Abstract
Background:
Haploinsufficiency may contribute to the development of breast cancer among women with a BRCA1 mutation. Thus, interventions that enhance BRCA1 expression may represent avenues for prevention. Studies have shown that 3,3′-diindolylmethane (DIM) can upregulate BRCA1 expression in breast cancer cells. This has yet to be demonstrated in vivo.
Methods:
We conducted a study to evaluate the ability of oral DIM to upregulate BRCA1 mRNA expression in white blood cells. A total of 18 women were enroled in the study, including 13 BRCA1 mutation carriers who received 300 mg per day of Rx Balance BioResponse DIM for 4–6 weeks (intervention group) and 5 BRCA1 mutation carriers who did not take DIM (control group). BRCA1 mRNA expression was assessed at baseline and at 4–6 weeks by real-time, quantitative PCR and the relative change in BRCA1 mRNA expression (that is, ) was calculated.
Results:
The relative change in BRCA1 mRNA expression among women in the intervention group achieved borderline significance (P paired t-test=0.05). In the intervention group, BRCA1 mRNA expression increased in 10 of the participants, decreased in 2 and remained unchanged in 1 of the participants following DIM intervention (P sign test=0.02). On average, women in the intervention group experienced a 34% increase in BRCA1 mRNA expression (range −24 to 194%). There was no significant difference in the relative change in BRCA1 mRNA expression among women in the control group (P paired t-test=0.45).
Conclusions:
Under the tested conditions, oral DIM was associated with an increase in BRCA1 mRNA expression in women with a BRCA1 mutation. The possibility of mitigating the effect of an inherited deleterious BRCA1 mutation by increasing the physiologic expression of the gene and normalising protein levels represents a clinically important paradigm shift in the prevention strategies available to these high-risk women. Future studies with a larger sample size and higher doses of DIM are warranted.
Similar content being viewed by others
Main
The inheritance of a deleterious mutation in the breast cancer susceptibility gene, BRCA1, confers high lifetime risks of developing breast and ovarian cancer, estimated at 80 and 40%, respectively (Ford et al, 1994; The Breast Cancer Linkage Consortium, 1999; Robson, 2002; Thompson and Easton, 2002; Antoniou et al, 2003; Chen and Parmigiani, 2007). Women with BRCA-associated breast cancers are often diagnosed at a young age (Narod, 2010), and have elevated risks of developing contralateral (Metcalfe et al, 2011a) and ipsilateral breast cancer (Metcalfe et al, 2011b). BRCA1-associated breast cancers exhibit features of an aggressive phenotype (for example, triple negative; Da Silva and Lakhani, 2010). Genetic testing permits the identification of high-risk women before cancer; however, prevention is limited to prophylactic surgery and chemoprevention with tamoxifen (Narod, 2010; Finch et al, 2014).
The incomplete penetrance associated with a BRCA mutation suggests that non-genetic modifiers may have an important role (Narod et al, 1993; Foulkes et al, 2002; Antoniou et al, 2003; King et al, 2003). Various reproductive factors have been shown to influence the risk (Jernstrom et al, 2004; Kotsopoulos et al, 2005a); however, the role for dietary and lifestyle factors is less clear (Kotsopoulos and Narod, 2005). There is some evidence that caffeine (Nkondjock et al, 2006), selenium (Kowalska et al, 2005; Kotsopoulos et al, 2010) and weight loss in early adult life (Kotsopoulos et al, 2005b) protect against BRCA1-related breast cancer. In addition, we have recently reported possible relationships between plasma iron and antimony levels and BRCA1-associated breast cancer (Kotsopoulos et al, 2012). Cancer risk reduction options that are nonsurgical and modifiable are needed.
When identifying possible lifestyle interventions that may help in the prevention of breast cancer, it is important to consider that the mechanism underlying the predisposition is likely to be different in BRCA1 mutation carriers from that of women in the general population (Salmena and Narod, 2012). BRCA1 helps maintain genomic integrity through participating in the cellular response to DNA damage, specifically in the repair of double-stranded DNA breaks (Scott, 2004). Haploinsufficiency refers to a state in which an individual has only one functional copy of a gene due to mutation or gene loss, and thus may produce an insufficient amount of protein (Berger and Pandolfi, 2011; Berger et al, 2011; Konishi et al, 2011). Although limited, there is evidence to support that the predisposition to breast cancer among BRCA1 mutation carriers is due to haploinsufficiency associated with heterozygosity, which increases genomic instability and accelerates the mutation rate of other critical genes, including the second copy of BRCA1 (Konishi et al, 2011; Salmena and Narod, 2012). Thus, factors that might increase the cellular expression of the normal copy of the gene and thereby help normalise protein levels may mitigate against the effect of the mutation.
One dietary supplement that is thought to have potential for preventing cancer in BRCA1 mutation carriers is 3,3′-diindolylmethane (DIM), a phytochemical derived from cruciferous vegetables (Higdon et al, 2007). DIM has been found to have various cancer-protective effects, particularly for hormone-dependent cancers such as that of the breast (Higdon et al, 2007). In vitro administration of a relatively low dose of the phytochemical DIM (and its precursor indole-3-carbinol (I3C)) can significantly upregulate both the BRCA1 and BRCA2 mRNA and the protein expression in breast and prostate cancer cells (Meng et al, 2000a, 2000b, 2000c; Fan et al, 2006, 2009).
If haploinsufficiency predisposes mutation carriers to cancer development, ultimately, the ability to upregulate BRCA1 expression in female BRCA1 heterozygotes may translate into a reduced cancer risk. To date, no studies have evaluated whether or not oral administration of I3C or DIM enhances the expression of normal BRCA1 mRNA or protein in vivo. We conducted a 4–6-week dietary intervention trial to evaluate the ability of DIM, a stable metabolite of I3C, to upregulate BRCA1 mRNA expression in women with a BRCA1 mutation.
Materials and Methods
Study population
Potential study participants were identified from the Familial Breast Cancer Research Unit, Women’s College Hospital (Toronto, Ontario, Canada) and included women who were enroled in previous and ongoing clinical research protocols. Eligible subjects were healthy women with no personal history of cancer, who were not pregnant or breastfeeding and were between the ages of 25 and 65 years. Women who had taken DIM were eligible to participate if they discontinued DIM use for at least 1 month before study enrolment. We included 21 healthy BRCA1 mutation carriers (BRCA1+/−). All study subjects provided their written informed consent. This study was approved by the Women’s College Hospital research ethics board and an independent Data Safety Monitoring Board was in place during the study.
Data collection
Women were invited to participate in the study by letter. After a woman expressed interest in the study, a package consisting of a consent form and a short questionnaire about diet and lifestyle was sent to her. The research coordinator contacted the participants to arrange a preliminary clinic visit.
DIM intervention
The intervention group included 15 BRCA1 mutation carriers who were assigned to receive 300 mg per day (150 mg twice daily) of Rx Balance BioResponse DIM for 4–6 weeks provided kindly by Michael Zeligs, BioResponse, LLC, Boulder, CO, Canada. The control group consisted of six BRCA1 mutation carriers who did not take DIM. At the first clinic visit, the research coordinator assigned the BRCA1 mutation carriers to either the intervention group or control group. DIM was not randomly assigned, given that women who did not want to take the intervention were assigned to the control group. A study diary was provided to the participants in the intervention group to record information on compliance and any side effects. The research coordinator also completed a reporting form for all participants to log clinic visits, compliance with the medication and any side effects. Adverse events were reported to the Data Safety Monitoring Board at the Women’s College Hospital.
Two women in the intervention group reported adverse side effects with DIM use and withdrew from the study, thus only providing baseline blood and urine samples and one woman in the intervention group did not return for a second clinic visit. One of these subjects experienced nausea and painful menstrual cramps, whereas the other woman had an adverse reaction to the gadolinium received during MRI appointment and not due to the study intervention. One of the subjects in the control group did not complete the study. Eight of the 16 women in the intervention group reported side effects on initiation of DIM supplementation, which were of mild severity and self-limited, resolving with continued use. Side effects included loose stools, change in urine colour, headaches, decreased appetite, feeling thirsty, joint pain and abdominal pain. All adverse events were reviewed by the Data Safety Monitoring Board at the Women’s College Research Institute and deemed to be of minimal severity.
Biological sample collection
Participants were invited to come to the Familial Breast Cancer Research Unit for a 15-min visit for biological sample collection and dietary intervention assignment. All participants had a blood sample collected at baseline during the first clinic visit and an additional sample collected 4–6 weeks after the first appointment. Subjects arrived to the clinic between 9 am and 10 am after an overnight fast. Approximately 20 ml of blood was collected from the participants by venipuncture into two 10 ml EDTA-containing vials. Women were also asked to bring their first morning urine sample on ice that was collected at home. Samples were labelled, placed on ice and delivered immediately (within half an hour) to the laboratory of Dr Steven Narod (Women’s College Hospital). The blood was immediately processed for RNA extraction, and 5 ml of urine was aliquotted into two 15 ml tubes containing 10 mg of ascorbic acid and stored for future use at –80 °C in freezers, which are alarmed and continuously monitored.
BRCA1 mRNA expression
BRCA1 mRNA expression was quantified in the white blood cells of the study subjects using real-time, quantitative PCR in the laboratory of Dr Steven Narod (Women’s College Hospital) at baseline and following DIM supplementation. The LeukoLOCK Total RNA Isolation System (Ambion, Austin, TX, USA) was used for total RNA extraction from the leukocyte population according to manufacturer’s instructions. The Taqman RNA-to-CT 1 Step Kit (Applied Biosystems, Foster City, CA, USA) was used for combined reverse-transcription real-time PCR and the ABI 7500 Fast Real-Time PCR System (Applied Biosystems) was used to quantify mRNA levels. The glyceraldehyde phosphate dehydrogenase (GAPDH) gene was used as a control measuring changes in BRCA1 mRNA by the comparative CT method (ΔΔCt method). The Taqman assay IDs for BRCA1 and GADPH were Hs01556194_m1 and Hs99999905_ml, respectively (Applied Biosystems). All the samples were run in triplicate to evaluate accuracy and reproducibility. The largest coefficient of variation was <2% and the mean s.e. for the CT was 0.09 and 0.10 for BRCA1 and GADPH, respectively. Samples from the same study subject (both baseline and second visit samples) were assayed in the same batch. Data were collected by the Applied Biosystems 7500 software v2.0.6 in the form of threshold cycle number (CT) for the target gene and the endogenous control gene. The mean CT values of the three replicate runs for each sample were used for calculations. The CT values were normalised to the endogenous control gene and the corresponding ΔCT values were obtained by subtracting the mean GAPDH value from the mean BRCA1 CT value. The corresponding ΔΔCT values were obtained by subtracting the ΔCT of the mRNA sample at baseline from the ΔCT of the mRNA at the second clinic visit. The relative change in BRCA1 mRNA expression is given by , which represents the change in BRCA1 mRNA expression at the second visit compared with the baseline levels (Livak and Schmittgen, 2001).
Statistical analyses
For descriptive statistics, the t-test and χ2 test were used to test for differences in continuous (including ) and categorical variables, respectively. A paired t-test was used to compare the mean ratio of the change in BRCA1 mRNA levels at baseline versus the second clinic visit (that is, specifically the ) compared with one (which represents the ratio for no change in BRCA1 mRNA expression) in the intervention group and control group separately. A sign test was used for differences in the distribution in the number of women in the intervention group that experienced an increase versus decrease in the . A P-value of ⩽0.05 was considered statistically significant and all analyses were carried out using SAS Version 9.1 (SAS Institute, Cary, NC, USA).
Results
Table 1 shows the baseline characteristics of the 18 participants in the intervention (n=13) and control (n=5) groups who provided two blood samples. Participants in the intervention group were on average significantly younger than those in the control group (P=0.02), and thus were more likely to be premenopausal (P=0.0004). There was no significant difference with respect to the other baseline characteristics between the two groups, including current oral contraceptive use, alcohol consumption and multivitamin use.
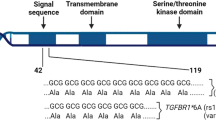
Figure 1 shows the distribution of the values among all the study participants. The relative change in BRCA1 mRNA expression among women in the intervention group achieved borderline significance (P paired t-test=0.05). In the intervention group (n=13), BRCA1 mRNA expression increased in 10 of the participants, decreased in 2 and remained unchanged in 1 of the participants following DIM intervention (P sign test=0.02). On average, these women experienced a 34% increase in BRCA1 mRNA expression (range −24 to 194%). There was no significant difference in the relative change in BRCA1 mRNA expression among women in the control group (P paired t-test=0.45). Among women in control group (n=5), BRCA1 mRNA expression decreased in two of the participants, increased in two of the participants and remained unchanged in one of the participants when comparing baseline and second visit levels with a mean increase of 15% (range −18 to 81%). There was no significant difference in the relative change in BRCA1 mRNA expression between women in the intervention group and those in the control group (P=0.43).
Relative change in BRCA1 expression normalized to GAPDH in all participants. The paired t-test used to test for the relative change in BRCA1 mRNA expression for women in the intervention group and in control group (P=0.05 and 0.45, respectively). The student’s t-test was used to test for differences in the relative change in BRCA1 mRNA expression between women in the intervention group and those in the control group (P=0.43).
There were three common mutations among the women in this study: (1) 2190delA (exon 11), (2) 185delAG (exon 2) and (3) 5382insC (exon 2). We found no significant difference in BRCA1 mRNA levels among the three (P from ANOVA=0.32; data not shown).
Discussion
The objective of this study was to evaluate the effect of a 4–6-week intervention with oral DIM on BRCA1 mRNA levels in women with an inherited BRCA1 mutation. We found that supplementation with 300 mg per day of Rx Balance BioResponse DIM for 4–6 weeks resulted in a borderline significant 34% increase in BRCA1 mRNA expression in lymphocytes from women with a BRCA1 mutation. To our knowledge, this represents the first study to demonstrate modulation, and more importantly an increase, in BRCA1 mRNA expression with a dietary intervention. This study was designed as a ‘proof of principal’ experiment to evaluate whether mRNA expression can be modified by non-genetic exposures and thus, these findings do not translate into a reduction in breast cancer risk with this level of DIM supplementation.
Cruciferous vegetables such as cauliflower, cabbage and broccoli are rich sources of glucosinolates (Higdon et al, 2007). Crushing or cooking these vegetables results in the formation of sulphur-containing isothiocyanates and indole-based I3C and DIM (Higdon et al, 2007; Ciska et al, 2009). Under the acidic environment of the stomach, I3C further dimerises to the biologically active and stable DIM and its associated oligomers, collectively referred to as acid condensation products, which are believed to be responsible for most of the biological effects associated with I3C (Shertzer and Senft, 2000). Numerous cancer-preventive properties have been associated with I3C and its derivatives, including cell cycle arrest, induction of apoptosis and modulation of oestrogen metabolism (Aggarwal and Ichikawa, 2005). Of particular relevance for BRCA1 mutation carriers is the ability of DIM to enhance BRCA1 expression (Fan et al, 2006).
In cell culture media, I3C is known to spontaneously auto-react, yielding DIM (Bradlow and Zeligs, 2010). In a series of cell culture experiments, Fan et al (2006) demonstrated that incubation of human breast cancer cells (that is, MCF-7 and T47D) with I3C significantly upregulated BRCA1 and BRCA2 mRNA and protein expression in human breast and prostate cancer cells in a dose- and time-dependent manner. The authors proposed that the induction of BRCA expression is oestrogen independent and may be via an endoplasmic reticulum stress-like pathway. This group has also shown that in vitro exposure to low doses of DIM (<0.5–1 μ M) for 72 h (rather than I3C) significantly increased BRCA1 and BRCA2 protein expressions and protects against oxidative stress (Fan et al, 2009). This dose of DIM was ∼40 times lower than that of I3C required to produce similar effects. Collectively, the findings of Fan et al provide preliminary evidence that expression of the normal BRCA1 protein may also be enhanced in BRCA1-deficient cells by exposing them to low doses of DIM. Zhang and colleagues have shown that intraperitoneal administration of DIM (10–50 mg kg−1 body weight) is able to significantly increase expression of BRCA1 in colon and cardiac tissue from mice with experimental colitis and adriamycin-induced cardiac fibrosis, respectively (Huang et al, 2011; Yao et al, 2013). This group also demonstrated a concomitant reduction in levels of oxidative stress.
Various groups (including ours) have evaluated mutagen sensitivity (as a marker of impaired cellular response to DNA damage) in fibroblasts, lymphoblastoid cell lines and peripheral blood lymphocytes of heterozygous BRCA1 (and BRCA2) mutation carriers; however, the results have been conflicting (Speit and Trenz, 2004; Kotsopoulos et al, 2007). Although limited, there is evidence to support the idea that the predisposition to breast cancer among BRCA1 mutation carriers is the haploinsufficiency associated with a heterozygosity, which increases genomic instability and accelerates the mutation rate of other critical genes, including the second copy of BRCA1 (Foray et al, 1999; Rothfuss et al, 2000; Baldeyron et al, 2002; Coupier et al, 2004; Kowalska et al, 2005; Konishi et al, 2011; Salmena and Narod, 2012). Baldeyron et al (2002) have shown that BRCA1 protein levels in lymphoblastoid cell lines established from peripheral blood lymphocytes of heterozygous BRCA1 mutation carriers were 50% lower in comparison with the normal control cell lines. Further, these heterozygous cells displayed impaired DNA end joining, a major double-strand break repair pathway in mammals. Similarly, Konishi et al (2011) have reported reduced capacity for homologous recombination-mediated DNA damage repair in human cell lines with a single mutant copy of BRCA1 derived from noncancerous human breast epithelial cells. In contrast, we and others have failed to demonstrate differences in DNA repair BRCA mutagen sensitivity using fibroblasts or lymphocytes with heterozygous mutations (Baria et al, 2001; Nieuwenhuis et al, 2002; Kotsopoulos et al, 2007; Lovelock et al, 2007).
Although some of the initial in vitro studies of I3C and BRCA expressions were conducted using I3C, the current study utilised DIM supplementation for several reasons. I3C is highly reactive and poorly absorbed as it does not leave the stomach or circulates in the bloodstream after oral administration to humans (Reed et al, 2006). In vitro studies have shown that at least 50% of I3C spontaneously dimerises to form DIM within 24 h of incubation (Bradlow and Zeligs, 2010), whereas in vivo studies have shown that following administration of I3C to humans, only DIM and not I3C is detectable in the bloodstream (Reed et al, 2006). Further, following oral administration of I3C in humans, only DIM and other non-DIM reaction products are found in the stomach (Reed et al, 2008). Thus, it is believed that DIM is the active agent and that I3C is a pro-drug that requires bioactivation in the acidic environment of the stomach (De Kruif et al, 1991).
A major limitation of our study was the quantification of BRCA1 mRNA in the genetic material derived from peripheral blood lymphocytes, which might not be representative of the breast tissue. Studies that directly quantify BRCA1 mRNA (or protein) levels in the breast before and following DIM administration are warranted. Despite this, the goal of this study was to elucidate the role of DIM in BRCA1 expression using a convenient, minimally invasive approach. Our small sample size may have precluded us from detecting a greater effect of DIM on BRCA1 expression; however, this was due to the need for immediate processing of the blood samples for RNA extraction. Nonetheless, we anticipated a substantial increase in BRCA1 mRNA with the intervention. Perhaps, the dose of DIM was not high enough or the duration of intervention was not long enough to induce a substantial change in gene expression, although this is unlikely given that this duration and dose were based on prior studies reporting plasma and tissue accumulation of DIM as well as shifts in oestrogen metabolism (Dalessandri et al, 2004; Reed et al, 2008; Heath et al, 2010; Rajoria et al, 2011), changes in gene expression (Kong et al, 2012) and activation of DNA repair (Fan et al, 2013). Pertinent to our study is that Fan et al (2009) showed increases in both BRCA1 mRNA and protein expression in cell lines exposed to ⩽0.5 μ M of DIM. This concentration of DIM corresponds to ⩽125 ng ml−1 of DIM in the human plasma, which has been achieved at lower doses of DIM (that is, ∼200 mg per day; Reed et al, 2008). Thus, the literature suggests that the dose and duration of intervention we used were adequate to induce changes in gene expression. Further, we did not have information on intake of cruciferous vegetables; however, we asked women to discontinue DIM use for at least 1 month before study enrolment. Finally, we did not evaluate the effect of DIM on a non-carrier population. Despite these limitations, strengths of the current study include the inclusion of unaffected participants with a known BRCA1 mutation status and the use of a single technician (who was blinded to the intervention group) who analysed all of the samples from the same participant in a single batch under the same conditions.
In summary, the findings from this study suggest that an intervention of 300 mg per day of Rx Balance BioResponse DIM significantly modulates BRCA1 mRNA expression in BRCA1 mutation carriers. The resultant effect on BRCA1 protein expression, and more importantly cancer risk, requires further exploration. Future studies that evaluate dietary and/or lifestyle determinants of BRCA1 expression at the gene or protein level in a large sample of BRCA1 mutation carriers may help delineate a role of non-genetic factors in the aetiology of this disease. The possibility of mitigating the effect of an inherited deleterious BRCA1 mutation by increasing the physiologic expression of the gene and normalising protein levels represents a clinically important paradigm shift in the prevention strategies available to these high-risk women.
Change history
23 September 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
The Breast Cancer Linkage Consortium (1999) Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst 91 (15): 1310–1316.
Aggarwal BB, Ichikawa H (2005) Molecular targets and anticancer potential of indole-3-carbinol and its derivatives. Cell Cycle 4 (9): 1201–1215.
Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, Hopper JL, Loman N, Olsson H, Johannsson O, Borg A, Pasini B, Radice P, Manoukian S, Eccles DM, Tang N, Olah E, Anton-Culver H, Warner E, Lubinski J, Gronwald J, Gorski B, Tulinius H, Thorlacius S, Eerola H, Nevanlinna H, Syrjakoski K, Kallioniemi OP, Thompson D, Evans C, Peto J, Lalloo F, Evans DG, Easton DF (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72 (5): 1117–1130.
Baldeyron C, Jacquemin E, Smith J, Jacquemont C, De Oliveira I, Gad S, Feunteun J, Stoppa-Lyonnet D, Papadopoulo D (2002) A single mutated BRCA1 allele leads to impaired fidelity of double strand break end-joining. Oncogene 21 (9): 1401–1410.
Baria K, Warren C, Roberts SA, West CM, Evans DG, Varley JM, Scott D (2001) Correspondence re: A. Rothfuss et al., Induced micronucleus frequencies in peripheral blood lymphocytes as a screening test for carriers of a BRCA1 mutation in breast cancer families. Cancer Res., 60: 390-394, 2000. Cancer Res 61 (15): 5948–5949.
Berger AH, Knudson AG, Pandolfi PP (2011) A continuum model for tumour suppression. Nature 476 (7359): 163–169.
Berger AH, Pandolfi PP (2011) Haplo-insufficiency: a driving force in cancer. J Pathol 223 (2): 137–146.
Bradlow HL, Zeligs MA (2010) Diindolylmethane (DIM) spontaneously forms from indole-3-carbinol (I3C) during cell culture experiments. In Vivo 24 (4): 387–391.
Chen S, Parmigiani G (2007) Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25 (11): 1329–1333.
Ciska E, Verkerk R, Honke J (2009) Effect of boiling on the content of ascorbigen, indole-3-carbinol, indole-3-acetonitrile, and 3,3′-diindolylmethane in fermented cabbage. J Agric Food Chem 57 (6): 2334–2338.
Coupier I, Baldeyron C, Rousseau A, Mosseri V, Pages-Berhouet S, Caux-Moncoutier V, Papadopoulo D, Stoppa-Lyonnet D (2004) Fidelity of DNA double-strand break repair in heterozygous cell lines harbouring BRCA1 missense mutations. Oncogene 23 (4): 914–919.
Da Silva L, Lakhani SR (2010) Pathology of hereditary breast cancer. Mod Pathol 23 (Suppl 2): S46–S51.
Dalessandri KM, Firestone GL, Fitch MD, Bradlow HL, Bjeldanes LF (2004) Pilot study: effect of 3,3′-diindolylmethane supplements on urinary hormone metabolites in postmenopausal women with a history of early-stage breast cancer. Nutr Cancer 50 (2): 161–167.
De Kruif CA, Marsman JW, Venekamp JC, Falke HE, Noordhoek J, Blaauboer BJ, Wortelboer HM (1991) Structure elucidation of acid reaction products of indole-3-carbinol: detection in vivo and enzyme induction in vitro. Chem Biol Interact 80 (3): 303–315.
Fan S, Meng Q, Auborn K, Carter T, Rosen EM (2006) BRCA1 and BRCA2 as molecular targets for phytochemicals indole-3-carbinol and genistein in breast and prostate cancer cells. Br J Cancer 94 (3): 407–426.
Fan S, Meng Q, Saha T, Sarkar FH, Rosen EM (2009) Low concentrations of diindolylmethane, a metabolite of indole-3-carbinol, protect against oxidative stress in a BRCA1-dependent manner. Cancer Res 69 (15): 6083–6091.
Fan S, Meng Q, Xu J, Jiao Y, Zhao L, Zhang X, Sarkar FH, Brown ML, Dritschilo A, Rosen EM (2013) DIM (3,3′-diindolylmethane) confers protection against ionizing radiation by a unique mechanism. Proc Natl Acad Sci USA 110 (46): 18650–18655.
Finch AP, Lubinski J, Moller P, Singer CF, Karlan B, Senter L, Rosen B, Maehle L, Ghadirian P, Cybulski C, Huzarski T, Eisen A, Foulkes WD, Kim-Sing C, Ainsworth P, Tung N, Lynch HT, Neuhausen S, Metcalfe KA, Thompson I, Murphy J, Sun P, Narod SA (2014) Impact of oophorectomy on cancer incidence and mortality in women with a BRCA1 or BRCA2 mutation. J Clin Oncol 32 (15): 1547–1553.
Foray N, Randrianarison V, Marot D, Perricaudet M, Lenoir G, Feunteun J (1999) Gamma-rays-induced death of human cells carrying mutations of BRCA1 or BRCA2. Oncogene 18 (51): 7334–7342.
Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE (1994) Risks of cancer in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Lancet 343 (8899): 692–695.
Foulkes WD, Brunet JS, Wong N, Goffin J, Chappuis PO (2002) Change in the penetrance of founder BRCA1/2 mutations? A retrospective cohort study. J Med Genet 39 (6): 407–409.
Heath EI, Heilbrun LK, Li J, Vaishampayan U, Harper F, Pemberton P, Sarkar FH (2010) A phase I dose-escalation study of oral BR-DIM (BioResponse 3,3′- Diindolylmethane) in castrate-resistant, non-metastatic prostate cancer. Am J Transl Res 2 (4): 402–411.
Higdon JV, Delage B, Williams DE, Dashwood RH (2007) Cruciferous vegetables and human cancer risk: epidemiologic evidence and mechanistic basis. Pharmacol Res 55 (3): 224–236.
Huang Z, Zuo L, Zhang Z, Liu J, Chen J, Dong L, Zhang J (2011) 3,3′-Diindolylmethane decreases VCAM-1 expression and alleviates experimental colitis via a BRCA1-dependent antioxidant pathway. Free Radic Biol Med 50 (2): 228–236.
Jernstrom H, Lubinski J, Lynch HT, Ghadirian P, Neuhausen S, Isaacs C, Weber BL, Horsman D, Rosen B, Foulkes WD, Friedman E, Gershoni-Baruch R, Ainsworth P, Daly M, Garber J, Olsson H, Sun P, Narod SA (2004) Breast-feeding and the risk of breast cancer in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 96 (14): 1094–1098.
King MC, Marks JH, Mandell JB (2003) Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302 (5645): 643–646.
Kong D, Heath E, Chen W, Cher M, Powell I, Heilbrun L, Li Y, Ali S, Sethi S, Hassan O, Hwang C, Gupta N, Chitale D, Sakr WA, Menon M, Sarkar FH (2012) Epigenetic silencing of miR-34a in human prostate cancer cells and tumor tissue specimens can be reversed by BR-DIM treatment. Am J Transl Res 4 (1): 14–23.
Konishi H, Mohseni M, Tamaki A, Garay JP, Croessmann S, Karnan S, Ota A, Wong HY, Konishi Y, Karakas B, Tahir K, Abukhdeir AM, Gustin JP, Cidado J, Wang GM, Cosgrove D, Cochran R, Jelovac D, Higgins MJ, Arena S, Hawkins L, Lauring J, Gross AL, Heaphy CM, Hosokawa Y, Gabrielson E, Meeker AK, Visvanathan K, Argani P, Bachman KE, Park BH (2011) Mutation of a single allele of the cancer susceptibility gene BRCA1 leads to genomic instability in human breast epithelial cells. Proc Natl Acad Sci USA 108 (43): 17773–17778.
Kotsopoulos J, Chen Z, Vallis KA, Poll A, Ainsworth P, Narod SA (2007) DNA repair capacity as a possible biomarker of breast cancer risk in female BRCA1 mutation carriers. Br J Cancer 96 (1): 118–125.
Kotsopoulos J, Chen Z, Vallis KA, Poll A, Ghadirian P, Kennedy G, Ainsworth P, Narod SA (2010) Toenail selenium status and DNA repair capacity among female BRCA1 mutation carriers. Cancer Causes Control 21 (5): 679–687.
Kotsopoulos J, Lubinski J, Lynch HT, Neuhausen SL, Ghadirian P, Isaacs C, Weber B, Kim-Sing C, Foulkes WD, Gershoni-Baruch R, Ainsworth P, Friedman E, Daly M, Garber JE, Karlan B, Olopade OI, Tung N, Saal HM, Eisen A, Osborne M, Olsson H, Gilchrist D, Sun P, Narod SA (2005a) Age at menarche and the risk of breast cancer in BRCA1 and BRCA2 mutation carriers. Cancer Causes Control 16 (6): 667–674.
Kotsopoulos J, Narod SA (2005) Towards a dietary prevention of hereditary breast cancer. Cancer Causes Control 16 (2): 125–138.
Kotsopoulos J, Olopado OI, Ghadirian P, Lubinski J, Lynch HT, Isaacs C, Weber B, Kim-Sing C, Ainsworth P, Foulkes WD, Eisen A, Sun P, Narod SA (2005b) Changes in body weight and the risk of breast cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res 7 (5): R833–R843.
Kotsopoulos J, Sukiennicki G, Muszynska M, Gackowski D, Kaklewski K, Durda K, Jaworska K, Huzarski T, Gronwald J, Byrski T, Ashuryk O, Debniak T, Toloczko-Grabarek A, Stawicka M, Godlewski D, Olinski R, Jakubowska A, Narod SA, Lubinski J (2012) Plasma micronutrients, trace elements, and breast cancer in BRCA1 mutation carriers: an exploratory study. Cancer Causes Control 23 (7): 1065–1074.
Kowalska E, Narod SA, Huzarski T, Zajaczek S, Huzarska J, Gorski B, Lubinski J (2005) Increased rates of chromosome breakage in BRCA1 carriers are normalized by oral selenium supplementation. Cancer Epidemiol Biomarkers Prev 14 (5): 1302–1306.
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25 (4): 402–408.
Lovelock PK, Wong EM, Sprung CN, Marsh A, Hobson K, French JD, Southey M, Sculley T, Pandeya N, Brown MA, Chenevix-Trench G, Spurdle AB, McKay MJ (2007) Prediction of BRCA1 and BRCA2 mutation status using post-irradiation assays of lymphoblastoid cell lines is compromised by inter-cell-line phenotypic variability. Breast Cancer Res Treat 104 (3): 257–266.
Meng Q, Goldberg ID, Rosen EM, Fan S (2000a) Inhibitory effects of Indole-3-carbinol on invasion and migration in human breast cancer cells. Breast Cancer Res Treat 63 (2): 147–152.
Meng Q, Qi M, Chen DZ, Yuan R, Goldberg ID, Rosen EM, Auborn K, Fan S (2000b) Suppression of breast cancer invasion and migration by indole-3-carbinol: associated with up-regulation of BRCA1 and E-cadherin/catenin complexes. J Mol Med 78 (3): 155–165.
Meng Q, Yuan F, Goldberg ID, Rosen EM, Auborn K, Fan S (2000c) Indole-3-carbinol is a negative regulator of estrogen receptor-alpha signaling in human tumor cells. J Nutr 130 (12): 2927–2931.
Metcalfe K, Gershman S, Lynch HT, Ghadirian P, Tung N, Kim-Sing C, Olopade OI, Domchek S, McLennan J, Eisen A, Foulkes WD, Rosen B, Sun P, Narod SA (2011a) Predictors of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer 104 (9): 1384–1392.
Metcalfe K, Lynch HT, Ghadirian P, Tung N, Kim-Sing C, Olopade OI, Domchek S, Eisen A, Foulkes WD, Rosen B, Vesprini D, Sun P, Narod SA (2011b) Risk of ipsilateral breast cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat 127 (1): 287–296.
Narod S, Lynch H, Conway T, Watson P, Feunteun J, Lenoir G (1993) Increasing incidence of breast cancer in family with BRCA1 mutation. Lancet 341 (8852): 1101–1102.
Narod SA (2010) BRCA mutations in the management of breast cancer: the state of the art. Nat Rev Clin Oncol 7 (12): 702–707.
Nieuwenhuis B, Van Assen-Bolt AJ, Van Waarde-Verhagen MA, Sijmons RH, Van der Hout AH, Bauch T, Streffer C, Kampinga HH (2002) BRCA1 and BRCA2 heterozygosity and repair of X-ray-induced DNA damage. Int J Radiat Biol 78 (4): 285–295.
Nkondjock A, Ghadirian P, Kotsopoulos J, Lubinski J, Lynch H, Kim-Sing C, Horsman D, Rosen B, Isaacs C, Weber B, Foulkes W, Ainsworth P, Tung N, Eisen A, Friedman E, Eng C, Sun P, Narod SA (2006) Coffee consumption and breast cancer risk among BRCA1 and BRCA2 mutation carriers. Int J Cancer 118 (1): 103–107.
Rajoria S, Suriano R, Parmar PS, Wilson YL, Megwalu U, Moscatello A, Bradlow HL, Sepkovic DW, Geliebter J, Schantz SP, Tiwari RK (2011) 3,3′-diindolylmethane modulates estrogen metabolism in patients with thyroid proliferative disease: a pilot study. Thyroid 21 (3): 299–304.
Reed GA, Arneson DW, Putnam WC, Smith HJ, Gray JC, Sullivan DK, Mayo MS, Crowell JA, Hurwitz A (2006) Single-dose and multiple-dose administration of indole-3-carbinol to women: pharmacokinetics based on 3,3′-diindolylmethane. Cancer Epidemiol Biomarkers Prev 15 (12): 2477–2481.
Reed GA, Sunega JM, Sullivan DK, Gray JC, Mayo MS, Crowell JA, Hurwitz A (2008) Single-dose pharmacokinetics and tolerability of absorption-enhanced 3,3′-diindolylmethane in healthy subjects. Cancer Epidemiol Biomarkers Prev 17 (10): 2619–2624.
Robson ME (2002) Clinical considerations in the management of individuals at risk for hereditary breast and ovarian cancer. Cancer Control 9 (6): 457–465.
Rothfuss A, Schutz P, Bochum S, Volm T, Eberhardt E, Kreienberg R, Vogel W, Speit G (2000) Induced micronucleus frequencies in peripheral lymphocytes as a screening test for carriers of a BRCA1 mutation in breast cancer families. Cancer Res 60 (2): 390–394.
Salmena L, Narod S (2012) BRCA1 haploinsufficiency: consequences for breast cancer. Womens Health (Lond Engl) 8 (2): 127–129.
Scott R (2004) DNA double strand break repair and its association with inherited predispositions to breast cancer. Hered Cancer Clin Pract 2 (1): 37–43.
Shertzer HG, Senft AP (2000) The micronutrient indole-3-carbinol: implications for disease and chemoprevention. Drug Metabol Drug Interact 17 (1–4): 159–188.
Speit G, Trenz K (2004) Chromosomal mutagen sensitivity associated with mutations in BRCA genes. Cytogenet Genome Res 104 (1–4): 325–332.
Thompson D, Easton DF (2002) Cancer Incidence in BRCA1 mutation carriers. J Natl Cancer Inst 94 (18): 1358–1365.
Yao Z, Hu W, Yin S, Huang Z, Zhu Q, Chen J, Zang Y, Dong L, Zhang J (2013) 3,3′-Diindolymethane ameliorates adriamycin-induced cardiac fibrosis via activation of a BRCA1-dependent anti-oxidant pathway. Pharmacol Res 70 (1): 139–146.
Acknowledgements
We would like to acknowledge the study coordinators Chantelle Vernon and Mitra Mohammadi who helped with the data collection and data entry. JK is the recipient of a Cancer Care Ontario Research Chair in Population Studies and a Canadian Cancer Society Career Development Award in Prevention. SAN is the recipient of a Canada Research Chair tier I. We would also like to thank MZ (Bioresponse) for providing the DIM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kotsopoulos, J., Zhang, S., Akbari, M. et al. BRCA1 mRNA levels following a 4–6-week intervention with oral 3,3′-diindolylmethane. Br J Cancer 111, 1269–1274 (2014). https://doi.org/10.1038/bjc.2014.391
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.391