Abstract
Background:
The purpose of this study was to evaluate the efficacy of superselective cisplatin infusion with concomitant radiotherapy (RADPLAT) for previously untreated patients with the squamous cell carcinoma of maxillary sinus (SCC-MS).
Methods:
Between 1999 and 2010, 54 patients were given superselective intra-arterial infusions of cisplatin (100–120 mg m−2 per week) with simultaneous intra-venous infusions of thiosulfate to neutralise cisplatin toxicity and conventional radiotherapy (65–70 Gy).
Results:
One patient (1.9%) was diagnosed with T2, 14 (25.9%) with T3, 27 (50%) with T4a, and 12 (22.2%) with T4b disease. Lymph-node involvement was present in 12 patients (22.2%). During the median follow-up period of 6.4 years, the 5-year local progression-free and overall survival rates were 65.8 and 67.9% for all patients, respectively. No patient died as a result of treatment toxicity or experienced a cerebrovascular accident. Osteonecrosis (n=5), brain necrosis (n=1), and ocular/visual problems (n=14) were observed as late adverse reactions.
Conclusion:
We have shown excellent overall survival and local progression-free rate in SCC-MS patients treated by RADPLAT with acceptable rates of acute and late toxicity. A multi-institutional trial is needed to prove that this strategy is a feasible and effective approach for the treatment of SCC-MS.
Similar content being viewed by others
Main
Malignant tumours of the maxillary sinus are rare neoplasms that constitute ∼70% of all malignancies of the paranasal sinuses and nasal cavity, although such malignancies account for only 3% of head and neck carcinomas and as little 0.5% of all malignant diseases (Muir and Nectoux, 1980).
Due to anatomic limitations in the early diagnosis and the absence of symptoms in early-stage disease, a large proportion of maxillary sinus cancers are advanced at the time of initial presentation. Most advanced cases require the radical surgery with or without a complete resection of the orbital contents; however, this results in a significant disfigurement and impairment of function.
Chemoradiotherapy (CRT) is the treatment of choice for locally advanced laryngeal and pharyngeal squamous cell carcinoma (SCC). However, CRT does not necessarily lead to satisfactory treatment outcomes in cases of maxillary sinus cancer (Jang et al, 2010; Kang et al, 2012). Recently, the superselective intra-arterial (IA) infusion of high-dose cisplatin with concomitant radiotherapy (hereafter RADPLAT) has been performed for the patients with locally advanced sinonasal cancer in several institutions and has been reported to result in a favourable survival rate (Samant et al, 2004; Shiga et al, 2007; Homma et al, 2009; Kanoto et al, 2010).
Our previous study (Homma et al, 2009) included non-SCC and non-maxillary sinus cancer, so the treatment results obtained using RADPLAT for SCC of the maxillary sinus (SCC-MS), which is the most common sinonasal cancer, were unclear. Therefore, we increased the number of and focussed on patients with SCC-MS treated by RADPLAT as the definitive treatment in this study.
Patients and methods
Eligibility criteria
Eligible patients had to be no older than 75 years and had to have a World Health Organization performance status of 0–2, adequate bone marrow reserve, and adequate liver and renal function. All patients provided written informed consent for this study, which was approved by the institutional review board of the school of medicine, Hokkaido University (Sapporo, Japan). Patients who were pregnant or breast-feeding were excluded from the study. Patients also required histologic proof of SCC-MS for inclusion. All patients were initially evaluated by a multi-disciplinary team consisting of head and neck surgeons and radiation oncologists, and tumours were classified according to the 7th Edition of the Union for International Cancer Control (UICC) staging system. The stage of the tumour was determined on the basis of patient history, physical examination, chest X-rays, as well as computed tomography (CT) and/or magnetic resonance imaging (MRI). Patients either had disease for which radical surgery was contraindicated or had rejected radical surgery. Patients were excluded if they had distant metastases (M1) or had received prior treatment of any kind for their cancer.
Chemotherapy
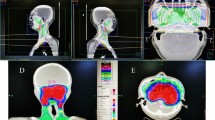
All patients received concurrent IA cisplatin and intra-venous (IV) sodium thiosulfate infusions as follows: cisplatin (100–120 mg m−2 per week for 4 weeks) was infused through a microcatheter placed angiographically to selectively encompass only the dominant blood supply of the targeted tumour using selective IA computed tomographic arteriography. Tumours of the maxillary sinuses are usually fed by the internal maxillary artery, but in cases when the facial artery, transverse facial artery, or ascending pharyngeal artery fed the tumour, part of the dose was administered through these alternative arteries. Selective IA-CT angiography was performed to correctly and carefully identify the feeding arteries and their perfusion. The dose of cisplatin infused from each artery was determined by IA-CT angiography as described in our previous report (Homma et al, 2009). Simultaneously, sodium thiosulfate (20–24 g) was given IV, as described by Robbins, to neutralise the cisplatin (Robbins et al, 2000). All arterial catheterisations were accomplished transcutaneously through the femoral artery, and the catheters were removed immediately after infusion. To ensure that patients excreted the cisplatin rapidly, 8 l of lactated Ringer’s solution was given over a 24-h period. A 5HT3-receptor antagonist was given to all patients before arterial infusion to minimise nausea and vomiting. Chemotherapy was completed during the first 4 weeks, provided that patients responded well during the early treatment period and had received three arterial infusions.
Radiotherapy
All patients received conventional radiotherapy using a 4-megavolt or 6-megavolt X-ray linear accelerator. The irradiation treatment volume included the entire maxilla, ethmoid sinus, ipsilateral nasal cavity, and pterygopalatine fossa. For patients with tumours extending to the orbita, this area was also treated, but efforts were made to spare the lacrimal gland. Until May 2006, the irradiation schedule was 65 Gy in 26 fractions over 6.5 weeks. From that time, it was changed to 70 Gy in 35 fractions over 7 weeks for all patients with advanced head and neck cancer. The treatment volume was reduced to 40 Gy for cases with a low possibility of tumour extension to adjacent structures, such as the ethmoid sinus or orbita.
A modified 45-wedged pair technique was used, in which the lateral beams were tilted ∼10° anteriorly with the hope of reducing the risk of temporal lobe necrosis. Multi-leaf collimators were also used for this purpose and to reduce the dose to other critical structures, such as the optic chiasma and contralateral eye. For patients with lymph-node metastases, the ipsilateral neck was irradiated (40 Gy) using an anterior–posterior field and a 25–30 Gy boost was given to the positive nodes. A thermo-plastic mask was used for immobilisation for all patients. CT and MRI were performed in the same position using the mask so that accurate diagnosis of the extent of the tumour could be made. The treatment was planned with a CT simulator and a three-dimensional dose calculation computer. The dose to the spinal cord was kept below 40 Gy in all instances.
Management of the neck
Patients with regional lymph-node metastasis of the neck were treated with 65–70 Gy of radiotherapy and chemotherapy. If lymph-node metastases remained or recurred, then patients with resectable neck disease were referred for dissection.
Evaluation of response and toxicity
Responses were evaluated by clinical examination, together with CT and/or MRI studies 6–8 weeks after the completion of therapy. A complete response was defined as a total resolution of the tumour. As it is difficult to differentiate between radiographic changes related to the treatment and scar tissue from persisting tumours, treatment response itself reflects this uncertainly. Over time, scar tissue remains stable, but persistent tumour tissue will progress, so a patient with radiologic changes that remained stable and with no signs or symptoms of disease was considered to be ‘progression free’. As for PET-CT, it is not always useful in distinguishing between inflammation and persistent disease, particularly in sinonasal cancer after RADPLAT. We, therefore, used PET-CT only as a guide. A biopsy was performed only to document recurrence, if indicated. All toxicities encountered during therapy were evaluated according to the Common Terminology Criteria for Adverse Events v3.0 (2003).
Statistical analysis
The major end point of the study was overall survival. Additional end points included local progression-free rate and toxicity. All patients were closely observed during the follow-up period, the median of which was 6.4 years (range 2.7–13 years).
In this study, the detailed anatomical sites in which the primary tumour developed were evaluated by CT and MRI. The local extension sites were classified according to the 7th UICC staging system.
Cases of persistent or recurrent primary or neck disease after the completion of RADPLAT were considered to be local or regional failures, regardless of whether salvage was successful. Patients who did not receive a full dose of radiation therapy and then underwent surgery were treated as local failures. Probabilities of overall survival, which included death from any cause, and local progression-free rates computed from the beginning of treatment to the time of local relapse, were calculated by the Kaplan–Meier method and compared using the log-rank test. The level of statistical significance was set at P<0.05. Statistical analysis was performed using the JMP Pro 10.0.0 statistical software (SAS Institute, Cary, NC, USA).
Results
Patient characteristics
Fifty-four patients were enrolled in this study between October 1999 and December 2010, and treated by RADPLAT at Hokkaido University Hospital (Sapporo, Japan). Patients consisted of 43 males and 11 females, with a median age of 60 years (range 35–74 years). During the same period as this study, seven patients with SCC-MS, all staged as T3N0M0, were treated by surgical therapy. All of them received eye-sparing surgery. A further nine patients were treated by radiotherapy alone (six patients) or radiotherapy with IV chemotherapy (three patients). As the majority of them showed a poor general condition and were considered as medically unfit to receive RADPLAT and surgery. Some patients did not want to receive either RADPLAT or surgery.
T and N classifications are shown in Table 1. One patient (1.9%) was diagnosed with T2, 14 (25.9%) with T3, 27 (50%) with T4a, and 12 (22.2%) with T4b disease. Lymph-node involvement was present in 12 patients (22.2%). Intensity Modulated Radiotherapy was employed for one patient to avoid exposing the eyeball and optic nerve of the unaffected side to radiation.
Compliance
RADPLAT was feasible (three or four infusions of IA cisplatin and a full dose of radiation therapy within 7 days of treatment interruptions) in 49 patients (90.7%). Three patients received one or two courses of IA chemotherapy. Of these, one received a full dose of radiation therapy, but his radiotherapy was interrupted for 30 days due to sepsis and poor general condition. The other two patients received 50 Gy of radiation therapy due to severe drug eruption or ischaemic enteritis. The patient then underwent total maxillectomy. One patient refused additional treatment and radiotherapy was stopped after four courses of IA chemotherapy and 48 Gy of radiotherapy. The remaining tumour was removed by endonasal resection. In the remaining patient, ipsilateral retinal detachment developed during therapy. Radiotherapy was stopped after 8 days and he underwent retinal detachment surgery.
Toxicity
Although the treatment regimen was intensive, acute toxicity was manageable in most patients (Table 2) and none died as a result of treatment toxicity. Thirty-nine patients (72.2%) experienced grade III to IV toxicity. Non-haematologic side effects included mucositis (n=19) and nausea/vomiting (n=11). No patient experienced a cerebrovascular accident. Haematologic toxicity consisted of leukopaenia (n=18), anaemia (n=6), and thrombocytopaenia (n=1). No surviving patients required feeding-tube support after therapy.
Osteonecrosis, brain necrosis, and ocular/visual problems occurred as late adverse reactions. Five patients experienced osteonecrosis, including four cases involving the maxilla, and one involving the mandible. One patient with grade 3 mandibular necrosis required reconstruction of the mandible with a free flap transfer. Another patient with grade 3 maxillary necrosis required total maxillectomy and reconstruction of the maxilla with a free flap transfer. The remaining three patients suffered from grade 2 osteonecrosis, which was manageable with minor sequestrectomy. One patient suffered from brain necrosis without sequelae.
Severe ocular/visual problems (grade 3/4) occurred in 14 of the 40 patients who were followed-up over 2 years without residual or recurrent primary disease. Severe ocular/visual problems occurred in 11 (55%) of 20 patients who were considered for orbital exenteration if the need for radical surgery was indicated. On the contrary, severe ocular/visual problems occurred in 3 (15%) of 20 patients who were not considered for orbital exenteration if the need for radical surgery was indicated.
Local progression-free and overall survival rates
The 5-year local progression-free rate was 65.8% for all patients (n=54), 75.8% for patients with T2-3 disease (n=15), 62.5% for patients with T4a disease (n=27), and 59.7% for patients with T4b disease (n=12, Figure 1). The 5-year overall survival was 67.9% for all patients, 80% for patients with T2-3 disease (n=15), 66.8% for patients with T4a disease (n=27), and 57.1% for patients with T4b disease (n=12, Figure 2).
No statistically significant differences were noted in overall survival and local progression-free rate among T stages and local extension sites. Patients with lymph-node metastasis had a worse overall survival rate than those without lymph-node metastasis, and males had a worse local progression-free rate than females. Further, differences in local progression-free rates were observed between patients by age, lymph-node metastasis, hard palate involvement, and subcutaneous tissue invasion, but the differences were not statistically significant (Table 3).
Response of the primary disease
Of the 54 patients enrolled in the treatment programme, complete response at the primary site was obtained in 30 (55.6%). However, the primary disease has been well controlled by RADPLAT in 38 patients to date. The remaining 16 patients had persistent or recurrent primary disease after the completion of RADPLAT.
Response of neck disease
Among the 12 patients with positive neck disease, 8 were well controlled by RADPLAT without surgery until the final follow-up. Four patients underwent a neck dissection after treatment for suspicious residual lymph nodes. As a result, three of four patients were treated successfully by salvage neck dissection. Four patients classified as N0 before therapy developed neck metastases after RADPLAT; of these, three were treated successfully by salvage neck dissection. In the remaining one patient, neck disease and distant metastasis developed simultaneously so that he was not able to undergo neck dissection. He was treated, instead, by systemic chemotherapy.
Pattern of relapse
The site of first recurrence (or residual disease) was identified wherever possible. Recurrence first occurred at the primary site in 16 patients. Of these, 12 underwent salvage surgery, and 8 patients were successfully salvaged. Neck recurrence occurred in eight patients. Of these, six patients were treated successfully by salvage neck dissection. Distant metastasis was found in two patients without primary or neck recurrence. Three patients died of other causes without disease.
Discussion
The standard of care for advanced maxillary sinus cancer is considered to be radical surgery followed by postoperative radiotherapy. Despite such radical therapy, the oncologic outcomes in terms of survival and disease control are not satisfactory. In addition, not a few patients present with unresectable disease. Such cases are expected to have a very poor outcome. There have been few reports of treatment outcomes focussed on SCC-MS as it is a rare disease. Bhattacharyya reported cases of maxillary sinus malignancies for the period from 1988 to 1998 extracted from the Surveillance, Epidemiology and End Results database. The 5-year survival of 401 cases of SCC-MS identified was reported to be 29.2% (Bhattacharyya, 2003). Bristol reviewed the data for 146 patients with maxillary sinus cancer treated for cure with surgery and postoperative radiotherapy between 1969 and 2002. The 5-year survival of 89 cases of SCC-MS was reported to be 49% (Bristol et al, 2007). Jang analysed the treatment results of definitive radiotherapy with or without chemotherapy in a group of 30 patients with T3-4 SCC-MS. The 5-year overall survival and local control rates were reported to be 34 and 29%, respectively (Jang et al, 2010).
RADPLAT has also been shown to be a promising treatment (Robbins, 2000; Homma et al, 2005), achieving a 90% complete response rate in advanced cases of head and neck cancer (Robbins et al, 2000). The treatment programme incorporates a novel technique for infusing cisplatin directly into the tumour bed, while minimising the effects of the drug systemically. On the basis of the promising results for RADPLAT reported by Robbins, a randomised trial was conducted in the Netherlands comparing RADPLAT with IV CRT (Rasch et al, 2010). Two hundred and thirty-six patients with (functional) inoperable head and neck cancer were randomly assigned to receive radiotherapy (70 Gy/35 f/7 weeks) combined with either four courses of IA cisplatin infusion on days 2, 9, 16, and 23 or IV cisplatin on days 1, 22, and 43. Results showed no significant differences in the locoregional control and overall survival. Renal toxicity was lower and neurological toxicity was higher in the IA arm. This trial failed to show any positive effect on survival and locoregional control compared with IV CRT.
The keys to success with IA chemotherapy are the angiographic technique and the appropriate infusion of cisplatin into the tumour. However, the paper made no mention of these factors. Thus, we did not know where or how the cisplatin was administered IA, although it would influence the treatment outcome. We speculate that there were some issues regarding the angiographic technique.
However, in an unplanned subgroup analysis, they found that there were significantly higher local control rates for IA treatment for large (>30 ml) lateralised tumours. Maxillary sinus cancer is generally large and lateralised, although the Dutch trial did not include maxillary sinus cancer. Thus, it appears to be suited for treatment with RADPLAT therapy. Indeed, several good results achieved by the use of RADPLT have been reported (Samant et al, 2004; Shiga et al, 2007; Homma et al, 2009; Kanoto et al, 2010).
The advantages of RADPLAT as a definitive treatment are that patients can avoid major surgery and can expect improved survival rates based on the results of this study. The 5-year overall survival rate of 67.9% observed for all patients, particularly that of 57.1% for those with T4b disease, was comparable to or better than those previously reported (Waldron et al, 2000; Bristol et al, 2007; Hoppe et al, 2008; Jang et al, 2010; Kang et al, 2012). Further, most advanced cases require radical surgery such as total maxillectomy or a craniofacial resection with or without a complete resection of the orbital contents; however, such interventions result in a significant disfigurement and impairment of function. Most of our patients were concerned about facial deformities after surgery, and understood the possibility of late complications, such as eye-related complications, after therapy and preferred RADPLAT. Indeed, during the same period as this study, seven patients with SCC-MS, all staged as T3N0M0, were treated by surgical therapy. Their facial deformities after surgery were expected to be acceptable and they consented to undergo surgery. No T4 patients elected to undergo surgery.
Patients with tumours invading the orbital fat, orbital musculature, or involving the orbital apex usually require orbital content extirpation if surgery is indicated (Wong and Kraus, 2001). Eye-related complications occurred in 55% of such patients in this study, although this rate is considered as acceptable. However, efforts should be made to spare vision and to avoid complications through the use of treatments such as intensity modulated radiation therapy and heavy particle radiation therapy.
The primary tumour extent has been reported to correlate with the clinical outcome in terms of overall survival and local control, regardless of treatment type (Waldron et al, 2000; Dirix et al, 2007). However, there were no statistically significant local extension sites affecting survival and local control in this study. This could be due to the fact that the arterial infusion of the tumour was performed appropriately. Nevertheless, patients with lymph-node involvement had a worse overall survival than those without lymph-node involvement, which is in agreement with previous reports (Waldron et al, 2000; Dirix et al, 2007). We have to reconsider the strategy for such patients, such as the inclusion of adjunct chemotherapy.
IMRT is useful for all base-of-skull tumours to improve dose delivery to the tumour and to spare normal tissue, particularly vital organs such as spinal cord, brain stem, and chiasma. We have, therefore, used IMRT for sinonasal cancer recently, and expect the incidence of late complications of radiotherapy to decrease in the future, although we did not use IMRT in this study period because of limited resources.
In conclusion, we have shown excellent overall survival and local progression-free rates, together with acceptable acute and late toxicity, in patients with SCC-MS treated by RADPLAT. We believe that RADPLAT is a useful treatment for suitable patients, such as patients with SCC-MS, although RADPLAT did not show better results than IV CRT in the previous Dutch trial. Therefore, we are now planning a multi-institutional trial of RADPLAT for locally advanced SCC-MS.
Change history
10 December 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bhattacharyya N (2003) Factors affecting survival in maxillary sinus cancer. J Oral Maxillofac Surg 61: 1016–1021.
Bristol IJ, Ahamad A, Garden AS, Morrison WH, Hanna EY, Papadimitrakopoulou VA, Rosenthal DI, Ang KK (2007) Postoperative radiotherapy for maxillary sinus cancer: long-term outcomes and toxicities of treatment. Int J Radiat Oncol Biol Phys 68: 719–730.
Dirix P, Nuyts S, Geussens Y, Jorissen M, Vander Poorten V, Fossion E, Hermans R, Van den Bogaert W (2007) Malignancies of the nasal cavity and paranasal sinuses: long-term outcome with conventional or three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 69: 1042–1050.
Homma A, Furuta Y, Suzuki F, Oridate N, Hatakeyama H, Nagahashi T, Ushikoshi S, Asano T, Nishioka T, Shirato H, Fukuda S (2005) Rapid superselective high-dose cisplatin infusion with concomitant radiotherapy for advanced head and neck cancer. Head Neck 27: 65–71.
Homma A, Oridate N, Suzuki F, Taki S, Asano T, Yoshida D, Onimaru R, Nishioka T, Shirato H, Fukuda S (2009) Superselective high-dose cisplatin infusion with concomitant radiotherapy in patients with advanced cancer of the nasal cavity and paranasal sinuses: a single institution experience. Cancer 115: 4705–4714.
Hoppe BS, Nelson CJ, Gomez DR, Stegman LD, Wu AJ, Wolden SL, Pfister DG, Zelefsky MJ, Shah JP, Kraus DH, Lee NY (2008) Unresectable carcinoma of the paranasal sinuses: outcomes and toxicities. Int J Radiat Oncol Biol Phys 72: 763–769.
Jang NY, Wu HG, Park CI, Heo DS, Kim DW, Lee SH, Rhee CS (2010) Definitive radiotherapy with or without chemotherapy for T3-4N0 squamous cell carcinoma of the maxillary sinus and nasal cavity. Jpn J Clin Oncol 40: 542–548.
Kang JH, Cho SH, Pyeong-Kim J, Kang KM, Cho KS, Kim W, Mi-Seol Y, Lee S, Soo-Park H, Joo-Hur W, Choi YJ, Oh SY (2012) Treatment outcomes between concurrent chemoradiotherapy and combination of surgery, radiotherapy, and/or chemotherapy in stage III and IV maxillary sinus cancer: multi-institutional retrospective analysis. J Oral Maxillofac Surg 70: 1717–1723.
Kanoto M, Oda A, Hosoya T, Nemoto K, Ishida A, Nasu T, Koike S, Aoyagi M (2010) Impact of superselective transarterial infusion therapy of high-dose cisplatin on maxillary cancer with orbital invasion. AJNR Am J Neuroradiol 31: 1390–1394.
Muir CS, Nectoux J (1980) Descriptive epidemiology of malignant neoplasms of nose, nasal cavities, middle ear and accessory sinuses. Clin Otolaryngol 5: 195–211.
Rasch CR, Hauptmann M, Schornagel J, Wijers O, Buter J, Gregor T, Wiggenraad R, Paul de Boer J, Ackerstaff AH, Kroger R, Hoebers FJ, Balm AJ (2010) Intra-arterial versus intravenous chemoradiation for advanced head and neck cancer: results of a randomized phase 3 trial. Cancer 116: 2159–2165.
Robbins KT (2000) The evolving role of combined modality therapy in head and neck cancer. Arch Otolaryngol Head Neck Surg 126: 265–269.
Robbins KT, Kumar P, Wong FS, Hartsell WF, Flick P, Palmer R, Weir AB 3rd, Neill HB, Murry T, Ferguson R, Hanchett C, Vieira F, Bush A, Howell SB (2000) Targeted chemoradiation for advanced head and neck cancer: analysis of 213 patients. Head Neck 22: 687–693.
Samant S, Robbins KT, Vang M, Wan J, Robertson J (2004) Intra-arterial cisplatin and concomitant radiation therapy followed by surgery for advanced paranasal sinus cancer. Arch Otolaryngol Head Neck Surg 130: 948–955.
Shiga K, Yokoyama J, Hashimoto S, Saijo S, Tateda M, Ogawa T, Watanabe M, Kobayashi T (2007) Combined therapy after superselective arterial cisplatin infusion to treat maxillary squamous cell carcinoma. Otolaryngol Head Neck Surg 136: 1003–1009.
Waldron JN, O'Sullivan B, Gullane P, Witterick IJ, Liu FF, Payne D, Warde P, Cummings B (2000) Carcinoma of the maxillary antrum: a retrospective analysis of 110 cases. Radiother Oncol 57: 167–173.
Wong RJ, Kraus DH (2001) Cancer of the nasal cavity and paranasal sinuses. In: Shah JP (ed.) Cancer of the head and neck pp 204–224. BC Decker, Inc.: Hamilton.
Acknowledgements
This study was supported in part by a Health and Labour Sciences Research Grant for Clinical Cancer Research (H22-Gannrinshou-Ippan-017) from the Ministry of Health, Labour and Welfare of Japan, the National Cancer Center Research and Development Fund (23-A-21) of Japan, and a grant-in-aid for Scientific Research (C) (KAKENHI 24592587) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Homma, A., Sakashita, T., Yoshida, D. et al. Superselective intra-arterial cisplatin infusion and concomitant radiotherapy for maxillary sinus cancer. Br J Cancer 109, 2980–2986 (2013). https://doi.org/10.1038/bjc.2013.663
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.663
Keywords
This article is cited by
-
Salvage surgery improves the treatment outcome of patients with residual/recurrent maxillary sinus cancer after superselective intra-arterial cisplatin infusion with concomitant radiation therapy
European Archives of Oto-Rhino-Laryngology (2022)
-
Radiologic criteria of retropharyngeal lymph node metastasis in maxillary sinus cancer
Radiation Oncology (2021)
-
Imaging predictor of ophthalmic involvement in maxillary sinus cancer during super selective intra-arterial cisplatin infusion and concomitant radiotherapy (RADPLAT)
Head & Face Medicine (2021)
-
Invasion of the pterygoid plates: an indicator for regional lymph node failure in maxillary sinus cancer
Radiation Oncology (2021)
-
Radiation with concomitant superselective intra-arterial cisplatin infusion for maxillary sinus squamous cell carcinoma
Japanese Journal of Radiology (2019)