cycles per patient was three (range: 1–23).
BRCA1 status
Among the 12 possible haplotypes, two (AAAG and GGGA) haplotypes covered ∼90% of the population (48.8% and 35.9%, respectively). Other haplotypes represented ∼10%. Patients were categorised into two subgroups based on the presence of the most frequent haplotype (AAAG): patients with at least one AAAG allele (n=99) and patients with no AAAG allele (n=36).
Survival
The median follow-up was 32.7 months (range 24.7–40.4). One complete response, 16 partial responses, and 28 disease stabilisations lasting >6 months were observed. The 6-month nonprogression rate (CBR) was 33.5%. At the time of analysis, 106 patients had died and 29 were still alive. Median OS was 12.2 months (95% confidence interval (CI): 9.3–15.1). Six-month and 1-year OS rates were 65.4% (95% CI: 62–68) and 51.3% (95% CI: 48.4–54.2), respectively (Figure 1).
Clinical benefit rate and survival according to BRCA1 haplotype—subgroup analyses
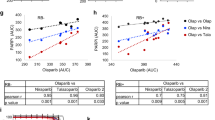
At 33.7%, the 6-month CBR rate was significantly higher in the group of patients with at least one AAAG allele vs 13.0% in patients with no AAAG allele, P=0.01. The same trend was observed for PFS (log-rank Mantel-Cox: P= 0.056) and OS (log-rank Mantel-Cox: P=0.01) (Figure 1). We did not find any differences between 6-month CBRs for anthracycline-treated patients (34.5% in the group of patients with at least one AAAG allele vs. 50%, P=0.3), PFS (log-rank Mantel-Cox: P= 0.46), or OS (log-rank Mantel-Cox: P= 0.78) (Figure 2). We did not find any differences between outcomes in patients with localised STS managed with surgery plus radiotherapy according to BRCA1 haplotype (log-rank Mantel-Cox: P= 0.34) (Figure 2).
Factors associated with OS
On univariate analysis, BRCA1 haplotype was the only variable significantly associated with OS (Table 2, Figure 1).
Correlation between somatic and constitutional BRCA1 haplotype
The comparison of the constitutional and tumour BRCA1 haplotype in 11 patients with available blood and tumour samples showed a similar status in all cases (10 cases with at least 1 AAAG allele, 1 case with no AAAG allele) (Pearson correlation coefficient r=1, P<0.0001).
Discussion
The BRCA1 protein has a crucial role in DNA repair. It is not only essential for the repair of DSBs by homologous recombination, but it also allows cells to sense such lesions (Murphy and Moynahan, 2010).
Our study indicates a link between the BRCA1 genotype and outcomes of sarcoma patients treated with trabectedin. Previous studies have mainly addressed the impact of BRCA1 mutations on cell sensitivity to platinum compounds and have found that such alterations were associated with tumour sensitivity, probably because of reduced BRCA1 activity (Chappuis et al, 2002; Cass et al, 2003; Goffin et al, 2003; Kirova et al, 2005). Analyses of several BRCA1 SNPs have also identified haplotypes that may be associated with clinical outcomes in patients with gastric or lung cancer treated with platinum-based chemotherapies (Kim et al, 2008; Shim et al, 2010). BRCA1 SNPs, whether they lead to amino-acid changes or not, may have a functional impact via several mechanisms. They could modify BRCA1 protein function or stability, or they could alter BRCA1 expression by acting on transcription, splicing, or translation. Whether the specific haplotype identified in our study is linked to a reduced activity of BRCA1 in HR or altered expression remains to be investigated. However, our results indirectly support the role of HR in trabectedin-induced cytotoxicity.
Our study has methodological strengths that compensate at least in part the potential bias related to its retrospective nature. A predictive factor is a clinical or biological characteristic that provides information on the likely benefit from treatment (either in terms of tumour shrinkage or survival). Such predictive factors can be used to identify subpopulations of patients who are most likely to benefit from a given therapy. In contrast, a prognostic factor is a clinical or biological characteristic that is objectively measurable and that provides information on the likely outcome of the cancer in an untreated individual. Such prognostic markers are helpful for identifying patients with cancer who are at high risk of metastatic relapse and therefore potential candidates for adjuvant systemic treatments. Importantly, prognostic factors define the effects of patient or tumour characteristics on the patient outcome, whereas predictive factors define the effect of treatment on the tumour. By analysing an independent series of patients with localised STS, we have identified that the BRCA1 haplotype has no impact on survival and therefore has no intrinsic prognostic value. This is in agreement with the fact that this gene was not included in the prognostic signature we recently identified (Chibon et al, 2010). Moreover, we found that the correlation between the BRCA1 haplotype and outcome was limited to patients managed with trabectedin, as no such correlations were observed in an independent series of advanced STS patients managed with doxorubicin.
Despite the limitations mainly related to the retrospective design, our study suggests that the BRCA1 haplotype may be a predictive factor of trabectedin efficacy in STS patients. As the unfavourable haplotype is present in about 25% of patients, these results may have obvious benefits for reducing the number of STS patients who ultimately receive this expensive drug, which exposes them to risks of adverse events without associated benefit. Such a DNA-based biomarker is easily assessable in routine practice as it requires only the availability of paraffin-embedded material, and it is probably also assessable in blood samples as we found the same BRCA1 status in all cases tested (although this needs further confirmation in larger cohorts). The next step for the validation of this biomarker would be to demonstrate the predictive value of the BRCA1 haplotype for trabectedin benefit in at least one randomised controlled trial comparing a trabectedin regimen to a trabectedin-free regimen. This would represent level A evidence that could modify the current conditions of trabectedin approval in STS patients.
Change history
17 February 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Barrett JC, Fry B, Maller J, Daly MJ (2005) Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21: 263–265.
Blay JY, Italiano A, Ray-Coquard I, Le CA, Duffaud F, Rios M, Collard O, Bertucci F, Bompas E, Isambert N, Chaigneau L, Cassier P, Bui B, Decanter G, Derbel O, Coindre JM, Zintl P, Badri N, Penel N (2013) Long-term outcome and effect of maintenance therapy in patients with advanced sarcoma treated with trabectedin: an analysis of 181 patients of the French ATU compassionate use program. BMC Cancer 13: 64.
Cass I, Baldwin RL, Varkey T, Moslehi R, Narod SA, Karlan BY (2003) Improved survival in women with BRCA-associated ovarian carcinoma. Cancer 97 (9): 2187–2195.
Chappuis PO, Goffin J, Wong N, Perret C, Ghadirian P, Tonin PN, Foulkes WD (2002) A significant response to neoadjuvant chemotherapy in BRCA1/2 related breast cancer. J Med Genet 39 (8): 608–610.
Chibon F, Lagarde P, Salas S, Perot G, Brouste V, Tirode F, Lucchesi C, de RA, Kauffmann A, Bui B, Terrier P, Bonvalot S, Le CA, Vince-Ranchere D, Blay JY, Collin F, Guillou L, Leroux A, Coindre JM, Aurias A (2010) Validated prediction of clinical outcome in sarcomas and multiple types of cancer on the basis of a gene expression signature related to genome complexity. Nat Med 16 (7): 781–787.
Damia G, Silvestri S, Carrassa L, Filiberti L, Faircloth GT, Liberi G, Foiani M, D'Incalci M (2001) Unique pattern of ET-743 activity in different cellular systems with defined deficiencies in DNA-repair pathways. Int J Cancer 92 (4): 583–588.
Demetri GD, Chawla SP, von MM, Ritch P, Baker LH, Blay JY, Hande KR, Keohan ML, Samuels BL, Schuetze S, Lebedinsky C, Elsayed YA, Izquierdo MA, Gomez J, Park YC, Le CA (2009) Efficacy and safety of trabectedin in patients with advanced or metastatic liposarcoma or leiomyosarcoma after failure of prior anthracyclines and ifosfamide: results of a randomized phase II study of two different schedules. J Clin Oncol 27 (25): 4188–4196.
Erba E, Bergamaschi D, Bassano L, Damia G, Ronzoni S, Faircloth GT, D'Incalci M (2001) Ecteinascidin-743 (ET-743), a natural marine compound, with a unique mechanism of action. Eur J Cancer 37 (1): 97–105.
Garcia-Carbonero R, Supko JG, Manola J, Seiden MV, Harmon D, Ryan DP, Quigley MT, Merriam P, Canniff J, Goss G, Matulonis U, Maki RG, Lopez T, Puchalski TA, Sancho MA, Gomez J, Guzman C, Jimeno J, Demetri GD (2004) Phase II and pharmacokinetic study of ecteinascidin 743 in patients with progressive sarcomas of soft tissues refractory to chemotherapy. J Clin Oncol 22 (8): 1480–1490.
Goffin JR, Chappuis PO, Begin LR, Wong N, Brunet JS, Hamel N, Paradis AJ, Boyd J, Foulkes WD (2003) Impact of germline BRCA1 mutations and overexpression of p53 on prognosis and response to treatment following breast carcinoma: 10-year follow up data. Cancer 97 (3): 527–536.
Herrero AB, Martin-Castellanos C, Marco E, Gago F, Moreno S (2006) Cross-talk between nucleotide excision and homologous recombination DNA repair pathways in the mechanism of action of antitumor trabectedin. Cancer Res 66 (16): 8155–8162.
Huen MS, Sy SM, Chen J (2010) BRCA1 and its toolbox for the maintenance of genome integrity. Nat Rev Mol Cell Biol 11 (2): 138–148.
Italiano A, Laurand A, Laroche A, Casali P, Sanfilippo R, Le CA, Judson I, Blay JY, Ray-Coquard I, Bui B, Coindre JM, Nieto A, Tercero JC, Jimeno J, Robert J, Pourquier P (2011) ERCC5/XPG, ERCC1, and BRCA1 gene status and clinical benefit of trabectedin in patients with soft tissue sarcoma. Cancer 117 (15): 3445–3456.
Kim HT, Lee JE, Shin ES, Yoo YK, Cho JH, Yun MH, Kim YH, Kim SK, Kim HJ, Jang TW, Kwak SM, Kim CS, Ryu JS (2008) Effect of BRCA1 haplotype on survival of non-small-cell lung cancer patients treated with platinum-based chemotherapy. J Clin Oncol 26 (36): 5972–5979.
Kirova YM, Stoppa-Lyonnet D, Savignoni A, Sigal-Zafrani B, Fabre N, Fourquet A (2005) Risk of breast cancer recurrence and contralateral breast cancer in relation to BRCA1 and BRCA2 mutation status following breast-conserving surgery and radiotherapy. Eur J Cancer 41 (15): 2304–2311.
Le Cesne A, Blay JY, Judson I, Van OA, Verweij J, Radford J, Lorigan P, Rodenhuis S, Ray-Coquard I, Bonvalot S, Collin F, Jimeno J, Di PE, Van GM, Nielsen OS (2005) Phase II study of ET-743 in advanced soft tissue sarcomas: a European Organisation for the Research and Treatment of Cancer (EORTC) soft tissue and bone sarcoma group trial. J Clin Oncol 23 (3): 576–584.
Martinez N, Sanchez-Beato M, Carnero A, Moneo V, Tercero JC, Fernandez I, Navarrete M, Jimeno J, Piris MA (2005) Transcriptional signature of Ecteinascidin 743 (Yondelis, Trabectedin) in human sarcoma cells explanted from chemo-naive patients. Mol Cancer Ther 4 (5): 814–823.
Murphy CG, Moynahan ME (2010) BRCA gene structure and function in tumor suppression: a repair-centric perspective. Cancer J 16 (1): 39–47.
Schoffski P, Taron M, Jimeno J, Grosso F, Sanfilipio R, Casali PG, Le CA, Jones RL, Blay JY, Poveda A, Maki RG, Nieto A, Tercero JC, Rosell R (2011) Predictive impact of DNA repair functionality on clinical outcome of advanced sarcoma patients treated with trabectedin: a retrospective multicentric study. Eur J Cancer 47 (7): 1006–1012.
Shim HJ, Yun JY, Hwang JE, Bae WK, Cho SH, Lee JH, Kim HN, Shin MH, Kweon SS, Lee JH, Kim HJ, Chung IJ (2010) BRCA1 and XRCC1 polymorphisms associated with survival in advanced gastric cancer treated with taxane and cisplatin. Cancer Sci 101 (5): 1247–1254.
Soares DG, Escargueil AE, Poindessous V, Sarasin A, de GA, Bonatto D, Henriques JA, Larsen AK (2007) Replication and homologous recombination repair regulate DNA double-strand break formation by the antitumor alkylator ecteinascidin 743. Proc Natl Acad Sci USA 104 (32): 13062–13067.
Takebayashi Y, Pourquier P, Zimonjic DB, Nakayama K, Emmert S, Ueda T, Urasaki Y, Kanzaki A, Akiyama SI, Popescu N, Kraemer KH, Pommier Y (2001) Antiproliferative activity of ecteinascidin 743 is dependent upon transcription-coupled nucleotide-excision repair. Nat Med 7 (8): 961–966.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van GM, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92 (3): 205–216.
Yovine A, Riofrio M, Blay JY, Brain E, Alexandre J, Kahatt C, Taamma A, Jimeno J, Martin C, Salhi Y, Cvitkovic E, Misset JL (2004) Phase II study of ecteinascidin-743 in advanced pretreated soft tissue sarcoma patients. J Clin Oncol 22 (5): 890–899.
Acknowledgements
This work was supported by l’Association pour la Recherche sur le Cancer (‘Soutien à la Thérapeutique Innovante en Cancérologie’ 2012). We thank Pippa McKelvie-Sebileau of Institut Bergonié for medical editorial services.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Laroche-Clary, A., Chaire, V., Le Morvan, V. et al. BRCA1 haplotype and clinical benefit of trabectedin in soft-tissue sarcoma patients. Br J Cancer 112, 688–692 (2015). https://doi.org/10.1038/bjc.2014.624
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.624
Keywords
This article is cited by
-
Trabectedin arrests a doxorubicin-resistant PDGFRA-activated liposarcoma patient-derived orthotopic xenograft (PDOX) nude mouse model
BMC Cancer (2018)
-
Activity of trabectedin and the PARP inhibitor rucaparib in soft-tissue sarcomas
Journal of Hematology & Oncology (2017)