Abstract
Background:
A growing body of evidence suggests that diabetes is a risk factor for endometrial cancer incidence. However, most of these studies used case-control study designs and did not adjust for obesity, an established risk factor for endometrial cancer. In addition, few epidemiological studies have examined the association between diabetes treatment and endometrial cancer risk. The objective of this study was to assess the relationships among diabetes, diabetes treatment and endometrial cancer risk in postmenopausal women participating in the Women’s Health Initiative (WHI).
Methods:
A total of 88 107 postmenopausal women aged 50–79 years who were free of cancer and had no hysterectomy at baseline were followed until date of endometrial cancer diagnosis, death, hysterectomy or loss to follow-up, whichever came first. Endometrial cancers were confirmed by central medical record and pathology report review. Multivariate Cox proportional hazards regression models were used to estimate hazard ratios (HRs) (95% confidence interval (CI)) for diagnosis of diabetes and metformin treatment as risk factors for endometrial cancer.
Results:
Over a mean of 11 years of follow-up, 1241 endometrial cancers developed. In the primary analysis that focused on prevalent diabetes at enrolment, compared with women without diabetes, women with self-reported diabetes, and the subset of women with treated diabetes, had significantly higher risk of endometrial cancer without adjusting for BMI (HR=1.44, 95% CI: 1.13–1.85 for diabetes, HR=1.57, 95% CI: 1.19–2.07 for treated diabetes). However after adjusting for BMI, the associations between diabetes, diabetes treatment, diabetes duration and the risk of endometrial cancer became non-significant. Elevated risk was noted when considering combining diabetes diagnosed at baseline and during follow-up as time-dependent exposure (HR=1.31, 95% CI: 1.08–1.59) even after adjusting for BMI. No significant association was observed between metformin use and endometrial cancer risk.
Conclusions:
Our results suggest that the relationship observed in previous research between diabetes and endometrial cancer incidence may be largely confounded by body weight, although some modest independent elevated risk remains.
Similar content being viewed by others
Main
Endometrial cancer is the most common gynaecologic cancer in the US women (Fader et al, 2009; ACS, 2013), and its incidence and mortality rose between 2006–2010 (Howlader et al, 2013). Obesity is one major risk factor for endometrial cancer (Kaaks et al, 2002; Renehan et al, 2008; Crosbie et al, 2010). Other consistently reported risk factors for endometrial cancer include reproductive factors, physical inactivity and hypertension (Purdie and Green, 2001; Dossus et al, 2010). The main hypothesis that has been proposed to explain endometrial carcinogenesis is that exposure of the endometrium to excess oestrogen unopposed by progesterone increases the mitogenic activity of endometrial cells (Key and Pike, 1988). This hypothesis has been supported by epidemiologic studies showing that an increased risk of endometrial cancer is associated with use of unopposed exogenous estrogens (Smith et al, 1975; Ziel and Finkle, 1975; Grady et al, 1995; Crosbie et al, 2010).
A growing body of evidence suggests that diabetes may be another risk factor for endometrial cancer (Friberg et al, 2007b). A meta-analysis of 13 studies published in 2007 (Friberg et al, 2007b) and a more recent meta-analysis (Zhang et al, 2013) of prospective studies reported an increased risk of endometrial cancer associated with diabetes. Insulin resistance and hyperinsulinemia have also been linked to an increased risk of endometrial cancer (Gunter et al, 2008; Mu et al, 2012). Given the adverse effect of obesity on the incidence of both diabetes and endometrial cancer, it is important to adjust for obesity when examining the independent association of diabetes on endometrial cancer risk. However, among a total of eight cohort studies examining diabetes associated with incidence of endometrial cancer, only three studies (Terry et al, 1999; Anderson et al, 2001; Friberg et al, 2007a) adjusted for body mass index (BMI) with one study (Friberg et al, 2007a) reporting a significant association independent of BMI. Thus, more large prospective studies are needed to examine whether the association between diabetes and endometrial cancer is partly or largely accounted for by obesity.
Metformin is a biguanide that has been used worldwide for the management of type 2 diabetes. It improves glycemic control by enhancing insulin sensitivity (Cusi and DeFronzo, 1998). Evidence from epidemiologic, clinical and experimental research has suggested that metformin may have potential anticancer effects (Evans et al, 2005; Buzzai et al, 2007; Ben Sahra et al, 2008; Decensi et al, 2010; Noto et al, 2012). The potential role of metformin as an anti-neoplastic agent for endometrial cancer has been explored in a number of in vitro and in vivo studies (Cantrell et al, 2010; Tan et al, 2011; Xie et al, 2011; Zhang et al, 2011). However, to the best of our knowledge, there is only one case-control study examining the association between metformin treatment and endometrial cancer risk, and the findings were null (Becker et al, 2013).
In this study, we used the Women’s Health Initiative (WHI), a large, prospective cohort study, to examine the relationship among diabetes, metformin treatment and endometrial cancer risk. We tested the hypotheses that diabetes is associated with increased risk of endometrial cancer controlling for obesity and other covariates, and that metformin has a protective effect in reducing endometrial cancer risk.
Materials and methods
Women’s Health Initiative
The WHI was designed to address the major causes of morbidity and mortality in postmenopausal women (1998), including both multi-center clinical trials (CT) and an observational study (OS). Details of the scientific rationale, eligibility requirements and baseline characteristics of the participants in the WHI have been published elsewhere (Hays et al, 2003; Jackson et al, 2003; Langer et al, 2003; Ritenbaugh et al, 2003; Stefanick et al, 2003). Briefly, a total of 161 808 women ages 50–79 were recruited at 40 clinical centers throughout the United States between 1 September, 1993 and 31 December 1998. The WHI CT includes four overlapping components: two Hormone Therapy Trials (27 347 women), a Dietary Modification Trial (48 835 women) and a Calcium/Vitamin D Supplementation Trial (36 282 women). Participants in the OS included 93 676 women who were screened for the CT but were ineligible or unwilling to participate, or were recruited through a direct invitation for the OS. The study was overseen by institutional review boards at all 40 clinical centers and at the coordinating center, as well as by a study-wide data and safety-monitoring board. All participants in WHI gave informed signed consent and were followed prospectively.
The following participants were excluded from the original cohort of 161 808 for this analysis: 12 655 women who had a history of cancer (except non-melanoma skin cancer) at baseline; 792 women who joined but provided no follow-up information; 60 016 who had had a hysterectomy, 129 women who were diagnosed with diabetes before age 20 and/or who were ever hospitalised for diabetic coma (these were deemed to have a probable type 1 diabetes diagnosis); and 109 women who had missing values of the main exposures (including diagnosis of diabetes, age at diagnosis and diabetes treatment). After exclusions, 88 107 women remained for further analysis.
Measurement of exposures, outcome and confounders
Exposures
Diabetes, diabetes treatment and diabetes duration at baseline were used as primary exposures. Prevalence of diabetes at enrolment was defined by a positive answer to the question: ‘did a doctor ever say that you had sugar diabetes or high blood sugar when you were not pregnant’, or by reported use of medication to treat diabetes collected on the study medication inventory. Treated diabetes at enrolment was defined as yes or no if the participant reported ever having been treated or not for diabetes with pills or insulin shots. Information on the type of treatment for diabetes was extracted from the WHI medication inventory collected at baseline; diabetic patients were divided into three groups based on the type of drugs used currently (i.e., metformin, insulin or others). The duration of diabetes at enrolment was based on the difference between age of participants when first diagnosed with diabetes and age at enrolment.
Incidence of medically treated diabetes was also determined during annual WHI follow-up. The definition of incident diabetes was a positive response to the question: ‘since the date given on this form has a doctor prescribed any of the following pills or treatments?’, and mention of any newly prescribed pills for treating diabetes, or insulin shots, on either the semi-annual or annual follow-up questionnaires. Self-reported diabetes in WHI has been validated by medication inventories, laboratory data and chart review as a reliable indicator of diagnosed diabetes (Margolis et al, 2008; Jackson et al, 2013).
Follow-up and ascertainment of cases
Incident endometrial cancer cases were identified by self-administered questionnaires (administered every 6 months in the CT through 2005, and annually in the CT after 2005 and in the OS), with all cases confirmed by medical record review. All primary endometrial cancer cases were then coded centrally in accordance with the Surveillance Epidemiology and End Results (SEER) coding guidelines. For these analyses participants were followed to first endometrial cancer diagnosis, date of hysterectomy, date of death, loss to follow-up or end of CT or OS follow-up (30 September, 2010), whichever occurred first.
Confounders
In the multivariable models, we considered a series of potential confounders, including age at enrolment (<55, 55–59, 60–64, 65–69, 70–74, ⩾75), ethnicity (American Indian or Alaska Native, Asian or Pacific Islander, Black or African-American, Hispanic/Latino, non-Hispanic white and other), education (high school or less, some college/technical training, college or some post-college and master or higher), smoking status (never, former—including years since quitting: ⩾30, 20–29, 10–19, <10 and current–including cigarettes smoked per day: <5, 5–14, 15–24, ⩾25), recreational physical activity (total metabolic equivalent tasks (METs) per week: <5, 5—<10, 10–<20, 20–<30, ⩾30), alcohol intake (non-drinker, past drinker, <1 drink per month and current drinker—including frequency: <1 drink per month, 1 drink per month to <1 drink per week, 1–<7 drinks per week, ⩾7 drinks per week) and history of Hormone Therapy use (none, oestrogen alone, oestrogen and progestin, mixed), oral contraception use, parity (never pregnant, never had term pregnancy, 1, 2, 3, 4, ⩾5), age at menarche (<12, 12–13, 14–15, ⩾16 years); age at first live birth (never had term pregnancy,<20 years, 20–29; ⩾30 years), family history of endometrial cancer.
Indices of obesity were included in multivariate models also, to better evaluate the independent effects of the exposure on the outcome: these included body mass index (<18.5, 18.5–24.9, 25.0–29.9, 30.0–34.9, 35.0–39.9, ⩾40).
Statistical analysis
For the distribution of demographic characteristics by diabetes status, χ2 tests were used to evaluate differences for categorical covariates, and t-tests were used for continuous variables. Cox proportional hazards regression models were employed to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between diabetes and risk of endometrial cancer. In the multivariable models, we adjusted for age, ethnicity, education, smoking status, BMI, waist-to-hip ratio, alcohol consumption, physical activity, and history of Hormone Therapy use, oral contraception use, parity, age at menarche, age at first live birth and family history of endometrial cancer as described above. Different study cohorts (participation in OS or CTs, and different treatment assignments for all three clinical trials) were treated as strata in the model to take into account possible different baseline hazards in different sub-groups and treatment effects.
The effect of exposure was examined in different ways. The first set of analyses was focused on prevalent diabetes as an exposure (4247 women with prevalent diabetes), including diabetes status, treatment of diabetes and duration of prevalent diabetes at enrolment. In the second set of analyses, we considered all treated diabetes as an exposure, including prevalent and incident-treated diabetes newly occurring during WHI follow-up (10046 women had or developed diabetes). In all analyses including incident diabetes, a time-dependent covariate was generated by taking into account change in diabetes status during follow-up. That is, we considered women in the non-diabetes group until they reported diabetes.
In addition, we also performed stratified analysis by obesity. Interaction between diabetes and obesity was tested by entering cross-product terms into the multiplicative models. The proportionality assumption was satisfied for all exposure variables of interest and potential confounding variables based on graphs of scaled Schoenfeld residuals (Hess, 1995). All statistical analyses were conducted using SAS (Version 9.3, SAS Institute, Cary, NC, USA).
Results
Baseline characteristics by type 2 diabetes status at enrolment are shown in Table 1. Compared with women without diabetes, women with diabetes were more likely to be older, non-White (non-Hispanic), less educated, and have higher BMI and higher waist-to-hip ratio. They were less physically active, and were more likely to be a non-drinker, report a family history of endometrial cancer, have hypertension, have younger age at menarche, have younger age at first birth and have greater number of term pregnancies. Women with diabetes were also less likely to report a history of oral contraception use or oestrogen plus progestin hormone therapy use (all P-values <0.05). Among 4247 (4.8%) diabetic women, 39.1% were receiving no pharmacologic treatment for diabetes, 12.5% used metformin, 31.9% used other oral medications and 16.5% used insulin (Table 1).
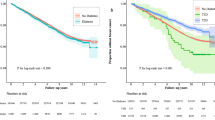
Over a mean of 11 years of follow-up, 1241 endometrial cancers developed. In the primary analysis, self-reported diabetes at enrolment was significantly associated with risk of endometrial cancer in the age-adjusted model and the multivariable-adjusted model without including BMI (Figure 1, Table 2). The association became weaker and non-significant after further adjusting for BMI in the multivariable-adjusted model (HR=1.16, 95% CI: 0.90–1.48) (Table 2). Similar results were found for women with treated diabetes, women who used metformin alone, women who received insulin and women with long duration (⩾6 years) of diabetes. These significant associations were observed only without adjusting for BMI, but not in the multivariable-adjusted model that adjusted for BMI. Similar patterns were observed in data stratified by BMI (<30 kg m−2 or ⩾30 kg m−2), but no significant association was observed for women with diabetes regardless of the type of treatment for diabetes or duration of diabetes (Table 3).
While adjusting for BMI that also attenuated the risk of endometrial cancer, it remained significantly elevated when combining treated diabetes at baseline and incident-treated diabetes diagnosed during follow-up as a time-dependent exposure (Table 4, HR=1.31, 95% CI: 1.08–1.59). Similar finding were noted regardless of the duration of diabetes and for women treated with oral medications (HR=1.33, 95% CI: 1.07–1.65). However, we did not observe significantly elevated endometrial cancer risk after adjustment for BMI in the smaller subsets of women treated with insulin, metformin or other drugs regimens. In addition, we compared endometrial cancer risk in metformin users and all non-metformin users in analyses restricted to diabetic women and found HR=1.00 (95% CI: 0.62–1.62) without adjusting for BMI and HR=0.97 (95% CI: 0.60–1.58) with adjusting for BMI in the time-dependent diabetes status model (data not shown).
We did a sensitivity analysis by excluding the first 2 years of follow-up and found that the results were similar to the primary analysis. For example, the HR for endometrial cancer was 1.44 (95% CI: 1.10–1.89) in women with prevalent diabetes without adjusting for BMI, and the HR dropped to 1.14 (95% CI: 0.87–1.49) after adjusting for BMI. We did another sensitivity analysis by restricting the analysis to endometrioid adenocarcinoma (938 cases) and found similar results as the findings when treating endometrial cancer cases as a whole (data not shown).
Discussion
In this large prospective study of postmenopausal women, our findings suggest that the relationship between diabetes and endometrial cancer incidence may be largely explained by body weight. There may, however, be a modest independent relationship between treated diabetes and endometrial cancer, as suggested by the analyses that include the larger number of cases among women with either prevalent or incident diabetes. In addition, our data did not support a protective role of metformin in endometrial cancer risk.
Obesity is an established risk factor for endometrial cancer (Kaaks et al, 2002; Renehan et al, 2008; Crosbie et al, 2010). Due to the close relation between obesity and diabetes, it is important to control for the confounding (in the sense of common cause) effect of BMI when examining the relationship between diabetes and risk of endometrial cancer. A few studies have examined the effect modification of diabetes and endometrial cancer by body weight. However, the findings of these studies have been inconsistent. A case-control study (Saltzman et al, 2008) reported that diabetes was associated with endometrial cancer among women with a BMI less than 35 kg m−2 but not among women with a BMI of 35 kg m−2 or more, while another case-control study (Lucenteforte et al, 2007) reported that the association with diabetes was stronger for obese women compared with non-obese ones. Our stratified analysis by obesity status revealed no significant association between diabetes and endometrial cancer in either the obese or non-obese group, although the patterns in both groups were similar to the overall data.
Our data indicate that the relationship between diabetes and endometrial cancer incidence may be largely confounded by body weight, but did not rule out completely some independent association between newly diagnosed diabetes and endometrial cancer. We observed non-significant increased risk of endometrial cancer associated with prevalent diabetes and significant increased risk associated with combined prevalent and incident diabetes. One explanation for the difference may be due to increased study power when using combined prevalent and incident diabetes. Another possible explanation may be related to higher level of circulating insulin (hyperinsulinemia) in a recent diagnosis of diabetes than a more distant diagnosis. This hypothesis was supported by a study (Saltzman et al, 2008) that observed a significant association between diabetes and risk of endometrial cancer only among women with a recent diabetes diagnosis (<5 years) but not among those with a more distant diagnosis, although the same finding was not observed in our data. It is biologically plausible that diagnosed diabetes is associated with endometrial cancer risk. High levels of insulin have been found to exert direct and indirect effects that contribute to the development of endometrial cancer. Insulin can promote tumorigenesis through a direct effect on epithelial tissues acting on the insulin/insulin-like growth factor family of receptors (Belfiore et al, 2009), or indirectly by affecting the levels of other modulations, such as insulin-like growth factors, sex hormones and adipokines (Pollak et al, 2004; Wolf et al, 2005).
Laboratory models provide impressive evidence for the activity of metformin in endometrial cancer treatment and chemoprevention (Cantrell et al, 2010; Zhang et al, 2011); however, results from our study along with another case-control study (Becker et al, 2013) did not support the effect of metformin in preventing the risk of endometrial cancer. Metformin is an oral biguanide commonly used for the treatment of type 2 diabetes. It has recently been demonstrated in laboratory data to possess anti-proliferative properties that can be exploited for the prevention and treatment of a variety of cancers. The proposed mechanism for the anti-neoplastic effects of metformin is by activating AMP protein kinase (AMPK) via serine/threonine kinase 11 (STK11 or LKB1). AMPK activation inhibits cellular proliferation and mRNA translation via mammalian target of rapamycin (mTOR) signalling, which may contribute to the direct anti-neoplastic effects of metformin (Shaw et al, 2005; Zakikhani et al, 2006; Williams and Brenman, 2008). Studies have reported that metformin can reverse progestin resistance in endometrial cancer cells by downregulating GloI expression (Zhang et al, 2011). Metformin was also reported to inhibit the proliferation of Ishikawa and ECC-1 endometrial cancer cell lines by activating AMPK and subsequent inhibiting of mTOR (Cantrell et al, 2010). Thus, metformin may not be effective for preventing endometrial cancer, but still might be an effective part of a cancer treatment regimen. A recent meta-analysis also found that metformin therapy improves the survival for endometrial cancer patients with concurrent diabetes (Zhang and Li, 2014).
Strengths of our study include the prospective design, detailed information on exposure, central coding of cancer diagnoses, information on obesity and inclusion of other potential confounders. However, several limitations deserve mention. First, diabetes status was based on self-report. Despite high positive and negative predictive value of self-reported diabetes in WHI, this may result in some degree of exposure misclassification, which may have led us to underestimate the strength of the association we observed. Second, patients may change their diabetes status during follow-up, which we were able to assess. They may also change their treatment plans during the course of diabetes. Classifying diabetes treatment based on the WHI current medication inventory collected at baseline would not capture these treatment changes. This kind of exposure misclassification is most likely to be non-differential, and may bias our effect toward to the null. Third, despite the relatively large number of participants, the statistical power was limited for studying the association of diabetes and endometrial cancer in sub-groups of medication treatment or stratified by obesity status. It is possible that lack of association after adjustment for BMI in the analyses limited to prevalent diabetes could be due to limited statistical power, since increasing the number of treated cases from 55–130 in the analyses that included both prevalent and incident diabetes found a positive association between diabetes and endometrial cancer risk even after adjustment for BMI.
In conclusion, our results suggest that the relationship observed in previous research between diabetes and endometrial cancer incidence may be largely attributable to the higher body weight in women with diabetes. Analyses that included women who developed diabetes during follow-up suggest that diabetes confers some modest residual risk of endometrial cancer that is independent of body weight. Nevertheless, it is important to appropriately adjust for body weight when further quantifying the magnitude of the independent association between diabetes and endometrial cancer. Our data did not support the protective effect of metformin for endometrial cancer.
Change history
23 September 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
The Women’s Health Initiative Study Group (1998) Design of the Women's Health Initiative clinical trial and observational study. Control Clin Trials 19 (1): 61–109.
ACS (2013) Cancer Facts & Figures, American Cancer Society: Atlanta, GA.
Anderson KE, Anderson E, Mink PJ, Hong CP, Kushi LH, Sellers TA, Lazovich D, Folsom AR (2001) Diabetes and endometrial cancer in the Iowa women’s health study. Cancer Epidemiol Biomarkers Prev 10 (6): 611–616.
Becker C, Jick SS, Meier CR, Bodmer M (2013) Metformin and the risk of endometrial cancer: a case-control analysis. Gynecol Oncol 129 (3): 565–569.
Belfiore A, Frasca F, Pandini G, Sciacca L, Vigneri R (2009) Insulin receptor isoforms and insulin receptor/insulin-like growth factor receptor hybrids in physiology and disease. Endocr Rev 30 (6): 586–623.
Ben Sahra I, Laurent K, Loubat A, Giorgetti-Peraldi S, Colosetti P, Auberger P, Tanti JF, Le Marchand-Brustel Y, Bost F (2008) The antidiabetic drug metformin exerts an antitumoral effect in vitro and in vivo through a decrease of cyclin D1 level. Oncogene 27 (25): 3576–3586.
Buzzai M, Jones RG, Amaravadi RK, Lum JJ, DeBerardinis RJ, Zhao F, Viollet B, Thompson CB (2007) Systemic treatment with the antidiabetic drug metformin selectively impairs p53-deficient tumor cell growth. Cancer Res 67 (14): 6745–6752.
Cantrell LA, Zhou CX, Mendivil A, Malloy KM, Gehrig PA, Bae-Jump VL (2010) Metformin is a potent inhibitor of endometrial cancer cell proliferation-implications for a novel treatment strategy. Gynecol Oncol 116 (1): 92–98.
Crosbie EJ, Zwahlen M, Kitchener HC, Egger M, Renehan AG (2010) Body mass index, hormone replacement therapy, and endometrial cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev 19 (12): 3119–3130.
Cusi K, DeFronzo RA (1998) Metformin: a review of its metabolic effects. Diabetes Rev 6 (2): 89–131.
Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, Gandini S (2010) Metformin and cancer risk in diabetic patients: a systematic review and meta-analysis. Cancer Prev Res 3 (11): 1451–1461.
Dossus L, Allen N, Kaaks R, Bakken K, Lund E, Tjonneland A, Olsen A, Overvad K, Clavel-Chapelon F, Fournier A, Chabbert-Buffet N, Boeing H, Schutze M, Trichopoulou A, Trichopoulos D, Lagiou P, Palli D, Krogh V, Tumino R, Vineis P, Mattiello A, Bueno-de-Mesquita HB, Onland-Moret NC, Peeters PH, Dumeaux V, Redondo ML, Duell E, Sanchez-Cantalejo E, Arriola L, Chirlaque MD, Ardanaz E, Manjer J, Borgquist S, Lukanova A, Lundin E, Khaw KT, Wareham N, Key T, Chajes V, Rinaldi S, Slimani N, Mouw T, Gallo V, Riboli E (2010) Reproductive risk factors and endometrial cancer: the European Prospective Investigation into Cancer and Nutrition. Int J Cancer 127 (2): 442–451.
Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD (2005) Metformin and reduced risk of cancer in diabetic patients. BMJ 330 (7503): 1304–1305.
Fader AN, Arriba LN, Frasure HE, von Gruenigen VE (2009) Endometrial cancer and obesity: epidemiology, biomarkers, prevention and survivorship. Gynecol Oncol 114 (1): 121–127.
Friberg E, Mantzoros CS, Wolk A (2007a) Diabetes and risk of endometrial cancer: a population-based prospective cohort study. Cancer Epidemiol Biomarkers Prev 16 (2): 276–280.
Friberg E, Orsini N, Mantzoros CS, Wolk A (2007b) Diabetes mellitus and risk of endometrial cancer: a meta-analysis. Diabetologia 50 (7): 1365–1374.
Grady D, Gebretsadik T, Kerlikowske K, Ernster V, Petitti D (1995) Hormone replacement therapy and endometrial cancer risk: a meta-analysis. Obstet Gynecol 85 (2): 304–313.
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Manson JE, Li JX, Harris TG, Rohan TE, Xue XN, Ho GYF, Einstein MH, Kaplan RC, Burk RD, Wylie-Rosett J, Pollak MN, Anderson G, Howard BV, Strickler HD (2008) A prospective evaluation of insulin and insulin-like growth factor-I as risk factors for endometrial cancer. Cancer Epidemiol Biomarkers Prev 17 (4): 921–929.
Hays J, Hunt JR, Hubbell FA, Anderson GL, Limacher M, Allen C, Rossouw JE (2003) The Women's Health Initiative recruitment methods and results. Ann Epidemiol 13 (9 Suppl): S18–S77.
Hess KR (1995) Graphical methods for assessing violations of the proportional hazards assumption in Cox regression. Stat Med 14 (15): 1707–1723.
Howlader N, Noone A, Krapcho M, Garshell J, Neyman N, Altekruse S, Kosary C, Yu M, Ruhl J, Tatalovich A, Cho H, Mariotto A, Levis D, Chen H, Feuer E, Cronin Ke (2013) SEER Cancer Statistics Review, 1975-2010 Vol. 2014. Bethesda MD, http://ser.cancer.gov/csr/1975_2010, based on November 2012 SEER data submission, posted to the SEER web site, April 2010: National Cancer Institute.
Jackson JM, Defor TA, Crain AL, Kerby T, Strayer L, Lewis CE, Whitlock E, Williams S, Bonds DE, Vitolins MZ, Rodabough RJ, Margolis KL (2013) Self-reported diabetes is a valid outcome in pragmatic clinical trials and observational studies. J Clin Epidemiol 66 (3): 349–350.
Jackson RD, LaCroix AZ, Cauley JA, McGowan J (2003) The Women's Health Initiative calcium-vitamin D trial: overview and baseline characteristics of participants. Ann Epidemiol 13 (9 Suppl): S98–106.
Kaaks R, Lukanova A, Kurzer MS (2002) Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol Biomarkers Prev 11 (12): 1531–1543.
Key TJA, Pike MC (1988) The dose-effect relationship between unopposed estrogens and endometrial mitotic rate—its central role in explaining and predicting endometrial cancer risk. Br J Cancer 57 (2): 205–212.
Langer RD, White E, Lewis CE, Kotchen JM, Hendrix SL, Trevisan M (2003) The Women's Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol 13 (9 Suppl): S107–S121.
Lucenteforte E, Bosetti C, Talamini R, Montella M, Zucchetto A, Pelucchi C, Franceschi S, Negri E, Levi F, La Vecchia C (2007) Diabetes and endometrial cancer: effect modification by body weight, physical activity and hypertension. Br J Cancer 97 (7): 995–998.
Margolis KL, Lihong Q, Brzyski R, Bonds DE, Howard BV, Kempainen S, Simin L, Robinson JG, Safford MM, Tinker LT, Phillips LS Women Health Initiative I (2008) Validity of diabetes self-reports in the Women’s Health Initiative: comparison with medication inventories and fasting glucose measurements. Clin Trials 5 (3): 240–247.
Mu N, Zhu Y, Wang Y, Zhang H, Xue F (2012) Insulin resistance: a significant risk factor of endometrial cancer. Gynecol Oncol 125 (3): 751–757.
Noto H, Goto A, Tsujimoto T, Noda M (2012) Cancer risk in diabetic patients treated with metformin: a systematic review and meta-analysis. PLoS One 7 (3): e33411.
Pollak MN, Schernhammer ES, Hankinson SE (2004) Insulin-like growth factors and neoplasia. Nat Rev Cancer 4 (7): 505–518.
Purdie DM, Green AC (2001) Epidemiology of endometrial cancer. Best Pract Res Clin Obstet Gynaecol 15 (3): 341–354.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371 (9612): 569–578.
Ritenbaugh C, Patterson RE, Chlebowski RT, Caan B, Fels-Tinker L, Howard B, Ockene J (2003) The Women’s Health Initiative Dietary Modification trial: overview and baseline characteristics of participants. Ann Epidemiol 13 (9 Suppl): S87–S97.
Saltzman BS, Doherty JA, Hill DA, Beresford SA, Voigt LF, Chen C, Weiss NS (2008) Diabetes and endometrial cancer: an evaluation of the modifying effects of other known risk factors. Am J Epidemiol 167 (5): 607–614.
Shaw RJ, Lamia KA, Vasquez D, Koo SH, Bardeesy N, Depinho RA, Montminy M, Cantley LC (2005) The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Science 310 (5754): 1642–1646.
Smith DC, Prentice R, Thompson DJ, Herrmann WL (1975) Association of exogenous estrogen and endometrial carcinoma. N Engl J Med 293 (23): 1164–1167.
Stefanick ML, Cochrane BB, Hsia J, Barad DH, Liu JH, Johnson SR (2003) The Women’s Health Initiative postmenopausal hormone trials: overview and baseline characteristics of participants. Ann Epidemiol 13 (9 Suppl): S78–S86.
Tan BK, Adya R, Chen J, Lehnert H, Cassia LJS, Randeva HS (2011) Metformin treatment exerts antiinvasive and antimetastatic effects in human endometrial carcinoma cells. J Clin Endocr Metab 96 (3): 808–816.
Terry P, Baron JA, Weiderpass E, Yuen J, Lichtenstein P, Nyren O (1999) Lifestyle and endometrial cancer risk: a cohort study from the Swedish Twin Registry. Int J Cancer 82 (1): 38–42.
Williams T, Brenman JE (2008) LKB1 and AMPK in cell polarity and division. Trends Cell Biol 18 (4): 193–198.
Wolf I, Sadetzki S, Catane R, Karasik A, Kaufman B (2005) Diabetes mellitus and breast cancer. Lancet Oncol 6 (2): 103–111.
Xie Y, Wang YL, Yu L, Hu Q, Ji L, Zhang Y, Liao QP (2011) Metformin promotes progesterone receptor expression via inhibition of mammalian target of rapamycin (mTOR) in endometrial cancer cells. J Steroid Biochem Mol Biol 126 (3-5): 113–120.
Zakikhani M, Dowling R, Fantus IG, Sonenberg N, Pollak M (2006) Metformin is an AMP kinase-dependent growth inhibitor for breast cancer cells. Cancer Res 66 (21): 10269–10273.
Zhang ZB, Dong LL, Sui L, Yang YX, Liu XL, Yu YH, Zhu YP, Feng YJ (2011) Metformin reverses progestin resistance in endometrial cancer cells by downregulating GloI expression. Int J Gynecol Cancer 21 (2): 213–221.
Zhang ZH, Su PY, Hao JH, Sun YH (2013) The role of preexisting diabetes mellitus on incidence and mortality of endometrial cancer: a meta-analysis of prospective cohort studies. Int J Gynecol Cancer 23 (2): 294–303.
Zhang ZJ, Li S (2014) The prognostic value of metformin for cancer patients with concurrent diabetes: a systematic review and meta-analysis. Diabetes Obes Metab e-pub ahead of print 27 February 2014 doi:10.1111/dom.12267.
Ziel HK, Finkle WD (1975) Increased risk of endometrial carcinoma among users of conjugated estrogens. New Engl J Med 293 (23): 1167–1170.
Acknowledgements
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C and HHSN271201100004C. A short list of WHI investigators appears in the appendix.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Appendix
Appendix
Short list of WHI investigators:
Program Office: Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller (National Heart, Lung, and Blood Institute, Bethesda, MD, USA).
Clinical Coordinating Center: Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg (Fred Hutchinson Cancer Research Center, Seattle, WA, USA).
Investigators and Academic Centers: JoAnn E. Manson (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA); Barbara V. Howard (MedStar Health Research Institute/Howard University, Washington, DC, USA); Marcia L. Stefanick (Stanford Prevention Research Center, Stanford, CA, USA); Rebecca Jackson (The Ohio State University, Columbus, OH, USA); Cynthia A. Thomson (University of Arizona, Tucson/Phoenix, AZ, USA); Jean Wactawski-Wende (University at Buffalo, Buffalo, NY, USA); Marian Limacher (University of Florida, Gainesville/Jacksonville, FL, USA); Robert Wallace (University of Iowa, Iowa City/Davenport, IA, USA); Lewis Kuller (University of Pittsburgh, Pittsburgh, PA, USA); Sally Shumaker (Wake Forest University School of Medicine, Winston-Salem, NC, USA).
Women’s Health Initiative Memory Study: Sally Shumaker (Wake Forest University School of Medicine, Winston-Salem, NC, USA).
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Luo, J., Beresford, S., Chen, C. et al. Association between diabetes, diabetes treatment and risk of developing endometrial cancer. Br J Cancer 111, 1432–1439 (2014). https://doi.org/10.1038/bjc.2014.407
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.407
Keywords
This article is cited by
-
Diabetes and anti-diabetic interventions and the risk of gynaecological and obstetric morbidity: an umbrella review of the literature
BMC Medicine (2023)
-
Differential Expressions of Ki-67, Bcl-2, and Apoptosis Index in Endometrial Cells of Women With and Without Type II Diabetes Mellitus and Their Correlation with Clinicopathological Variables
Reproductive Sciences (2021)
-
The effect of diabetes on the risk of endometrial Cancer: an updated a systematic review and meta-analysis
BMC Cancer (2019)
-
Cancer incidence among Finnish people with type 2 diabetes during 1989–2014
European Journal of Epidemiology (2019)
-
Diabetes mellitus and cancer incidence: the Atherosclerosis Risk in Communities (ARIC) cohort study
Journal of Diabetes & Metabolic Disorders (2019)