Abstract
Background:
Recent evidence indicates that the host inflammatory response has an important role in the tumour progression. Elevated C-reactive protein (CRP) levels have been previously associated with poor prognosis in several cancer types including small-scale studies in pancreatic cancer (PC) patients. The purpose of the present study was to validate the prognostic impact of plasma CRP levels at date of diagnosis on cancer-specific survival (CSS) in a large cohort of PC patients.
Methods:
Data from 474 consecutive patients with adenocarcinoma of the pancreas, treated between 2004 and 2012 at a single centre, were evaluated retrospectively. CSS was analysed using the Kaplan–Meier method. To evaluate the prognostic significance of plasma CRP levels, univariate and multivariate Cox analyses were applied.
Results:
High plasma CRP levels at diagnosis were significantly associated with well-established prognostic factors, including high tumour stage and tumour grade and the administration of chemotherapy (P<0.05). In univariate analysis, we observed that a high plasma CRP level was a consistent factor for poor CSS in PC patients (hazard ratio (HR)=2.21; 95% confidence interval (CI)=1.68–2.92, P<0.001). In multivariate analysis, tumour stage, grade, administration of chemotherapy, a high neutrophil–lymphocyte ratio and the highest quartile of CRP levels (HR=1.60, 95% CI=1.16–2.21; P=0.005) were identified as independent prognostic factors in PC patients.
Conclusion:
In conclusion, we confirmed a significant association of elevated CRP levels with poor clinical outcome in PC patients. Our results indicate that the plasma CRP level might represent a useful marker for patient stratification in PC management.
Similar content being viewed by others
Main
Pancreatic cancer (PC) is a very aggressive tumour, which is reflected by the second most common cause of death from cancer within all gastrointestinal malignancies (Siegel et al, 2012). In more detail, the prognosis for PC has been nearly unchanged over the last 25 years, with an overall poor 5-year survival rate of only 1–4% (Richter et al, 2003). Despite developments in novel diagnostic techniques and modalities, the lack of early symptoms results in delayed diagnosis. The majority of patients initially diagnosed have locally advanced or metastatic disease and only approximately 15% of the patients are amenable to resection (Niederhuber et al, 1995). Adjuvant chemotherapy and palliative treatment have slightly improved the clinical outcome results and neoadjuvant treatment approaches are under clincial investigation (Sultana et al, 2012; Tinchon et al, 2013). Several prognostic factors have been identified that predict survival in PC patients, such as tumour size, histologic grade, vascular invasion, lymph node metastases and perineural invasion (Griffanti-Bartoli et al, 1994; Fortner et al, 1996; Ozaki et al, 1999; Raut et al, 2007). Nevertheless, the majority of these established histological predictors is only amenable for assessment after surgery. Other novel molecular biomarkers are associated with high costs, time-consuming procedures and laboratory efforts. Therefore, there is a clear need for the establishment of easily determinable and cheap pre-treatment prognostic markers that can be used for a better risk stratified treatment approach. Recent studies suggest that not only the intrinsic properties of tumour cells determine tumour spread, but also systemic factors, in the shape of cytokines and other chemical messengers, have an important role in cellular proliferation and the ability to metastasize (Coussens and Werb, 2002; Mantovani et al, 2008). C-reactive protein (CRP) is an acute phase protein produced by the liver as part of the systemic inflammatory response. Several studies have demonstrated a prognostic role of CRP in numerous cancer types including soft tissue sarcoma, small-cell lung cancer, renal cell cancer and colorectal cancer (Hashimoto et al, 2005; Karakiewicz et al, 2007; Nakamura et al, 2013). However, with respect to PC, the results are mainly derived from small-scale studies with controversially reported results (Falconer et al, 1995; Ueno et al, 2000; Jamieson et al, 2005; Tingstedt et al, 2007; Papadoniou et al, 2008; Pine et al, 2009; Garcea et al, 2011; Sanjay et al, 2012). In the present study, we aimed at validating the prognostic significance of pre-treatment plasma CRP levels on cancer-specific survival (CSS) in a large cohort of 474 PC patients.
Material and Methods
This retrospective analysis included data from 474 consecutive patients who were treated at the Division of Clinical Oncology, Medical University of Graz, between 2004 and 2012. All patients had histological confirmed pancreatic ductal adenocarcinoma and available CRP levels at the time of diagnosis. All clinico-pathological data were retrieved from medical records at the Division of Clinical Oncology, as well as from pathology records from the Institute of Pathology at the same institution.
As the TNM classification system for PC changed during the study period, tumour stages were uniformly adjusted according to the 7th edition of this system (Edge et al, 2010). Other documented clinico-pathological parameters included administration of chemotherapy with gemcitabine, gender and age. The laboratory data, CRP levels, bilirubin levels, numbers of neutrophils, lymphocytes and platelets were obtained by exploration within 7 days before treatment or histological-proven diagnosis. The neutrophil–lymphocyte ratio (NLR) and the platetlet–lymphocyte ratio (PLR) were calculated as previously described (Wang et al, 2012). Based on our previously published smaller study, a NLR of >3.25 was selected as the cutoff value for validation (Stotz et al, 2013). In addition, we evaluated the prognostic value of the PLR as previously described (Proctor et al, 2011; Wang et al, 2012). PLR was categorised into three groups according to previously published cutoff values (Wang et al, 2012). Follow-up evaluations were performed every 3 months within the first 3 years, 6 months for 5 years and annually thereafter for curative resected tumour stages. For deceased patients, dates of death were obtained from the central registry of the Austrian Bureau of Statistics or telephone calls to their families. A complete follow-up was available for all patients in this retrospective analysis. The study was approved by the local ethical committee of the Medical University of Graz (No. 25-458 ex 12/13).
Statistical analyses
Cancer-specific survival was defined as the time (in months) from date of surgery or date of histological-proven diagnosis to cancer-related death. The association between the plasma CRP levels and clinico-pathological parameters was evaluated by non-parametric tests (Mann–Whitney U and χ2 test). We seek an ideal cutoff value for the continuous CRP variable by applying receiver operating curve analysis as previously reported (Absenger et al, 2013). Patients’ clinical end point was calculated using the Kaplan–Meier method and compared by the log-rank test. Backward stepwise multivariate Cox proportion analysis was performed to determine the influence of different clinico-pathological parameters and plasma CRP levels on CSS. Hazard ratios (HRs) estimated from the Cox analysis were reported as relative risks with corresponding 95% confidence intervals (CIs). All statistical analyses were performed using the Statistical Package for Social Sciences version 20.0 (SPSS Inc., Chicago, IL, USA). A two-sided P<0.05 was considered statistically significant.
Results
Overall, 256 male and 218 female patients with PC were included in the study cohort. The mean age at diagnosis was 64.6±10.4 years. Median survival was 7 months (range: 0–79 months) and 406 (85.7%) patients died by their most recent follow-up visit. The tumour stage was defined as stage I in 5 (1%) patients, stage IIa in 18 (3.8%) patients, stage IIb in 85 (17.9%) patients, stage III in 33 (7%) patient and stage IV in 333 (70.3%) patients. Three hundred and forty-five (72.6%) patients received a chemotherapy. Of the 474 patients, 126 (26.6%) underwent a tumour resection, 93 (19.6%) patients underwent a laparoscopic/laparotomy and consecutive biopsy and 255 (53.8%) were diagnosed by fine needle biopsy.
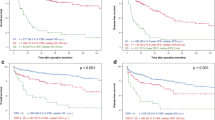
The mean pre-treatment plasma CRP level was 23.2±36 mg l−1. In an attempt to test whether increasing CRP levels influence the clinical outcome of PC patients, we first subdivided the patients into four groups according to their CRP levels. Kaplan–Meier curves for CSS, which comprises groups according to quartiles of the CRP levels are shown in Figure 1. Pairwise log-rank test indicates significant differences between the highest quartile (plasma CRP level >27.1 mg l−1) compared with the lowest (0–2.4 mg l−1; P<0.001), low (2.1–7.5 mg l−1; P<0.001) and third (7.5–27.1 mg l−1, P<0.001) quartiles. After performing receiver operating curve analysis, an optimal cutoff value of >4.5 mg l−1 (area under the curve: 0.59, 95% CI: 0.54–0.62) was identified to differentiate between survival and death. Consequently, we separated patients into two groups according to low CRP levels (<4.5 mg l−1) or high CRP levels (⩾4.5 mg l−1) and tested the associations between preoperative plasma CRP levels and other clinical-pathological factors. An elevated plasma CRP level significantly correlated with high tumour stage, unresectable tumours, poor Karnofsky index, high NLR, high PLR and elevated bilirubin (P<0.05), whereas no association with age, gender, tumour grading, administration of chemotherapy could be found (Table 1).
To investigate whether plasma CRP level and other clinical-pathological factors are associated with clinical outcome of PC patients, univariate and multivariate Cox proportional models for CSS were calculated. Among the 474 PC patients, death occured in 134 of 177 (77.9%) patients with a low plasma CRP level and in 272 of 302 (90.1%) patients with a high plasma CRP level (P<0.001). Figure 2 shows the Kaplan–Meier curves for CSS and reveals that a high plasma CRP level is a consistent factor for poor prognosis in PC patients (P<0.001, log-rank test).
Univariate analysis identified older age (<65 vs ⩾65 years, P=0.011), a high tumour stage (stage I+II vs III vs IV, P<0.001), a high tumour grade (G1, G2 vs G3, G4, P=0.011), no administration of chemotherapy (chemotherapy vs no treatment, P<0.001), no surgical resection (P<0.001), a high NLR (P<0.001) and a high plasma CRP level (P<0.001) as poor prognostic factors for CSS in this study cohort. Gender, PLR and elevated bilirubin levels were not significantly associated with clinical outcome (Table 2).
To determine the independent prognostic value of the plasma CRP levels for CSS, a multivariate analysis using a Cox proportional hazard model was performed. In the multivariate analysis that included age, gender, tumour grade, tumour stage, administration of chemotherapy, surgical resection, NLR, PLR, bilirubin levels and plasma CRP levels, we identified tumour grade, tumour stage, administration of chemotherapy, high NLR and plasma CRP level within the highest quartile as independent prognostic factors for CSS (HR=1.60, 95% CI=1.16–2.21; P=0.005; Table 2).
Discussion
In the present study, we confirmed an association between elevated CRP levels at the time of PC diagnosis and decreased CSS on a large cohort of patients with PC. Many efforts have been previously made to investigate the relationship between CRP and prognosis in various types of cancer (Hashimoto et al, 2005; Karakiewicz et al, 2007; Nakamura et al, 2013). Regarding PC, the previously reported data are conflicting and mainly relies on small-scale studies. An early study conducted by Falconer et al (1995) proposed a prognostic value for elevated CRP levels (>10 mg l−1) in 102 patients with unresectable PC. Ueno et al (2000) found an independent prognostic significance for elevated CRP (>5 mg l−1) in 103 metastatic PC patients. In a smaller study, including 65 patients with surgically resected PC, Jamieson et al (2005) reported that patients with elevated (>10 mg l−1) post-operative CRP values had a poor clinical outcome. Papadoniou et al (2008) retrospectively evaluated 215 patients and showed that elevated plasma CRP was an independent factor of poor prognostic outcome in patients with advanced or metastatic PC. Pine et al (2009) reported in 199 patients that raised plasma CRP concentration (>5 mg l−1) at the time of presentation of advanced PC carries a poor prognosis independent of biliary tract obstruction.
In line with these findings, Tingstedt et al (2007) reported that raised plasma CRP concentrations (⩾5 mg l−1) were independently associated with decreased overall survival in 119 PC patients. Furthermore, in a smaller study including 51 patients from Japan, elevated preoperative plasma CRP levels (>3 mg l−1) were demonstrated to predict poor prognosis in patients undergoing curative resection for PC (Sanjay et al, 2012). In contrast to these mentioned studies, in a recent report by Garcea et al (2011), no association between plasma CRP levels and tumour recurrence was identified in 74 PC patients. However, many of these studies included rather small number of investigated cases and differ in terms of inclusion criteria and clinical end points. In our study, we validated the prognostic impact of plasma CRP levels on CSS as the end point and clearly demonstrated that an elevated plasma CRP level was independently associated with CSS in a large cohort of 316 PC patients. In our study, which is currently the largest one reported, we found also an association of elevated CRP levels and other clinico-pathological parameters. Regarding this association, different factors might explain the prognostic value of CRP. For instance, a higher tumour stage can lead to a greater extend of systemic inflammation by secretion of cytokines and release of tumour-degradation products, which in turn increase the CRP production in the liver. The association with elevated bilirubin levels and reduced Karnofsky index also indicate to a higher rate of PC-related cholestasis/cholangitis and impaired performance status in patients with high CRP levels. Thus, elevated CRP levels can be regarded as a surrogate biomarker for poor tumour biology as well as adverse individual-related medical conditions. Besides the role of CRP as a simply indicative circulating biomarker, its independent prognostic role might also be explained by its discrete influence on tumour progression. In this context, a number of theories have been postulated to explain why an elevated plasma CRP level could influence the biological properties of cancer cells. Previous studies indicate that tumour cells recruit endothelial cells, fibroblasts and inflammatory cells into the tumour bed to shape their unique microenvironment. The inflammatory response to tumour cells, reflected by an elevated plasma CRP level, results in a tumour microenvironment enriched with proinflammatory cytokines, angiogenic and lymphogenic factors and chemokines that promote tumour growth, angiogenesis and metastasis (Coussens and Werb, 2002; Miki et al, 2004). Alternatively, elevated plasma CRP may represent a response secondary to tumour necrosis and local tissue damage, which is caused by the tumour–host cell interaction and reflects a high tumour burden (McMillan et al, 2003). On the other hand, IL-6 may also indirectly help the binding of CRP to phospholipides on tumour cells, activating the complement system and acting as an opsonin, augmenting tumour cell phagocytosis (Black et al, 2004). Thus, CRP may not only represent a response to tumour microenvironment, but also contribute to opsonisation and elimination of tumour cells. Taken together, CRP has a fundamental role in a wide range of inflammatory processes and provides a link between the innate and adaptive immune system.
There are a few limitations to the present study. CRP is known to be a non-specific marker of inflammation, and it is also possible that the presence of other systemic diseases could influence CRP concentrations in the plasma. Furthermore, for head of pancreas tumours the associated clinical condition of jaundice (with an associated bactobilia) may be a confounding factor in assessing CRP levels but we were not able to evaluate this feature in our study. Moreover, our study is limited by its retrospective nature and a heterogenous group of patients. Based on the results of our study, one can propose that higher CRP levels at the date of diagnosis of PC are associated with a higher risk for earlier death because of the disease. Whether patients can be selected for resection or increase the chances of curative resection can only be evaluated in a controlled prospective clinical trial. However, to the best of our knowledge, our study represents to date the largest one validating the prognostic value of plasma CRP levels in PC patients.
In conclusion, in the present study, elevated CRP levels before initial treatment were demonstrated to represent a poor prognostic factor for CSS in PC patients. This simple, highly repitable, inexpensive and easily available marker shows a potential to select patients at high risk for poor clinical outcome for appropriate treatment strategies.
Change history
07 January 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Absenger G, Szkandera J, Pichler M, Stotz M, Arminger F, Weissmueller M, Schaberl-Moser R, Samonigg H, Stojakovic T, Gerger A (2013) A derived neutrophil to lymphocyte ratio predicts clinical outcome in stage II and III colon cancer patients. Br J Cancer 109: 395–400.
Black S, Kushner I, Samols D . C-reactive Protein (2004) J Biol Chem 279: 48487–48490.
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420: 860–867.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (2010) Exocrine and endocrine pancreas. In: AJCC Cancer Staging Manual 7th edn, pp 241–249. Springer: New York.
Falconer JS, Fearon KC, Ross JA, Elton R, Wigmore SJ, Garden OJ, Carter DC (1995) Acute-phase protein response and survival duration of patients with pancreatic cancer. Cancer 75: 2077–2082.
Fortner JG, Klimstra DS, Senie RT, Maclean BJ (1996) Tumor size is the primary prognosticator for pancreatic cancer after regional pancreatectomy. Ann Surg 223: 147–153.
Garcea G, Ladwa N, Neal CP, Metcalfe MS, Dennison AR, Berry DP (2011) Preoperative neutrophil-to-lymphocyte ratio (NLR) is associated with reduced disease-free survival following curative resection of pancreatic adenocarcinoma. World J Surg 35: 868–872.
Griffanti-Bartoli F, Arnone GB, Ceppa P, Ravera G, Carrabetta S, Civalleri D (1994) Malignant tumors in the head of the pancreas and the periampullary region. Diagnostic and prognostic aspects. Anticancer Res 14: 657–666.
Hashimoto K, Ikeda Y, Korenaga D, Tanoue K, Hamatake M, Kawasaki K, Yamaoka T, Iwatani Y, Akazawa K, Takenaka K (2005) The impact of preoperative serum C-reactive protein on the prognosis of patients with hepatocellular carcinoma. Cancer 103: 1856–1864.
Jamieson NB, Glen P, McMillan DC, McKay CJ, Foulis AK, Carter R, Imrie CW (2005) Systemic inflammatory response predicts outcome in patients undergoing resection for ductal adenocarcinoma head of pancreas. Br J Cancer 92: 21–23.
Karakiewicz PI, Hutterer GC, Trinh QD, Jeldres C, Perrotte P, Gallina A, Tostain J, Patard JJ (2007) C-reactive protein is an informative predictor of renal cell carcinoma-specific mortality: a European study of 313 patients. Cancer 110: 1241–1247.
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454: 436–444.
McMillan DC, Canna K, McArdle CS (2003) Systemic inflammatory response predicts survival following curative resection of colorectal cancer. Br J Surg 90: 215–219.
Miki C, Konishi N, Ojima E, Hatada T, Inoue Y, Kusunoki M (2004) C-reactive protein as a prognostic variable that reflects uncontrolled up-regulation of the IL-1-IL-6 network system in colorectal carcinoma. Dig Dis Sci 49: 970–976.
Nakamura T, Grimer R, Gaston C, Francis M, Charman J, Graunt P, Uchida A, Sudo A, Jeys L (2013) The value of C-reactive protein and comorbidity in predicting survival of patients with high grade soft tissue sarcoma. Eur J Cancer 49: 377–385.
Niederhuber JE, Brennan MF, Menck HR (1995) The National Cancer Data Base report on pancreatic cancer. Cancer 76: 1671–1677.
Ozaki H, Hiraoka T, Mizumoto R, Matsuno S, Matsumoto Y, Nakayama T, Tsunoda T, Suzuki T, Monden M, Saitoh Y, Yamauchi H, Ogata Y (1999) The prognostic significance of lymph node metastasis and intrapancreatic perineural invasion in pancreatic cancer after curative resection. Surg Today 29: 16–22.
Papadoniou N, Kosmas C, Gennatas K, Polyzos A, Mouratidou D, Skopelitis E, Tzivras M, Sougioultzis S, Papastratis G, Karatzas G, Papalambros E, Tsavaris N (2008) Prognostic factors in patients with locally advanced (unresectable) or metastatic pancreatic adenocarcinoma: a retrospective analysis. Anticancer Res 28: 543–549.
Pine JK, Fusai KG, Young R, Sharma D, Davidson BR, Menon KV, Rahman SH (2009) Serum C-reactive protein concentration and the prognosis of ductal adenocarcinoma of the head of pancreas. Eur J Surg Oncol 35: 605–610.
Proctor MJ, Morrison DS, Talwar D, Balmer SM, O'Reilly DS, Foulis AK, Horgan PG, McMillan DC (2011) An inflammation-based prognostic score (mGPS) predicts cancer survival independent of tumour site: a Glasgow Inflammation Outcome Study. Br J Cancer 104 (4): 726–734.
Raut CP, Tseng JF, Sun CC, Wang H, Wolff RA, Crane CH, Hwang R, Vauthey JN, Abdalla EK, Lee JE, Pisters PW, Evans DB (2007) Impact of resection status on pattern of failure and survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Ann Surg 246: 52–60.
Richter A, Niedergethmann M, Sturm JW, Lorenz D, Post S, Trede M (2003) Long-term results of partial pancreaticoduodenectomy for ductal adenocarcinoma of the pancreatic head: 25-year experience. World J Surg 27: 324–329.
Sanjay P, de Figueiredo RS, Leaver H, Ogston S, Kulli C, Polignano FM, Tait IS (2012) Preoperative serum C-reactive protein levels and post-operative lymph node ratio are important predictors of survival after pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. JOP 13: 199–204.
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62: 10–29.
Stotz M, Gerger A, Eisner F, Szkandera J, Loibner H, L Ress A, Kornprat P, A Zoughbi W, Seggewies FS, Lackner C, Stojakovic T, Samonigg H, Hoefler G, Pichler M (2013) Increased neutrophil-lymphocyte ratio is a poor prognostic factor in patients with primary operable and inoperable pancreatic cancer. Br J Cancer 109 (2): 416–421.
Sultana A, Cox T, Ghaneh P, Neoptolemos JP (2012) Adjuvant therapy for pancreatic cancer. Recent Results Cancer Res 196: 65–88.
Tinchon C, Hubmann E, Pichler A, Keil F, Pichler M, Rabl H, Uggowitzer M, Jilek K, Leitner G, Bauernhofer T (2013) Safety and efficacy of neoadjuvant FOLFIRINOX treatment in a series of patients with borderline resectable pancreatic ductal adenocarcinoma. Acta Oncol 52 (6): 1231–1233.
Tingstedt B, Johansson P, Andersson B, Andersson R (2007) Predictive factors in pancreatic ductal adenocarcinoma: role of the inflammatory response. Scand J Gastroenterol 42: 754–759.
Ueno H, Okada S, Okusaka T, Ikeda M (2000) Prognostic factors in patients with metastatic pancreatic adenocarcinoma receiving systemic chemotherapy. Oncology 59: 296–301.
Wang DS, Luo HY, Qiu MZ, Wang ZQ, Zhang DS, Wang FH, Li YH, Xu RH (2012) Comparison of the prognostic values of various inflammation based factors in patients with pancreatic cancer. Med Oncol 29 (5): 3092–3100.
Acknowledgements
This study was supported by funds of the ‘Oesterreichische Nationalbank’ (Anniversary Fund, project number: 14320 to Gerald Hoefler).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Szkandera, J., Stotz, M., Absenger, G. et al. Validation of C-reactive protein levels as a prognostic indicator for survival in a large cohort of pancreatic cancer patients. Br J Cancer 110, 183–188 (2014). https://doi.org/10.1038/bjc.2013.701
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.701
Keywords
This article is cited by
-
C-reactive protein/albumin ratio is the most significant inflammatory marker in unresectable pancreatic cancer treated with FOLFIRINOX or gemcitabine plus nab-paclitaxel
Scientific Reports (2023)
-
Pancreatic fibrosis, acinar atrophy and chronic inflammation in surgical specimens associated with survival in patients with resectable pancreatic ductal adenocarcinoma
BMC Cancer (2022)
-
Effect of exercise on pancreatic cancer patients during treatment: a scoping review of the literature
Supportive Care in Cancer (2022)
-
Pancreatic cancer survival prediction via inflammatory serum markers
Cancer Immunology, Immunotherapy (2022)
-
Apolipoprotein A1 is negatively associated with male papillary thyroid cancer patients: a cross-sectional study of single academic center in China
BMC Endocrine Disorders (2021)