Abstract
Background:
Malignant pleural mesothelioma (MPM) is an aggressive neoplasm arising from mesothelial lining of pleura. CD26 molecules preferentially expressed on epithelioid type of MPM. This study investigates the molecular mechanisms of CD26 regulating MPM cells in vitro and in vivo.
Methods:
Biochemical and cell biological approaches were used for identifying a novel molecular target of MPM. Its contribution to tumour expansion has been also assessed using animal models. The clinical samples of MPM were also assessed for its expression.
Results:
We identify that cytostatic effects in MPM are mediated by somatostatin (SST) receptor 4 (SSTR4), being inhibited by the interaction of CD26 molecules. We also indicates that SSTR4-mediated cytostatic effects are regulated by SHP-2 PTP, and that this inhibitory effect by SST agonist is enhanced via lipid raft clustering of associated molecules following crosslinking of anti-CD26 antibody. Finally, using an in vivo xenograft model, we demonstrate that the anti-tumour effect of anti-CD26 mAb is enhanced when combined with SSTR4 agonist treatment, and that SSTR4 is highly coexpressed with CD26 on epithelioid or biphasic types of MPM tissues obtained from patients’ surgical specimens.
Conclusions:
Combination therapy with humanised anti-CD26 mAb and SSTR4 agonist may therefore potentiate anti-tumour effect on MPM.
Similar content being viewed by others
Main
Malignant pleural mesothelioma (MPM) is an aggressive malignancy arising from mesothelial lining of pleura (Robinson and Lake, 2005; Shersher and Liptay, 2013). It is generally associated with a history of asbestos exposure and has a very poor prognosis (Britton, 2002; Robinson and Lake, 2005; Shersher and Liptay, 2013). In fact, the median survival is less than 12 months, with most patients dying within 10–17 months of their first symptoms (Astoul et al, 2012; Haas and Sterman, 2013; Shersher and Liptay, 2013). Once rare, the incident of MPM has increased in industrialised nations as a result of past wide spread exposure to asbestos (Myers, 2012). The incident is predicted to increase further in the next decades, especially in developing countries where asbestos has not yet been prohibited (Shersher and Liptay, 2013). Due to the lack of efficacy of conventional treatments, novel therapeutic strategies are urgently needed to improve outcomes (Astoul et al, 2012; Haas and Sterman, 2013).
CD26 is a 110-kDa, type II transmembrane glycoprotein with known dipeptidyl peptidase IV (DPPIV) (DPPIV, EC 3.4.14.5) activity in its extracellular domain and is capable of cleaving N-terminal dipeptides with either L-proline or L-alanine at the penultimate position (Ohnuma et al, 2008). CD26 has an important role in T-cell biology and overall immune function (Morimoto and Schlossman, 1998; Ohnuma et al, 2004). In addition, CD26 is expressed in various cancers and is involved in cancer biology (Havre et al, 2008). For instance, CD26 regulates topoisomerase IIα level in haematological malignancies, affecting sensitivity to doxorubicin and etoposide (Yamochi et al, 2005). Moreover, CD26 itself appears to be a novel therapeutic target, and anti-CD26 monoclonal antibody (mAb) treatment resulted in both in vitro and in vivo anti-tumour activity against several tumour types, including lymphoma and renal cell carcinoma (Ho et al, 2001; Ohnuma et al, 2002; Inamoto et al, 2006). Of note is that CD26 expression is associated with both pro- and anti-tumour effects in different cancers (Havre et al, 2008).
Previously, humanised anti-CD26 antibody inhibited growth of MPM cells and induced long-term survival of tumour-transplanted SCID mice (Inamoto et al, 2007). Recently, by analysing clinical samples, we showed that CD26 was preferentially expressed on the cell membrane of the epithelial type, but not the sarcomatoid type, of mesothelioma, while treatment outcome prediction study showed that CD26 membrane expression on MPM was closely correlated with disease responsiveness to chemotherapy (Aoe et al, 2012). Meanwhile, our in vitro studies showed that mesothelioma cells expressing high level of CD26 displayed high proliferative activity and invasiveness, and microarray analysis of CD26 knockdown and CD26-transfected mesothelioma cells showed that CD26 expression was closely linked to expression of genes contributing to cell proliferation and cell-cycle regulation (Aoe et al, 2012). More recently, we showed that nuclear localisation of CD26 molecules induced by anti-CD26 mAbs inhibited cell proliferation by modulating POLR2A transcription in MPM cells (Yamada et al, 2009, 2013). However, the nuclear translocation by mAbs occurred 30–240 min after mAb treatment, which provided inhibition of cell proliferation, but not cell motility such as migration or invasion, while the earlier signalling events in regulating cell motility via CD26 molecules remain to be elucidated. Moreover, we demonstrated that CD9 suppressed cell adhesion by inhibiting CD26–α5β1 integrin complex through its negative regulation of CD26 (Okamoto et al, 2014). These observations show that CD26 regulates the interaction of MPM cells with the extracellular matrix (ECM) via the integrin adhesion molecules. Meanwhile, with proximal signalling events associated with the cytoplasmic six amino-acid residues of CD26 being demonstrated in normal human T lymphocytes (Ohnuma et al, 2007), it is conceivable that similar CD26-mediated proximal signalling events, which remain to be clarified, have a pivotal role in MPM cell motility.
Somatostatin (SST) exhibits cytostatic effects, as treatment with SST analogue causes cell-cycle arrest in G1 or apoptosis of tumour cells in in vitro and in vivo studies (Weckbecker et al, 2003). The anti-tumour effects are mediated by a family of five G-protein-coupled SST receptors (SSTR1–5) having seven transmembrane segments, which bind the naturally occurring peptides SST-14 and SST-28 with similar affinity (Bruns et al, 1994). On the other hand, most neoplasms preferentially express SSTR2, and less frequently SSTR1, 3, 5, with SSTR4 being only rarely detected in selected tumours including neuroendocrine and prostate cancers (Reubi et al, 2001; Portela-Gomes et al, 2007; Montironi et al, 2008). However, data from the published literature on receptor expression in various tumours reveal major inconsistencies, possibly owing to the small number of tumours examined so far, as well as the use of different detection methods (Froidevaux and Eberle, 2002). Therefore, although knowledge of receptor distribution in cancer tissues is of utmost importance and has significant clinical implications, inconsistencies in the published literature regarding expression of individual receptor subtypes other than SSTR2 impede the development of novel targeted therapies.
In the current study, we extend our previous studies on high proliferative activity and invasiveness and high-expression level of CD26 by demonstrating the association between CD26 and SSTR4 with a linkage to SHP-2 PTP (phosphotyrosine phosphatase)-dependent tumour inhibition of MPM cells. Importantly, our present study is the first to report a linkage of SSTR4 in MPM cell inhibition, with implications for the treatment of MPM with SSTR4 agonist and anti-CD26 mAb, characterising the novel target molecule while concurrently suggesting a new therapeutic strategy for MPM.
Materials and methods
Cell lines and cultures
Two human MPM cell lines, H-MESO-1 (MESO1) (epithelioid) and MSTO-211 H (MSTO-P) (biphasic), and HEK293 cells were obtained from the American Type Culture Collection. JMN cells (biphasic) were a kind gift from Dr Brenda Gerwin (Laboratory of Human Carcinogenesis, National Institutes of Health, Bethesda, MD, USA). Malignant pleural mesothelioma or HEK293 cells were cultured by the methods previously described (Inamoto et al, 2007; Amatya et al, 2011). MSTO-P cells were transfected with a full-length CD26 (CD26WT) or CD26-CD10 chimaeric receptor (CD26/10Chi) subcloned retroviral shuttle plasmid pLNCX2 vector (Clontech Laboratories Inc., Mountain View, CA, USA) using the Lipofectamine2000 reagent (Life Technologies Inc., Carlsbad, CA, USA). The CD26-CD10 chimaeric receptor was composed of the N-terminal cytoplasmic region of human CD10 (1–23 amino-acid position) ligated to the transmembrane and extracellular regions of human CD26 (7–766 amino-acid position), which had been described elsewhere (Ohnuma et al, 2007). Two days after transfection of CD26WT, CD26/10Chi or mock plasmids, the cells were selected for G418 (500 μg ml−1) (Sigma-Aldrich, St Louis, MO, USA) resistance for 4 weeks. Single clone cells expressing CD26WT (MSTO-CD26WT), CD26/10Chi (MSTO-CD26/10Chi), or mock (MSTO-Mock) were then selected using a standard limiting dilution method. Luciferase-expressing cells were generated by transfection with EF1a-Luciferase (firefly)-2 A-GFP lentiviral vector (GenTarget Inc., San Diego, CA, USA). Three days after transfection, the cells were sorted for GFP-positive cells using FACSAria cell sorter (BD Biosciences, San Jose, CA, USA). Adaptation of cells to reduced serum medium was performed using a sequential adaptation method, with a conversion to 10% reduction of FBS at every three passages, leading to cells being adapted to 0.5% FBS-containing medium.
Antibodies and reagents
Anti-CD26 goat polyclonal antibody (pAb) (AF1180) was from R&D Systems (Minneapolis, MN, USA). Anti-SHP-2 rabbit pAb (C-18) and anti-transferrin receptor rabbit pAb (H-300) were from Santa Cruz Biotechnology Inc. (Dallas, TX, USA). Anti-SHP-1 rabbit pAb (07-419) was from Upsate Biotechnology (Lake Placid, NY, USA). Anti-SSTR4 rabbit pAb (AV33359), anti-FLAG M2 mouse mAb (IgG1), Peroxidase (HRP) or agarose conjugated anti-FLAG M2 mAb, and anti-β-actin mAb (AC-74) were from Sigma-Aldrich. Humanised anti-CD26 mAb (human IgG1 isotype) was generously provided by Y’s therapeutics (Tokyo, Japan). Anti-human IgG, Fcγ fragment-specific F(ab’)2 fragment (anti-Fcγ) of goat was from Jackson ImmunoResearch (West Grove, PA, USA). SHP-1/2-specific inhibitor (NSC-87877) was from Millipore (Billerica, MA, USA) and stocked in 10 mM with sterile distilled water. SSTR4-specific agonist (L-803087) was from TOCRIS Bioscience (Minneapolis, MN, USA) and stocked in 100 mM with DMSO. Cytochalasin D was from Sigma-Aldrich and stocked in 10 mM with DMSO.
Generation of deletion mutant of human SSTR4
Full-length human SSTR4 construct in pCMV6-Entry vector (SSTR4WT-FLAG) was obtained from OriGene Technologies Inc. (Rockville, MD, USA). Human SSTR4 with deleted C-terminal cytoplasmic region (SSTR4ΔC-FLAG) was made by PCR, using the forward primer (5′-gcgatcgccATGAGCGCC CCCTCGACGCTG-3′) and the reverse primer (5′-acgcgtGAGGA AGCCATAGAGAATGGGGTT-3′), and constructed into SgfI and MluI sites of pCMV6-Entry vector.
Native polyacrylamide gel electrophoresis
Membrane fraction from MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi cells was extracted with the ProteoExtract Native Membrane Protein Extraction Kit (Invitrogen Dynal AS, Oslo, Norway) according to the manufacturer’s instructions. After being precleared with normal goat Ig-crosslinked Dynabeads (VERITAS, Carlsbad, CA, USA), the native membrane extracts were immunoprecipitated with anti-CD26 pAb-crosslinked Dynabeads and eluted with the Elution Buffer of MAG2 Dynabeads Co-Immunoprecipitation Kit (Invitrogen Dynal AS). The eluates were resolved by the Blue Native polyacrylamide gel electrophoresis (PAGE) (Life Technologies Inc.). Analytical gels were stained with SilverQuest (Life Technologies Inc.). Peptide mass mapping was performed by recording peptide mass fingerprints of typical in-gel digests of the corresponding gel bands using tandem mass spectrometry (LC-MS/MS) (nano LCMS-IT-TOF; Shimadzu Biotech, Kyoto, Japan) and subsequently searching the MASCOT database (Matrix Sciences, Boston, MA, USA).
Coimmunoprecipitation, immunoblotting and lipid raft fractioning
To study the interaction between CD26 and SSTR4 using MPM cells, membrane fraction from indicated cells was extracted and coimmunoprecipitation experiments were conducted as described above. To examine the interacting domains through the use of mutant proteins, HEK293 cells were transfected with full-length human CD26, CD26-CD10 chimaeric receptor, SSTR4WT-FLAG or SSTR4ΔC-FLAG expressing plasmids, using Lipofecatmine2000 reagent. Membrane fraction was prepared as described above. After being precleared with normal mouse Ig-conjugated resin, the fractions were immunoprecipitated with anti-FLAG M2 affinity resin and eluted with FLAG peptide. The eluates in sample buffer (1% SDS, 6 M urea, 150 mM NaCl, 1 mM EDTA, 50 mM Tris (pH 8.0)) were then submitted to SDS–PAGE under reducing conditions and western blot analysis using the indicated specific antibodies. To obtain the lipid raft membrane fraction, after stimulation with control IgG or humanised anti-CD26 mAb by crosslinking with anti-Fcγ for 10 min, MSTO-CD26WT cells (each, 1 × 108) were lysed on ice with 1 ml 1% Triton X-100 and 1 mM PMSF in MNE buffer (25 mM MES (pH 6.5), 150 mM NaCl, 5 mM EDTA), followed by sucrose-gradient ultracentrifugation as described previously (Ishii et al, 2001). For immunoprecipitation of the pooled lipid raft fractions, fractionated lipid rafts (collection of fraction number 3–5) were lysed at 4 °C for 30 min with 1% N-octyl-β-D-glucoside (Nakarai Tesuque, Inc., Kyoto, Japan), and subjected to immunoprecipitation experiments, followed by SDS–PAGE and western blot analyses.
Small interference RNA
Knockdown experiments in MPM cell lines were achieved by transiently transfecting cells with the indicated specific small interference RNAs (siRNAs) or control siRNA (csi), purchased from Sigma-Aldrich. The target sequences of specific siRNA are shown in Supplementary Table. Transfection of siRNA into MPM cells was conducted using the Xfect siRNA Transfection Reagent (Takara Bio Inc., Shiga, Japan). After 48 h of transfection, cells were subjected to the corresponding experiments.
Cell migration, invasion and colony formation assays
For cell migration assay, cells (500 μl of 1 × 105 per ml in 0.1% FBS-RPMI1640) were seeded onto uncoated filters in a 24-well Transwell chamber (8-μm pore size; Costar, Corning, NY, USA) with 750 μl of FBS fresh medium in the lower cell, and allowed to migrate for 24 h at 37 °C in 100% humidifier. The cells that migrated to the underside of the filter were stained with crystal violet and images under brightfield microscopy were captured with an Olympus digital camera DP21 attached to an Olympus BX43 microscope using the CellSens software (Olympus, Tokyo, Japan). Crystal violet-stained cells were counted in five fields per filter using the ImageJ software (The National Institutes of Health). For cell invasion assay, cells (500 μl of 1 × 105 per ml in 0.1% FBS-RPMI1640) were seeded onto filters of a 24-well Transwell chamber that were coated with Matrigel (BD Biosciences) with 750 μl of FBS fresh medium in the lower cell. Invasion of the cells through the Matrigels to the underside of the filter was assessed 24 h later by staining with crystal violet and counting by the same method as in the migration assay. Soft-agar colony formation was assayed using the CytoSelect Cell Transformation Assay kit (Cell Biolabs, Inc., San Diego, CA, USA). Cells (1 × 103) were incubated 7 days in a semisolid agar medium containing the indicated antibody or reagents before being solubilised and detected by using the provided MTT solution in iMark microplate absorbance reader (absorbance at 570 nm) (Bio-Rad Laboratories, Hercules, CA, USA).
In vivo evaluation of tumour growth
Female CB17/lcr-Prkdcscid/CrlCrlj mice (SCID mice) were purchased from Charles River Laboratories Japan Inc. (Yokohama, Japan) for experimental animals and housed in a specific pathogen-free facility in micro-isolator cages. Mice were used at 8–12 weeks. SCID mice were injected i.p. with 1 × 105 luciferase-expressing MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi cells (each cohort, n=20). For in vivo bioluminescence imaging (BLI), mice were given an i.p. injection of 150 mg kg−1 body weight of D-luciferin (Wako Pure Chemical Industries, Osaka, Japan) and then anaesthetised with isoflurane gas. The mice were imaged using Caliper IVIS Lumina II In Vivo Imaging System (Perkin-Elmer, Waltham, MA, USA) to assess bioluminescence 10 min after injection of the substrate. Imaging data were analysed with the Caliper Living Image software (Perkin-Elmer) and indicated as total flux of photons per second. Mice demonstrating more than 1 × 109 photons per second or reaching end of the observation periods are euthanised.
Confocal microlaser microscopy
For detection of colocalisation between CD26 and SSTR4 in MESO1 and JMN cells, cells were preincubated in collagen-coated 8-well chamber slide glass cells (Iwaki, Tokyo, Japan), and fixed with 4% paraformaldehyde in PBS (Nakarai Tesque, Inc.). After being washed with ice-cold PBS, cells were blocked with normal goat and rabbit IgG (Santa Cruz Biotechnology Inc.), followed by incubation with Alexa Fluor 488-conjugated anti-CD26 pAb and Alexa Fluor 594-conjugated anti-SSTR4 pAb (each at a concentration of 5 μg ml−1). After being washed with ice-cold PBS, slides were mounted with Prolong Gold antifade reagent with DAPI (Molecular Probes, Eugene, OR, USA). Confocal microscopy was performed with an Olympus IX70 confocal microscope with 60 objective lenses (Olympus), using laser excitation at 496 and 568 nm. The widths of Alexa Fluor 488 and 594 emission channels were set to maximise specificity.
Tissue samples and immunohistochemistry
Fifty MPM tissues were obtained from patients who had undergone biopsy or surgery at Okayama Rosai Hospital (Okayama, Japan) or National Hospital Organization Yamaguchi-Ube Medical Center (Yamaguchi, Japan) between 1998 and 2009. Histological sections from the mesothelioma patients were previously examined and classified into epithelioid, sarcomatoid and biphasic subtypes, according to the World Health Organization histological classification by three independent pathologists (Takeshima et al, 2009), who were blinded to the results of the studies discussed in this article. Immunohistochemistry staining of 50 MPM tissues for CD26 and SSTR4 was performed and evaluated as described previously (Aoe et al, 2012).
Assessment of anti-tumour activity of SSTR4 agonist and humanised anti-CD26 mAb in mice
To assess the effect of SSTR4 agonist and humanised anti-CD26 mAb against tumorigenicity, JMN cells (1 × 106) were inoculated s.c. into the left flank of SCID mice. Mice were treated with i.p. injection of control human Ig or humanised anti-CD26 mAb (10 μg per dose) in the presence of SSTR4 agonist (20 μ M per dose) or solvent control on the seventh day after cancer cell inoculation, at a time when the tumour mass became visible (5 mm in size). Each antibody or agonist was given three times per week. Each cohort was examined with n=20. Tumours were measured every 4 days using a vernier caliper, and the volume was calculated according to the formula: 1/6 × length × square width. For assessment using systemic xenograft model, SCID mice were injected i.p. with 1 × 105 luciferase-expressing JMN cells. Mice were treated with i.p. injection of control human Ig or humanised anti-CD26 mAb (10 μg per dose) in the presence of SSTR4 agonist (20 μ M per dose) or solvent control on the next day after cancer cell inoculation. Each antibody or agonist was given three times per week. Each cohort was examined with n=20. Tumour growth was evaluated with BLI every 1 week.
Study approval
Human study protocols were approved by the Ethics Committees at Juntendo University, and at Keio University. Informed consent was obtained from all patients according to the format of the institutional review board at Okayama Rosai Hospital and National Hospital Organization Yamaguchi-Ube Medical Center. All studies on human subjects were carried out according to the principles set out in the Declaration of Helsinki. Animal experiments were conducted following protocols approved by the Animal Care and Use Committees at Juntendo University.
Statistical analysis
All experiments were performed in triplicates and repeated at least three times. Data were expressed as mean values±s.e.m. (standard error of the mean) and analysed by one-way or two-way ANOVA followed by the Tukey–Kramer post hoc test. The level of significance was P<0.05. The calculations were conducted using the Prism6.0 software (GraphPad Software, Inc., La Jolla, CA, USA).
Results
Cytoplasmic region of CD26 has an important role in tumour cell activity of MPM cells
We previously showed that CD26-mediated tumour cell proliferation of T-lymphoma and MPM cell lines was exerted via β1 integrin, in relation to the process of cell adhesion (Sato et al, 2005; Okamoto et al, 2014). Meanwhile, with the proximal signalling events associated with the cytoplasmic region of CD26 being shown in normal human T lymphocytes (Ohnuma et al, 2007), it is conceivable that similar CD26-mediated proximal events may have a role in MPM cell biology. To define the crucial role of the CD26 cytoplasmic region in regulating migratory, invasive or proliferative activity of MPM cells, we used a mutant construct of CD26 in which its cytoplasmic region was replaced with that of human CD10 (CD26-CD10 chimaeric receptor), which was shown to abrogate CD26-mediated costimulation in T cells (Ohnuma et al, 2007). CD10, as is the case with CD26, is a type II transmembrane glycoprotein with a relatively short cytoplasmic tail containing signal sequence that has an expected membrane topology similar to CD26 (Ogata et al, 1989; Maguer-Satta et al, 2011). We then transfected CD26-negative parental MSTO cells with full-length human CD26 or CD26-CD10 chimaeric receptor to establish MSTO-CD26WT or MSTO-CD26/10Chi, respectively (Supplementary Figure S1A). As shown in Figure 1A, a significant increase in migration was observed in MSTO-CD26WT as compared with MSTO-Mock (P<0.0001) or MSTO-CD26/10Chi (P<0.0001). Similarly, an increase in invasion was also observed in MSTO-CD26WT as compared with MSTO-Mock or MSTO-CD26/10Chi (Figure 1B). To study the process of tumour formation in MPM cells, we conducted colony formation assay as a model of anchorage-independent cell growth. As shown in Figure 1C, a significant increase in colony formation was observed in MSTO-CD26WT as compared with MSTO-Mock (P<0.0001) or MSTO-CD26/10Chi (P<0.0001). To extend the above in vitro results to in vivo experimentation, we conducted the cell growth assay using tumour-transplant mice. A significant increase in in vivo tumour growth was observed with MSTO-CD26WT as compared with MSTO-Mock (P<0.0001) or MSTO-CD26/10Chi (P<0.0001) (Figure 1D). These results suggest that the cytoplasmic region of CD26 is important for CD26 function in such biological processes of MPM as cell migration, invasion and anchorage-independent cell growth as well as in vivo tumour growth using xenograft mouse model.
The cytoplasmic region of CD26 is required for cell migration, invasion and colony formation. (A) Cells were seeded on top of a Boyden chamber. The number of cells that migrated through the uncoated filter in the lower chamber was counted. The mean number of cells per field was determined from five fields per filter (mean±s.e.m.; n=5 experiments with triplicates). A significant increase in MSTO-CD26WT is indicated as P<0.0001 (vs MSTO-Mock or MSTO-CD26/10Chi), as calculated by ANOVA with Tukey–Kramer post hoc test. NS denotes ‘not significant’. Representative microphotographs of cells migrating through the filter were shown in the lower panels (crystal violet staining). Scale bars indicate 200 μm. (B) Cells were seeded on top of Matrigel-coated chamber inserts. The number of cells that invaded through the Matrigel in the lower chamber was counted. The mean number of cells per field was determined from five fields per filter (mean±s.e.m.; n=5 experiments with triplicates). A significant increase in MSTO-CD26WT is indicated as P<0.0001 (vs MSTO-Mock or MSTO-CD26/10Chi), as calculated by ANOVA with Tukey–Kramer post hoc test. NS denotes ‘not significant’. Representative microphotographs of cells invading through the filter were shown in the lower panels (crystal violet staining). Scale bar indicates 200 μm. (C) Cells were plated in a cell suspension agar matrix between layers of base agar matrix. After 1 week, the agar matrix was solubilised and the cells were stained with MTT solution. Absorbance at 570 nm was measured (mean±s.e.m.; n=5 experiments with triplicates). A significant increase in MSTO-CD26WT is indicated as P<0.0001 (vs MSTO-Mock or MSTO-CD26/10Chi), as calculated by ANOVA with Tukey–Kramer post hoc test. NS denotes ‘not significant’. Representative microphotographs of cells grown in soft agar just before solubilisation to indicate cell size and morphology were shown in the lower panels (phase-contrast imaging). Original magnification, × 8. Scale bars indicate 50 μm. (D) SCID mice were injected i.p. with 1 × 105 luciferase-expressing MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi cells. Tumour growth was measured by in vivo bioluminescence photometry, with imaging data of each cohort being indicated as total flux of photons per second (mean±s.e.m.; n=20). A significant increase in MSTO-CD26WT is indicated as P<0.0001 (vs MSTO-Mock or MSTO-CD26/10Chi), as calculated by ANOVA with Tukey–Kramer post hoc test. Representative optical bioluminescence imaging of each cohort mice was shown with intensity of luminescence as heat maps in the lower panels. The full colour version of this figure is available at British Journal of Cancer online.
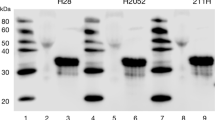
CD26 associates with SSTR4 via their respective cytoplasmic regions
To define the molecular details involved in the critical role of the CD26 cytoplasmic region, we used affinity purification and LC-MS/MS to identify the proteins that are associated with the CD26 cytoplasmic domain. In these experiments, membrane fractions of MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi were harvested in native conditions and subjected to affinity purification using anti-CD26 pAb. LC-MS/MS analysis suggested that the CD26 cytoplasmic region copurified with CD26, actin, TRAK2 (trafficking protein, kinesin binding 2), PEX1 (peroxin1), ribosomal proteins (S2, S3 and S4) and SSTR4 (lane 2 of Figure 2A). It is expected that CD26 co-precipitates with CD26 itself as CD26 forms homodimers in cell membrane (Chien et al, 2004). To determine whether these proteins are present in MPM cells, we conducted a conventional western blotting analysis using total cell lysates of MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi. While SSTR4 was detected, TRAK2 and PEX1 of MSTO cells was not detected in 50 μg of each lysate, suggesting that SSTR4 is a primary CD26-interacting protein involved in MPM cell regulation. In addition, as actin and ribosomal proteins (S2, S3 and S4) exist abundantly in cells, the presence of these proteins in the copurified complex might not be specific to CD26. We have therefore confirmed the presence of SSTR4 in the CD26-interacting complex by western blotting analysis. As shown in Figure 2B, SSTR4 coimmunoprecipitated with CD26 in MSTO-CD26WT (lane 2), but not MSTO-Mock or MSTO-CD26/10Chi (lanes 1 or 3, respectively). In addition, the association of endogenous CD26 and SSTR4 was confirmed by coimmunoprecipitation experiments using JMN or MESO1 cells that express CD26 endogenously (lanes 2 or 3 of Figure 2C, respectively, and Supplementary Figure S1B). To confirm the above findings in living cells, we performed immunocytochemical analysis using confocal laser microscopy. As shown in Figure 2D, the association of endogenous CD26 and SSTR4 was clearly observed in JMN or MESO1 cells. These results indicate that the interaction between CD26 and SSTR4 occurs not only in MPM cells with exogenous CD26 expression, but also in MPM cells with natively expressed CD26.
CD26 interacts with somatostatin receptor 4 (SSTR4) in MPM cells. (A) Immunoaffinity purification of CD26-containing proteins. Membrane fractions of MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi were extracted in a native condition. After being precleared with normal goat immunoglobulin (Ig) crosslinked Dynabeads, the native membrane extracts were immunoprecipitated with anti-CD26 pAb-crosslinked Dynabeads and eluted. The eluates were resolved by the Blue Native PAGE and sliver stained. The protein bands were retrieved and analysed by tandem mass spectrometry. The determined proteins were indicated in the right of the panel. Similar results were obtained in three independent experiments. (B) Immunoprecipitation assay using membrane extractions from MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi. After being precleared with normal goat Ig crosslinked Dynabeads, the membrane extracts were immunoprecipitated by the same method as shown in (A). The eluates were resolved by SDS–PAGE, and immunoblotted using anti-CD26 or anti-SSTR4 antibodies (upper two panels). Total lysates from each cell type were resolved by SDS–PAGE, and immunoblotted using anti-CD26 or anti-SSTR4 antibodies (lower two panels). SSTR4 is co-precipitated with CD26WT, but not with CD26/CD10 chimaeric protein (upper panel). Similar results were obtained in three independent experiments. (C) Immunoprecipitation assay using membrane extractions from parental MSTO-H211 (MSTO-P), JMN or H-MESO-1 (MESO1) cell lines. The membrane extracts were immunoprecipitated and immunoblotted by the same method as shown in (B). SSTR4 is co-precipitated with natively expressing CD26 molecules (upper panel). Similar results were obtained in three independent experiments. (D) Colocalisation of CD26 with SSTR4. JMN or MESO1 cells were fixed using 4% paraformaldehyde-PBS, and stained with Alexa Fluor 488-conjugated anti-CD26 pAb and Alexa Fluor 594-conjugated anti-SSTR4 pAb. Stained cells were mounted using Prolong Gold antifade reagent with DAPI. Observations were made on 10–15 cells in each of three different experiments using confocal laser microscopy. The micrographs are representative of >75% of the cells observed. CD26 and SSTR4 are observed as punctate coexpression on the cell surface. Original magnification, × 200. Scale bars indicate 25 μm. (E) Association of CD26 with SSTR4 via their respective C-terminal region. After being precleared using normal mouse Ig and protein G resin, membrane extracts from HEK293 cells transiently expressing full-length CD26 (CD26WT), CD26-CD10 chimaeric receptor (CD26/10Chi), FLAG-tagged full-length SSTR4 (SSTR4WT-FLAG) or FLAG-tagged SSTR4 with deleted C-terminal cytoplasmic tail (SSTR4ΔC-FLAG) were immunoprecipitated with anti-FLAG affinity resin. Immunocomplexes were then immunoblotted using anti-CD26 or anti-FLAG antibodies (upper two panels). Total lysates from each cell were resolved by SDS–PAGE, and immunoblotted using anti-CD26 or anti-FLAG antibodies (lower two panels). Co-precipitation is observed in CD26WT and SSTR4WT, but not in CD26WT and SSTR4ΔC, CD26/10Chi and SSTR4WT, or CD26/10Chi and SSTR4ΔC (upper panel). Similar results were obtained in three independent experiments. The full colour version of this figure is available at British Journal of Cancer online.
Previous work has demonstrated that the C-terminal intracytoplasmic tail of SSTR4 is essential for homo- and hetero-dimerisation (Somvanshi et al, 2009). To determine whether the C-terminal intracytoplasmic tail of SSTR4 is required for binding to CD26, we constructed the C-terminal deletion mutant of FLAG-tagged SSTR4 (SSTR4ΔC-FLAG), and coimmunoprecipitation experiments were then conducted. As shown in Figure 2E, the full-length SSTR4 (SSTR4WT-FLAG) co-precipitated with CD26WT (lane 2), but not with CD26/10Chi (lane 4), while SSTR4ΔC-FLAG did not co-precipitate with CD26WT (lane 3), nor with CD26/10Chi (lane 5). Taken together with the results described earlier, our data indicate that the association between CD26 and SSTR4 requires for their respective cytoplasmic domains.
Cytostatic effects of SSTR4 agonist are enhanced following suppression of CD26 expression
Since previous reports have shown that SSTR4 agonists mediate growth inhibition of neuroendocrine cells (Patel, 1999; Weckbecker et al, 2003), we next examined the effect of SSTR4 on MPM cell migration, invasion and colony formation. For this purpose, knockdown experiments using siRNA against SSTR4 were conducted in MPM cells. Expression of CD26 or SSTR4 was determined by western blotting analysis of cell lysates of MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi in the presence of control siRNA or two different sequences of SSTR4-siRNAs (si-1 or si-2) (Supplementary Figure S2A). As shown in Figure 3A, inhibition of migration, invasion and colony formation was abrogated in MSTO-Mock (P<0.0001) and MSTO-CD26/10Chi (P<0.0001) in the presence of SSTR4-siRNAs. For cells treated with control siRNA (csi), an increase in migration, invasion and colony formation was observed in MSTO-CD26WT (* in panels a–c of Figure 3A) as compared with MSTO-Mock (P<0.0001) or MSTO-CD26/10Chi (P<0.0001), similar to results seen in Figure 1A–C. However, the enhancement in cellular activities seen in MSTO-CD26WT was not affected by SSTR4-siRNAs (NS in panels a–c of Figure 3A). These results suggest that coexpression of SSTR4 with full-length CD26 inhibits the SSTR4-mediated cytostatic effects. Meanwhile, it is possible that SSTR4 agonist-like factors may be present in FBS of the culture medium, as SSTRs bind the naturally occurring peptides SST-14 and SST-28 with similar affinity (Bruns et al, 1994), affecting cell migration, invasion or colony formation of MSTO-Mock and MSTO-CD26/10Chi (panels a–c of Figure 3A). To exclude the possibility of serum-derived SSTR4 agonistic effect, we established various MPM cell lines that have been adapted to the serum-reduced condition, and conducted cell migration, invasion and colony formation assays in the presence or absence of the specific SSTR4 agonist L803087 (Rohrer, 1998). The expression levels of CD26 or SSTR4 in these adapted MPM cells were confirmed by western blot analysis to be similar to those of respective parental cells (Supplementary Figure S2B). As shown in Figure 3B, levels of cell migration, invasion and colony formation were observed to be equal among MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi (NS at points of medium alone in panels a–c), suggesting that the influence of serum on these cell lines was minimised by the serum-reduced condition. Under this serum-reduced condition, inhibition of migration, invasion and colony formation of MSTO-Mock or MSTO-CD26/10Chi by the SSTR4 agonist was observed in a dose-dependent manner (○ or ▴ in panels a–c, respectively), while inhibition of migration, invasion or colony formation of MSTO-CD26WT in a serum-reduced condition was not observed ( × in panels a–c of Figure 3B). These results strongly suggest that SSTR4-mediated cytostatic effects are abrogated in the presence of CD26.
SSTR4-mediated cytostatic effects are inhibited in the presence of CD26. (A) MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi cells were transfected with two different siRNAs against SSTR4 (si-1 or si-2) or control siRNA (csi). After 48 h of transfection, cell migration (panel a), invasion (panel b) or colony formation assays (panel c) were conducted by the same methods as in Figure 1 (mean±s.e.m.; n=5 experiments with triplicates), with results being shown in bar graphs (MSTO-Mock (red bar), MSTO-CD26WT (blue bar) or MSTO-CD26/10Chi (green bar)). A significant increase in si-1 or si-2 in MSTO-Mock or MSTO-CD26/10Chi cells is indicated as P<0.0001 (vs the corresponding csi). A significant increase in csi of MSTO-CD26WT cells (*) is indicated as P<0.0001 (vs csi of MSTO-Mock or MSTO-CD26/10Chi). NS denotes ‘not significant’. P-values are calculated by ANOVA with Tukey–Kramer post hoc test. (B) Using MSTO-Mock, MSTO-CD26WT or MSTO-CD26/10Chi cells adapted to the serum-reduced condition, cell migration (panel a), invasion (panel b) or colony formation assays (panel c) were conducted by the same methods as in Figure 1 (mean±s.e.m.; n=5 experiments with triplicates). The SSTR4 agonist L803087 at the indicated concentrations or DMSO as a solvent control was added to the assays. P<0.0001 vs those in MSTO-Mock or MSTO-CD26/10Chi at respective concentrations of L803087 is calculated by ANOVA with Tukey–Kramer post hoc test. NS denotes ‘not significant’. (C, D) Knockdown of endogenous CD26 induces inhibitory effects of SSTR4 agonist in JMN or MESO1 cells. After being adapted to the serum-reduced condition, endogenous CD26-expressing JMN (C) or MESO1 (D) cells were transfected with two different siRNAs against CD26 (si-1 or si-2), control siRNA (csi) or transfection reagent alone (none). After 48 h of transfection, cell migration (panels a), invasion (panels b) or colony formation assays (panels c) were conducted by the same methods as in Figure 1 (mean±s.e.m.; n=5 experiments with triplicates). The SSTR4 agonist L803087 at the indicated concentrations or DMSO as a solvent control was added to the assays. A significant decrease in si-1 or si-2 is indicated as P<0.0001 (vs the corresponding csi or none), as calculated by ANOVA with Tukey–Kramer post hoc test. The full colour version of this figure is available at British Journal of Cancer online.
To determine whether SSTR4-mediated cytostatic effects are abrogated in the presence of the association between CD26 and SSTR4, knockdown experiments using siRNA against CD26 were conducted in JMN or MESO1 cell lines. Expression of CD26 or SSTR4 was determined by western blotting analysis of cell lysates of JMN or MESO1 cell lines in the presence of control siRNA (csi) or two different sequences of CD26-siRNAs (si-1 or si-2) (Supplementary Figure S2C). Following knockdown of endogenous CD26, inhibition of migration, invasion and colony formation of JMN cells by SSTR4 agonist in a serum-reduced condition was observed in a dose-dependent manner of L803087 (P<0.0001, panels a–c of Figure 3C). Similarly, following knockdown of endogenous CD26 in MESO1 cells adapted to a serum-reduced condition, inhibition of migration, invasion and colony formation by SSTR4 agonist was also observed in a dose-dependent manner of L803087 (P<0.0001, panels a–c of Figure 3D). These results indicate that SSTR4-mediated cytostatic effects are strongly elicited by decreased CD26 expression. Taken together, our results strongly suggest that the association of CD26 with SSTR4 impedes the cytostatic signalling of the SSTR4 agonist.
Downstream signalling via SHP-2 is required for SSTR4-mediated cytostatic effects
To further clarify the role of the association between CD26 and SSTR4 on SSTR4-mediated cytostatic effects in MPM, we next investigated the molecular basis for downstream signalling events elicited by the SSTR4 agonist. Since previous work indicated that PTPs, SHP-1 or SHP-2 are involved in signalling events of the SSTR family (Patel, 1999; Weckbecker et al, 2003; Florio, 2008), we conducted experiments using an SHP inhibitor. As shown in Figure 4A, the SHP-1/2 PTP inhibitor abrogated the inhibitory effect of SSTR4 agonist on cell migration, invasion and colony formation of MSTO-P cells adopted to a serum-reduced condition (panels a–c). To further support the conclusion that SSTR4-mediated cytostatic effects were abrogated by the SHP-1/2 PTP inhibitor, we conducted similar experiments with JMN or MESO1 cells, and found that SSTR4-mediated cytostatic effects in CD26-knockdown cells were abrogated in the presence of the SHP-1/2 PTP inhibitor (panels a–c of Supplementary Figure S3A and B). These results strongly suggest that the SSTR4-mediated cytostatic effects are associated with downstream signalling via SHP-1/2 PTPs.
Downstream signalling with SHP-2 has a role in SSTR4-mediated cytostatic effects. (A) Endogenous CD26-deficient parental MSTO cells (MSTO-P) adapted to the serum-reduced condition were incubated with 1 μ M of SHP-1/2 inhibitor (black bars) or PBS as a solvent control (grey bars) for 30 min, followed by cell migration (panel a), invasion (panel b) or colony formation assays (panel c) in the presence of the SSTR4 agonist L803087 (10 μ M) or DMSO as a solvent control (vehicle) (mean±s.e.m.; n=5 experiments with triplicates). A significant suppression in L803087 treatment without SHP-1/2 inhibitor (P<0.0001, grey bars) was restored in the presence of SHP-1/2 inhibitor (P<0.0001, grey and black bars of L803087), as calculated by ANOVA with Tukey–Kramer post hoc test. (B) MSTO-P cells adapted to the serum-reduced condition were transfected with two different siRNAs against SHP-2 (si-1 or si-2), control siRNA (csi) or transfection reagent alone (none). After 48 h of transfection, cell migration (panel a), invasion (panel b) or colony formation assays (panel c) were conducted by the same methods as in Figure 1 (mean±s.e.m.; n=5 experiments with triplicates). The SSTR4 agonist L803087 at the indicated concentrations or DMSO as a solvent control was added to the assays. A significant increase in si-1 or si-2 is indicated as P<0.0001 (vs the corresponding csi or none), as calculated by ANOVA with Tukey–Kramer post hoc test.
To further characterise the involvement of SHP-1/2 PTPs downstream of SSTR4, we next analysed expression levels of SHP-1 and SHP-2 in various cell lines. As shown in Supplementary Figure S3C, MPM cell lines used in the current study expressed SHP-2, but not SHP-1. These results suggest that SHP-2 PTP is predominantly associated with SSTR4-mediated cytostatic effects in our experimental system. As further support for this conclusion, we next conducted knockdown experiments using siRNAs against SHP-2 in MSTO-Mock cells. Expression of SHP-1/2, SSTR4 and CD26 was determined by western blotting analysis of cell lysates in the presence of control siRNA (csi) or two different sequences of SHP-2-siRNAs (si-1 or si-2). Endogenous SHP-2 was clearly reduced by SHP2-siRNAs without any change in the level of endogenous SSTR4 expression. Endogenous CD26 and SHP-1 were not detected in MSTO-Mock (Supplementary Figure S3D). As shown in Figure 4B, SHP-2-siRNAs clearly abrogated SSTR4-mediated cytostatic effects in MSTO-Mock cells (▴ or ♦ in panels a–c), with dose-dependent inhibition of migration, invasion and colony formation by SSTR4 agonist being observed in a dose-dependent manner (○ or × in panels a–c). Our overall results hence indicate that SSTR4-mediated cytostatic effects in MPM cells are exerted via SHP-2 signalling.
SSTR4-mediated cytostatic effects are enhanced via lipid raft aggregation induced by humanised anti-CD26 mAb
It has been previously shown that CD26-mediated costimulatory signalling in T cells was exerted via lipid raft clustering (Ishii et al, 2001; Ohnuma et al, 2007). Moreover, it is estimated that SSTR4 is recruited into lipid rafts via a palmitoyl membrane anchor site which is located at the cysteine residue of its C-tail region (Patel, 1999). In view of these molecular characteristics of CD26 and SSTR4, to define the molecular events involved in the formation of these critical integrated cell membrane protein–protein complexes, we analysed the molecular clustering induced by lipid raft aggregation in MPM cells treated with humanised anti-CD26 mAb. As shown in Figure 5A, humanised anti-CD26 mAb treatment resulted in increased levels of CD26, SSTR4 and SHP-2 molecules in lipid raft fractions (upper three of right panels) while a non-lipid raft anchored protein, transferrin receptor (TfR), was not aggregated in lipid raft fractions (bottom panels). Furthermore, to examine whether anti-CD26 mAb treatment affects CD26 binding to SSTR4 in lipid rafts, co-precipitation assay was performed using lipid raft fractions. As shown in Figure 5B, CD26 in lipid rafts of MPM cell treated with control IgG was co-precipitated with SSTR4 (lane 1), while CD26 was not co-precipitated with SSTR4 in lipid raft fractions of MPM cells following stimulation with humanised anti-CD26 mAb, despite the presence of SSTR4 in lipid raft fractions (lane 2). These results suggest that SSTR4 and CD26 are associated in lipid rafts, and that anti-CD26 mAb ligates CD26 to cause the release of SSTR4 from CD26 and the clustering of SSTR4 in lipid rafts, hence providing a platform for signalling events associated with multimerisation of SSTR4 molecules, such as SHP-2 activation.
Humanised anti-CD26 mAb ligation promotes SSTR4 clustering with CD26 in lipid rafts and enhances SSTR4-mediated cytostatic effects. (A) MSTO-CD26WT cells were stimulated for 10 min with humanised anti-CD26 mAb alone (5.0 μg ml−1), or with control human Ig (5.0 μg ml−1) in the presence of anti-Fcγ (5.0 μg ml−1). Lipid raft or cytosolic fractions were prepared by sucrose gradient ultracentrifugation. The distribution of CD26, SSTR4, SHP-2 and transferrin receptor (TfR) was determined by immunoblotting with specific antibodies. TfR is a representative of non-lipid raft proteins, and used as a quantity control indicating equal amounts in the experiments. Fraction number (Fr#) 3–5 or 9–11 contains lipid raft or cytosolic fractions, respectively. CD26, SSTR4 and SHP-2 molecules are recruited into the lipid raft fractions after anti-CD26 mAb treatment (upper three in the right panels). Similar results were obtained in three independent experiments. (B) MSTO-CD26WT cells were stimulated, and sucrose gradient ultracentrifugation was conducted by the same methods as in (A). Lipid raft fractions were pooled by collection of corresponding Fr#3–5. After being precleared with normal rabbit IgG, immunoprecipitation of lipid rafts with anti-SSTR4 rabbit pAb was performed, followed by resolution with SDS–PAGE, and immunoblotted with the indicated antibodies. After stimulation by anti-CD26 mAb, SSTR4 molecules were increased in lipid rafts (lane 2 of the lower panel), while the association of SSTR4 with CD26 molecules was decreased (lane 2 of the upper panel). Similar results were obtained in three independent experiments. * corresponds to the protein bands of immunoglobulin heavy chain, and arrow head, those of SSTR4. (C) MSTO-CD26WT cells adapted to the serum-reduced condition were incubated with 1 μM of cytochalasin D (Cytoch. D) or DMSO as a solvent control for 30 min, followed by cell migration (panel a), invasion (panel b) or colony formation assays (panel c) in the presence of the SSTR4 agonist L803087 (10 μM) or DMSO as a solvent control (mean±s.e.m.; n=5 experiments with triplicates). A significant decrease in anti-CD26 mAb-treated cell in control reagents was observed (P<0.0001, white bars), and a more profound decrease was observed in the presence of L803087 (*, P<0.0001). This reduction in the anti-CD26 mAb treatment group was restored in the presence of Cytoch. D (P<0.0001). P-values are calculated by ANOVA with Tukey–Kramer post hoc test.
To further evaluate the association of CD26 and SSTR4 via lipid raft, we conducted experiments using a lipid raft disturbing reagent, cytochalasin D (Cytoch. D) (Ishii et al, 2001). Cytoch. D slightly inhibited cell migration, invasion and colony formation at the indicated concentration (P<0.001) (panels a–c of Figure 5C), as Cytoch. D is a potent inhibitor of actin polymerisation (Brenner and Korn, 1979). However, as shown in panels a–c of Figure 5C, anti-CD26 mAb treatment resulted in enhanced inhibitory effect on cell migration, invasion and colony formation at the indicated concentration (P<0.0001), and this inhibitory effect was more profoundly exerted in the presence of the SSTR4 agonist (*, P<0.0001). On the other hand, this inhibitory effect of anti-CD26 mAb on cell migration, invasion and colony formation was reversed in the presence of Cytoch. D (P<0.001) (panels a–c of Figure 5C). Similar effects of Cytoch. D were observed in cell migration, invasion and colony formation assays using JMN or MESO1 cells (Supplementary Figure S4B or C, respectively). These results indicate that the effect of humanised anti-CD26 mAb on anti-tumour activity is enhanced by SSTR4-mediated activation of SHP-2, which is induced by lipid raft clustering.
Anti-tumour effect of humanised anti-CD26 mAb is enhanced in combination with SSTR4 agonist in vivo
To further validate our in vitro observations regarding the enhancing effect of humanised anti-CD26 mAb treatment on SSTR4-mediated anti-tumour effect, we conducted in vivo experiments using SCID mice transplanted with MPM cells. As shown in Figure 6A and B, humanised anti-CD26 mAb reduced the tumorigenicity of s.c. inoculated JMN (blue line, P<0.0001), while this anti-tumour effect was not observed in mice treated with the SSTR4 agonist L803087 alone (green or yellow lines). This in vivo anti-tumour effect was enhanced with the combined administration of humanised anti-CD26 mAb and SSTR4 agonist (red line in Figure 6A, P<0.0001, and Figure 6B). To further define the in vivo effect of the combined treatment of anti-CD26 mAb and SSTR4 agonist, serial BLI study was conducted. As shown in Figure 6C, humanised anti-CD26 mAb reduced the tumorigenicity of i.p. inoculated JMN (blue line, P<0.0001), while this anti-tumour effect was not observed in mice treated with the SSTR4 agonist L803087 alone (green or yellow lines). This in vivo anti-tumour effect was enhanced with the combined administration of humanised anti-CD26 mAb and SSTR4 agonist (red line in Figure 6C, P<0.0001). Taken together with results of the in vitro experiments presented in Figure 5C; Supplementary Figure S4A and B, our work illustrates the potency of the anti-tumour effect of the combination of humanised anti-CD26 mAb and the SSTR4 agonist on CD26-expressing MPM cells.
The inhibitory effect of combination of SSTR4 agonist and humanised anti-CD26 mAb on tumour growth in a murine xenograft model. (A) JMN cells (1 × 106) were inoculated s.c. into the left flank of mice. Mice were treated with i.p. injection of control IgG (10 μg per dose) alone, SSTR4 agonist L803087 (20 μ M per dose) alone, L803087 (20 μ M per dose) plus control IgG (10 μg per dose), humanised anti-CD26 mAb (10 μg per dose) alone or L803087 (20 μ M per dose) plus humanised anti-CD26 mAb (10 μg per dose) on the seventh day post cancer cell inoculation, when the tumour mass became visible (5 mm in size). Each antibody or agonist was given three times per week. Each cohort was examined with n=20. A significant decrease in the anti-CD26 mAb treatment cohort (blue line) was observed (P<0.0001 vs control Ig, L803087 alone or L803087 plus control Ig cohort), and more profound decrease was observed in the L803087 plus anti-CD26 mAb treatment cohort (red line, P<0.0001 vs control Ig, L803087 alone, L803087 plus control Ig or anti-CD26 mAb alone cohort). P-values are calculated by ANOVA with Tukey–Kramer post hoc test. (B) Representative macroscopic photo of resected specimens in an s.c. tumorigenicity model on the 28th day post first treatment. Scale bar indicates 1 cm. (C) After 1 day of i.p. injection of luciferase-expressing JMN cells (1 × 105), mice were treated with i.p. injection of control IgG (10 μg per dose), L803087 (20 μ M per dose) plus control IgG (10 μg per dose), humanised anti-CD26 mAb (10 μg per dose) alone or L803087 (20 μ M per dose) plus humanised anti-CD26 mAb (10 μg per dose). Each antibody or agonist was given three times per week. Tumour growth was measured by in vivo bioluminescence photometry, with imaging data of each cohort being indicated as total flux of photons per second (mean±s.e.m.; n=20). A significant decrease in anti-CD26 mAb treatment cohort (blue line) was observed (P<0.0001 vs control Ig, L803087 alone or L803087 plus control Ig cohort), and a more profound decrease was observed in the L803087 plus anti-CD26 mAb treatment cohort (red line, P<0.0001 vs control Ig, L803087 alone, L803087 plus control Ig or anti-CD26 mAb alone cohort). P-values are calculated by ANOVA with Tukey–Kramer post hoc test. Representative optical bioluminescence imaging of each cohort mice was shown with intensity of luminescence as heat maps in the right panels. The full colour version of this figure is available at British Journal of Cancer online.
Coexpression of CD26 and SSTR4 is detected in surgical specimens of MPM patients
To explore the potential implications of SSTR4-mediated cytostatic effects in the clinical setting, we evaluated SSTR4 expression level in surgically resected human MPM tissues. Fifty consecutive surgically resected specimens from the primary sites were examined for membranous expression of SSTR4 and CD26. CD26 was highly expressed on epithelioid or biphasic type of MPM (panel b of Figure 7A and B), findings that were consistent with the results we showed previously (Aoe et al, 2012). In addition, SSTR4 was detected on epithelioid or biphasic type of MPM, predominantly coexpressed with membranous CD26 (panel c of Figure 7A and black bars of Figure 7B). These results suggest that selected MPM patients may be suitable candidates for a combined therapeutic approach with an anti-CD26 mAb and an SSTR4 agonist.
Coexpression of CD26 and SSTR4 in surgical specimens of MPM patients. (A) Representative serial sections of resected specimens of epithelioid type of malignant mesothelioma. Panel a, Haematoxylin and eosin (H&E) stain, panel b, anti-CD26 and panel c, anti-SSTR4 immunohistochemistry. Original magnification, x100. (B) CD26 and SSTR4 expression profile among 50 patient tissues. Fifty consecutive surgically resected specimens from the primary sites were examined for membranous expression of SSTR4 and CD26 by the same method as in (A). CD26 was highly expressed on epithelioid or biphasic type of MPM (purple bars), and SSTR4 was detected on epithelioid or biphasic type of MPM (red bars), predominantly coexpressed with membranous CD26 (black bars). The full colour version of this figure is available at British Journal of Cancer online.
Discussion
In this article, we show that CD26 is associated with SSTR4 in MPM cells, and this interaction inhibits SSTR4-mediated cytostatic effects. Moreover, we show using exogenous expression of deletion mutants that this molecular association needs the intracytoplasmic region of CD26 and the C-tail region of SSTR4. The present study also indicates that SSTR4-mediated cytostatic effects are transduced by SHP-2 PTP, and that this inhibitory effect is enhanced via lipid raft clustering of associated molecules following crosslinking of anti-CD26 mAb. Furthermore, using an in vivo xenograft model, we demonstrate that the anti-tumour effect of humanised anti-CD26 mAb is enhanced when combined with SSTR4 agonist treatment. Finally, we show that SSTR4 is highly coexpressed with CD26 on epithelioid or biphasic types of MPM tissues obtained from patients’ surgical specimens.
We previously showed that anti-CD26 mAb inhibited growth of MPM cells and induced long-term survival of tumour-transplanted SCID mice (Inamoto et al, 2007). Recently, we showed that CD26 is preferentially expressed in MPM cells but not in normal mesothelial cells (Amatya et al, 2011), and suggested that membranous expression of CD26 is of potential importance in the treatment of MPM patients (Aoe et al, 2012). More recently, we showed that anti-CD26 mAbs induced the nuclear translocation of CD26 molecules to inhibit proliferation of MPM cells via suppression of POLR2A gene expression (Yamada et al, 2009, 2013). CD26 molecules were observed in the nucleus 30 min after anti-CD26 mAb treatment, peaking at 120 min and decreasing by 240 min. However, these findings did not provide an understanding of the earlier signalling events involved in the regulation of cell motility by CD26. Another regulatory mechanism for the malignant behaviour of CD26-expressing MPM cells involves the expression of CD9. We demonstrated that cells from certain CD26-positive MPM cell lines appeared to include the cancer stem cell characteristics for malignant mesothelioma in addition to CD24+CD9+ cells (Ghani et al, 2011; Yamazaki et al, 2012), and that CD9 suppressed cell invasion and migration by inhibiting the formation of CD26–α5β1 integrin complex with an associated decrease in phosphorylation of β1 integrin-related proteins such as focal adhesion kinase (FAK) and Crk-associated substrate lymphocyte type (Cas-L/HEF1/NEDD9) (Okamoto et al, 2014). Moreover, we showed that CD26 was associated with integrin-dependent adhesion of T-anaplastic large cell lymphoma Karpas 299 to ECM by regulating p38-MAPK (mitogen-activated protein kinase)-dependent phosphorylation of β1 integrin (Sato et al, 2005). While these findings indicate that CD26 regulates ECM-associated tumour cell behaviour, the exact proximal molecular signalling events in tumour biology associated with the cytoplasmic region of CD26 remain to be elucidated, although those involved with the regulation of normal T-cell physiology have been well characterised (Ohnuma et al, 2008). In the present study, we demonstrate that the presence of the cytoplasmic, not the extracellular, region of CD26 resulted in enhanced MPM cell growth in vivo as well as in vitro migration, invasion and colony formation. In addition, we demonstrate that the cytoplasmic region of CD26 had a crucial role in MPM tumour biology through its linkage to SSTR4 and SHP-2 PTP in cell membrane lipid rafts, leading to cytostatic effects in MPM cells without direct association of ECM to CD26.
While SSTR subtypes have an important role in regulating tumour cell proliferation, SSTR4 is the least well-understood receptor among all the SSTR subtypes (Kumar, 2013). In the present study, we showed that SSTR4 was clearly expressed in MPM clinical specimens as well as various MPM cell lines, and that specific agonist for SSTR4 exhibited anti-tumour effects. Although these anti-tumour effects were blocked by coexpression of CD26, ligation of CD26 molecules by humanised anti-CD26 mAb induced lipid raft aggregation, leading to the activation of the cytostatic signalling molecule SHP-2 via clustering of SSTR4, which provides a platform for signalling events associated with multimerisation of SSTR4 molecules. Moreover, our observation that clustering of SSTR4 occurs in lipid raft is consistent with the findings that the C-terminal intracytoplasmic tail of SSTR4 and its oligomerisation are required for its cytostatic effects via SHP-2 recruitment in SSTR4-associated complex (Somvanshi et al, 2009). Although different pathways have been identified to regulate SST-induced inhibition of cell proliferation, according to the SSTR subtypes and experimental models, there is now an emerging consensus regarding the central role played by activation of PTPs in this process (Weckbecker et al, 2003; Florio, 2008). In fact, we showed that SHP-2 was required for SSTR4-mediated cytostatic effects in MPM cells, and that SHP-2 was clustered in lipid rafts along with the SSTR4 molecules that presumably disengaged from CD26. Moreover, the SST-regulated PTPs control the activity of a number of downstream signalling molecules and, ultimately, induce an upregulation of cyclin-dependent kinase inhibitors (CDKIs), such as p21cip1 and p27kip1 (Reardon et al, 1997; Florio, 2008). These data support our previous findings that anti-CD26 mAb treatment induces upregulation of these CDKIs in T cells, renal carcinoma and MPM cells (Ohnuma et al, 2002; Inamoto et al, 2006, 2007).
As predicted by the mass-spectrometry analysis for proteins copurified with anti-CD26, we could not formally exclude the possibility that TRAK2, PEX1, actin or ribosomal proteins are involved in CD26-associated cell proliferation or mobility. It has been reported that TRAK2 and actin are cell membrane-associated proteins and that PEX1 or ribosomal proteins are abundantly located in peroxisomes or ribosomes (Tamura et al, 1998; Beck et al, 2002). In particular, actin or TRAK2 may interact with CD26 directly or indirectly to regulate the pathways involved in cell mobility (Beck et al, 2002; Buchan et al, 2002). Since our present effort aims to identify cell surface membrane proteins that can associate with the cytoplasmic region of CD26 in MPM cell lines, we focus our investigation on the membrane protein SSTR4 in the current study.
Although CD26/DPPIV is capable of cleaving N-terminal dipeptides with either L-proline or L-alanine at the penultimate position through its DPPIV activity (Ohnuma et al, 2008), the SSTR4 agonist used in the current study and the naturally occurring peptides SST-14 and SST-28 do not possess such amino-acid sequences (Bruns et al, 1994). Therefore, it is likely that the inhibition of SSTR4-mediated cytostatic effects observed in the present study is not due to cleavage of its agonists by CD26/DPPIV.
Meanwhile, data from the clinical samples obtained from patients with MPM revealed that SSTR4 is detected in almost all MPM tissues expressing membranous CD26. Taken together with the current in vitro observations, these results suggest that a novel therapeutic approach combining anti-CD26 mAb and an SSTR4 agonist may be of clinical benefit in selected patients with MPM, a notion that will be explored in future investigations. Likewise, the role of CD26 and SSTR4 coexpression as potential biomarkers and prognostic markers in MPM will be investigated in future studies.
In conclusion, we report that CD26 associates with SSTR4 in MPM cells, leading to high proliferative, migratory and invasive activities by CD26-expressing MPM cells. Humanised anti-CD26 mAb induces SSTR4 aggregation in lipid rafts and potentiates its cytostatic and anti-tumour effects. As SSTR4 and CD26 are found to coexpress in surgically resected specimens of human MPM, combination therapy using humanised anti-CD26 mAb and an SSTR4 agonist may provide clinical benefits in MPM.
Change history
29 April 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Amatya VJ, Takeshima Y, Kushitani K, Yamada T, Morimoto C, Inai K (2011) Overexpression of CD26/DPPIV in mesothelioma tissue and mesothelioma cell lines. Oncol Rep 26: 1369–1375.
Aoe K, Amatya VJ, Fujimoto N, Ohnuma K, Hosono O, Hiraki A, Fujii M, Yamada T, Dang NH, Takeshima Y, Inai K, Kishimoto T, Morimoto C (2012) CD26 overexpression is associated with prolonged survival and enhanced chemosensitivity in malignant pleural mesothelioma. Clin Cancer Res 18: 1447–1456.
Astoul P, Roca E, Galateau-Salle F, Scherpereel A (2012) Malignant pleural mesothelioma: from the bench to the bedside. Respiration 83: 481–493.
Beck M, Brickley K, Wilkinson HL, Sharma S, Smith M, Chazot PL, Pollard S, Stephenson FA (2002) Identification, molecular cloning, and characterization of a novel GABAA receptor-associated protein, GRIF-1. J Biol Chem 277: 30079–30090.
Brenner SL, Korn ED (1979) Substoichiometric concentrations of cytochalasin D inhibit actin polymerization. Additional evidence for an F-actin treadmill. J Biol Chem 254: 9982–9985.
Britton M (2002) The epidemiology of mesothelioma. Semin Oncol 29: 18–25.
Bruns C, Weckbecker G, Raulf F, Kaupmann K, Schoeffter P, Hoyer D, Lubbert H (1994) Molecular pharmacology of somatostatin-receptor subtypes. Ann NY Acad Sci 733: 138–146.
Buchan AM, Lin CY, Choi J, Barber DL (2002) Somatostatin, acting at receptor subtype 1, inhibits Rho activity, the assembly of actin stress fibers, and cell migration. J Biol Chem 277: 28431–28438.
Chien CH, Huang LH, Chou CY, Chen YS, Han YS, Chang GG, Liang PH, Chen X (2004) One site mutation disrupts dimer formation in human DPP-IV proteins. J Biol Chem 279: 52338–52345.
Florio T (2008) Somatostatin/somatostatin receptor signalling: phosphotyrosine phosphatases. Mol Cell Endocrinol 286: 40–48.
Froidevaux S, Eberle AN (2002) Somatostatin analogs and radiopeptides in cancer therapy. Biopolymers 66: 161–183.
Ghani FI, Yamazaki H, Iwata S, Okamoto T, Aoe K, Okabe K, Mimura Y, Fujimoto N, Kishimoto T, Yamada T, Xu CW, Morimoto C (2011) Identification of cancer stem cell markers in human malignant mesothelioma cells. Biochem Biophys Res Commun 404: 735–742.
Haas AR, Sterman DH (2013) Malignant pleural mesothelioma: update on treatment options with a focus on novel therapies. Clin Chest Med 34: 99–111.
Havre PA, Abe M, Urasaki Y, Ohnuma K, Morimoto C, Dang NH (2008) The role of CD26/dipeptidyl peptidase IV in cancer. Front Biosci 13: 1634–1645.
Ho L, Aytac U, Stephens LC, Ohnuma K, Mills GB, McKee KS, Neumann C, LaPushin R, Cabanillas F, Abbruzzese JL, Morimoto C, Dang NH (2001) In vitro and in vivo antitumor effect of the anti-CD26 monoclonal antibody 1F7 on human CD30+ anaplastic large cell T-cell lymphoma Karpas 299. Clin Cancer Res 7: 2031–2040.
Inamoto T, Yamada T, Ohnuma K, Kina S, Takahashi N, Yamochi T, Inamoto S, Katsuoka Y, Hosono O, Tanaka H, Dang NH, Morimoto C (2007) Humanized anti-CD26 monoclonal antibody as a treatment for malignant mesothelioma tumors. Clin Cancer Res 13: 4191–4200.
Inamoto T, Yamochi T, Ohnuma K, Iwata S, Kina S, Inamoto S, Tachibana M, Katsuoka Y, Dang NH, Morimoto C (2006) Anti-CD26 monoclonal antibody-mediated G1-S arrest of human renal clear cell carcinoma Caki-2 is associated with retinoblastoma substrate dephosphorylation, cyclin-dependent kinase 2 reduction, p27kip1 enhancement, and disruption of binding to the extracellular matrix. Clin Cancer Res 12: 3470–3477.
Ishii T, Ohnuma K, Murakami A, Takasawa N, Kobayashi S, Dang NH, Schlossman SF, Morimoto C (2001) CD26-mediated signaling for T cell activation occurs in lipid rafts through its association with CD45RO. Proc Natl Acad Sci USA 98: 12138–12143.
Kumar U (2013) G-Protein coupled receptors dimerization: diversity in somatostatin receptors subtypes. J Pharmacogenomics Pharmacoproteomics 4: 120–129.
Maguer-Satta V, Besancon R, Bachelard-Cascales E (2011) Concise review: neutral endopeptidase (CD10): a multifaceted environment actor in stem cells, physiological mechanisms, and cancer. Stem Cells 29: 389–396.
Montironi R, Cheng L, Mazzucchelli R, Morichetti D, Stramazzotti D, Santinelli A, Moroncini G, Galosi AB, Muzzonigro G, Comeri G, Lovisolo J, Cosciani-Cunico S, Bono AV (2008) Immunohistochemical detection and localization of somatostatin receptor subtypes in prostate tissue from patients with bladder outlet obstruction. Cell Oncol 30: 473–482.
Morimoto C, Schlossman SF (1998) The structure and function of CD26 in the T-cell immune response. Immunol Rev 161: 55–70.
Myers R (2012) Asbestos-related pleural disease. Curr Opin Pulm Med 18: 377–381.
Ogata S, Misumi Y, Ikehara Y (1989) Primary structure of rat liver dipeptidyl peptidase IV deduced from its cDNA and identification of the NH2-terminal signal sequence as the membrane-anchoring domain. J Biol Chem 264: 3596–3601.
Ohnuma K, Dang NH, Morimoto C (2008) Revisiting an old acquaintance: CD26 and its molecular mechanisms in T cell function. Trends Immunol 29: 295–301.
Ohnuma K, Ishii T, Iwata S, Hosono O, Kawasaki H, Uchiyama M, Tanaka H, Yamochi T, Dang NH, Morimoto C (2002) G1/S cell cycle arrest provoked in human T cells by antibody to CD26. Immunology 107: 325–333.
Ohnuma K, Uchiyama M, Yamochi T, Nishibashi K, Hosono O, Takahashi N, Kina S, Tanaka H, Lin X, Dang NH, Morimoto C (2007) Caveolin-1 triggers T-cell activation via CD26 in association with CARMA1. J Biol Chem 282: 10117–10131.
Ohnuma K, Yamochi T, Uchiyama M, Nishibashi K, Yoshikawa N, Shimizu N, Iwata S, Tanaka H, Dang NH, Morimoto C (2004) CD26 up-regulates expression of CD86 on antigen-presenting cells by means of caveolin-1. Proc Natl Acad Sci USA 101: 14186–14191.
Okamoto T, Iwata S, Yamada H, Hatano R, Komiya E, Dang NH, Ohnuma K, Morimoto C (2014) CD9 negatively regulates CD26 expression and inhibits CD26-mediated enhancement of invasive potential of malignant mesothelioma cells. PLoS One 9 (1): e86671.
Patel YC (1999) Somatostatin and its receptor family. Front Neuroendocrinol 20: 157–198.
Portela-Gomes GM, Stridsberg M, Grimelius L, Rorstad O, Janson ET (2007) Differential expression of the five somatostatin receptor subtypes in human benign and malignant insulinomas - predominance of receptor subtype 4. Endocr Pathol 18: 79–85.
Reardon DB, Dent P, Wood SL, Kong T, Sturgill TW (1997) Activation in vitro of somatostatin receptor subtypes 2, 3, or 4 stimulates protein tyrosine phosphatase activity in membranes from transfected Ras-transformed NIH 3T3 cells: coexpression with catalytically inactive SHP-2 blocks responsiveness. Mol Endocrinol 11: 1062–1069.
Reubi JC, Waser B, Schaer JC, Laissue JA (2001) Somatostatin receptor sst1-sst5 expression in normal and neoplastic human tissues using receptor autoradiography with subtype-selective ligands. Eur J Nucl Med 28: 836–846.
Robinson BW, Lake RA (2005) Advances in malignant mesothelioma. N Engl J Med 353: 1591–1603.
Rohrer SP (1998) Rapid identification of subtype-selective agonists of the somatostatin receptor through combinatorial chemistry. Science 282: 737–740.
Sato T, Yamochi T, Yamochi T, Aytac U, Ohnuma K, McKee KS, Morimoto C, Dang NH (2005) CD26 regulates p38 mitogen-activated protein kinase-dependent phosphorylation of integrin β1, adhesion to extracellular matrix, and tumorigenicity of T-anaplastic large cell lymphoma Karpas 299. Cancer Res 65: 6950–6956.
Shersher DD, Liptay MJ (2013) Multimodality treatment of pleural mesothelioma. Surg Oncol Clin N Am 22: 345–355.
Somvanshi RK, Billova S, Kharmate G, Rajput PS, Kumar U (2009) C-tail mediated modulation of somatostatin receptor type-4 homo- and heterodimerizations and signaling. Cell Signal 21: 1396–1414.
Takeshima Y, Inai K, Amatya VJ, Gemba K, Aoe K, Fujimoto N, Kato K, Kishimoto T (2009) Accuracy of pathological diagnosis of mesothelioma cases in Japan: clinicopathological analysis of 382 cases. Lung Cancer 66: 191–197.
Tamura S, Okumoto K, Toyama R, Shimozawa N, Tsukamoto T, Suzuki Y, Osumi T, Kondo N, Fujiki Y (1998) Human PEX1 cloned by functional complementation on a CHO cell mutant is responsible for peroxisome-deficient Zellweger syndrome of complementation group I. Proc Natl Acad Sci USA 95: 4350–4355.
Weckbecker G, Lewis I, Albert R, Schmid HA, Hoyer D, Bruns C (2003) Opportunities in somatostatin research: biological, chemical and therapeutic aspects. Nat Rev Drug Discov 2: 999–1017.
Yamada K, Hayashi M, Du W, Ohnuma K, Sakamoto M, Morimoto C, Yamada T (2009) Localization of CD26/DPPIV in nucleus and its nuclear translocation enhanced by anti-CD26 monoclonal antibody with anti-tumor effect. Cancer Cell Int 9: 17.
Yamada K, Hayashi M, Madokoro H, Nishida H, Du W, Ohnuma K, Sakamoto M, Morimoto C, Yamada T (2013) Nuclear localization of CD26 induced by a humanized monoclonal antibody inhibits tumor cell growth by modulating of POLR2A transcription. PLoS One 8: e62304.
Yamazaki H, Naito M, Ghani FI, Dang NH, Iwata S, Morimoto C (2012) Characterization of cancer stem cell properties of CD24 and CD26-positive human malignant mesothelioma cells. Biochem Biophys Res Commun 419: 529–536.
Yamochi T, Yamochi T, Aytac U, Sato T, Sato K, Ohnuma K, McKee KS, Morimoto C, Dang NH (2005) Regulation of p38 phosphorylation and topoisomerase IIα expression in the B-cell lymphoma line Jiyoye by CD26/dipeptidyl Peptidase IV is associated with enhanced in vitro and in vivo sensitivity to doxorubicin. Cancer Res 65: 1973–1983.
Acknowledgements
We thank Ms. Aya Miwa and Ms. Haruna Otsuka for excellent assistance with laboratory work, and Drs. Yukio Takeshima, Vishwa Jeet Amatya and Kouki Inai for histopathological examination and classification of the clinical tissues. This study is supported by Grant-in-Aid of The Ministry of Education, Science, Sports (KO and CM) and Culture, Ministry of Health, Labour, and Welfare, Japan (CM).
Author contributions
JY, RH, TO, EK, HY and SI performed the experiments, interpreted the data and assisted with the paper, KO and CM designed the research, interpreted the data and wrote the paper, NHD interpreted the data, assisted with the paper, and proofread the manuscript, and KA, TK and TY provided the clinical data and samples, performed the experiments, analysed pathological results, interpreted the data and assisted with the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
CM is an inventor of the humanised CD26 mAb, YS110 (US Patent #7402698). Y’s Therapeutics Co., Ltd owns this patent, and CM and NHD are founding members of this company.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Yamamoto, J., Ohnuma, K., Hatano, R. et al. Regulation of somatostatin receptor 4-mediated cytostatic effects by CD26 in malignant pleural mesothelioma. Br J Cancer 110, 2232–2245 (2014). https://doi.org/10.1038/bjc.2014.151
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.151
Keywords
This article is cited by
-
Serum soluble CD26/DPP4 titer variation is a potential prognostic biomarker in cancer therapy with a humanized anti-CD26 antibody
Biomarker Research (2021)
-
DPP8 is a novel therapeutic target for multiple myeloma
Scientific Reports (2019)
-
First-in-human phase 1 of YS110, a monoclonal antibody directed against CD26 in advanced CD26-expressing cancers
British Journal of Cancer (2017)
-
DPPIV/CD26: a tumor suppressor or a marker of malignancy?
Tumor Biology (2016)