Abstract
Background:
This study examines the cost-effectiveness of sentinel lymph node biopsy, a potentially less morbid procedure, compared with inguinofemoral lymphadenectomy (IFL) among women with stage I and stage II vulval squamous cell carcinoma.
Methods:
A model-based economic evaluation was undertaken based on clinical evidence from a systematic review of published sources. A decision tree model was developed with the structure being informed by clinical input, taking the perspective of the health-care provider.
Results:
For overall survival for 2 years, IFL was found to be the most cost-effective option and dominated all other strategies, being the least costly and most effective. For morbidity-free related outcomes for 2 years, sentinel lymph node (SLN) biopsy with 99mTc and blue dye and haematoxylin & eosin (H&E) histopathology, with ultrastaging and immunohistochemistry reserved for those that test negative following H&E is likely to be the most effective approach.
Conclusion:
SLN biopsy using 99mTc and blue dye with ultrastaging may be considered the most cost-effective strategy based on the outcome of survival free of morbidity for 2 years. The findings here also indicate that using blue dye and H&E for the identification of the SLN and the identification of metastasis, respectively, are not sensitive enough to be used on their own.
Similar content being viewed by others
Main
Vulval cancer represents ∼3–5% of all gynaecological malignancies and 1% of all female cancers (Hacker, 2005). It is more often seen in older women, although risk factors such as HPV (Macnab et al, 1986) and HIV (Elit et al, 2005) mean that it is also seen in younger women. In 90% of cases, it develops as a squamous cell carcinoma with the remainder being melanoma, Bartholin’s gland tumours, adenocarcinoma and basal cell carcinomas.
Current treatment for early squamous cell vulval cancer consists of radical excision of the tumour with inguinofemoral lymphadenectomy (IFL) (van der Zee et al, 2008). This treatment is effective in terms of averting groin recurrence; however, it would ideally only be used in women with nodal metastasis. Given that only 25–35% (de Hullu et al, 2000; Hampl et al, 2008) of women with presumed early-stage vulval cancer have metastasis this means that for 65–75% of women IFL will have been of no benefit, but patients will still be at increased risk from the significant morbidity resulting from the procedure (de Hullu et al, 2002). In the short-term patients may suffer wound breakdown or infection, while in the long-term lower limb lymphedema and erysipelas (type of skin infection) can occur beyond 1 year (van der Zee et al, 2008). In spite of the morbidity of IFL, it has traditionally been preferred, as unrecognised disease in the inguinofemoral lymph nodes is associated with a very high risk of mortality.
An accurate test to identify metastasis in the inguinofemoral lymph nodes with a high degree of accuracy would mean that only women with confirmed nodal disease would receive IFL, thus sparing many women from the unnecessary morbidity associated with the procedure.
It has been shown that the various imaging modalities are not sufficiently sensitive strategies to identify women with groin metastases (Selman et al, 2005), and therefore pre-operative imaging of the groin is not a good strategy to identify women who should undergo IFL. Instead, sentinel lymph node (SLN) biopsy is used to identify and surgically excise the first draining lymph node from the primary cancer. The lymph node is then examined through histopathogical techniques to detect for the presence of metastasis. Only women that test positive for a metastasis would then go on to receive an IFL. Sentinel lymph node biopsy may consist of injection of one or both of blue dye and 99mTc (technetium-99m-labelled nanocolloid). A key advantage of these biopsy procedures is that they are associated with a much lower morbidity rate than IFL (van der Zee et al, 2008). However, it is acknowledged there is a risk that a false-negative SLN biopsy could result in a woman developing a groin recurrence with the associated higher risk of mortality (van der Zee et al, 2008).
In this study, we report the results of a model-based economic evaluation based on evidence from a systematic review of the literature that we carried out as part of a wider project to identify the most appropriate testing strategies for vulval cancer. The relative cost-effectiveness of undertaking a range of SLN biopsy options among women with presumed stage I or stage II vulval cancer compared with implementing ILF for all patients is examined.
Materials and Methods
A systematic review assessing the effectiveness of SLN biopsy in the diagnosis and treatment of early-stage vulval cancer has already been conducted (Meads et al, 2013). This model-based economic evaluation relied exclusively on secondary data from the systematic review and takes the form of a cost-effectiveness analysis, carried out from a health-care provider perspective (in this case the UK NHS) in a secondary care (hospital) setting.
Model structure
A model was developed via consultation within the research team drawing on key clinical (SS, ANR and PB are all UK accredited gynaecological oncologists and regularly practice these procedures) and modelling expertise, using a decision tree in TreeAge Pro 2001 software (TreeAge Software Inc., Williamstown, MA, USA). It was felt that this approach would be most appropriate for the evaluation rather than use a Markov model due to the short-time horizon and there being no examples of the same event happening to the same patient (such as a single patient experiencing multiple groin recurrences over the 2-year time horizon) many times in the model structure. This choice of model structure is in line with published guidance, for example, Barton et al (2004); Brennan et al (2006).
Women enter the model having been identified, via prior histopathology of the primary lesion, as having presumed T1 (not T1a) or T2 FIGO stage unifocal vulval cancer. Only women with squamous cell carcinomas were considered; all other histological types were excluded due to their rarity and lack of adequate data for accurate modelling.
Seven different pathways are compared that describe alternative approaches to the SLN biopsy and the treatment of vulval cancer (referred to using square brackets in the text). The first pathway is the comparison arm (IFL without SLN biopsy), and is used to show how this more morbid treatment compares with different SLN biopsy options. In the case of pathways 2–7, SLN biopsy is performed using either blue dye, 99mTc, or both, in order to identify the SLN. This is followed by histopathology, which is a combination of haematoxylin and eosin (H&E) staining and ultrastaging in order to test for the presence of metastasis, where ultrastaging can be considered to be representative of more sensitive techniques such as immunohistochemistry and additional sections. The impact of administering H&E as the routine histopathological examination alone is also examined. For women with metastasis detected by SLN biopsy an IFL is subsequently performed with radiotherapy also given where necessary (which may be necessary when more than one intranodal metastasis and/or extracapsular spread is detected (van der Zee et al, 2008)). Following an IFL, women are clinically monitored every 3 months for 2 years for evidence of recurrence. If women only receive SLN biopsy, then under these circumstances they are clinically monitored every 2 months for 2 years, which is the protocol for the UK. The seven patient treatment pathways are defined as shown in Table 1.
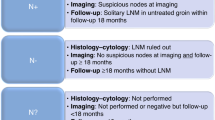
These treatment pathways are summarised in Figure 1 and the decision tree is shown in Figure 2. Further more detailed decision trees are given in the Appendices.
Clinical assumptions and parameterisation
The parameterisation of the model used in this economic evaluation was undertaken using the findings of a systematic review (Meads et al, 2013). In all cases where the results from multiple studies could be pooled to provide single-parameter values, these were always utilised. However, in cases where this was not possible, the results from larger more recent studies that were identified in the systematic review were preferred. The detection rates for the sentinel lymph node for the different types of SLN biopsy considered in this study are shown in Table 2. The application of the remaining parameters in the model are described in the appendices, while the assumptions that are required in order to develop a workable model structure and enable the analysis to be carried out are described in Table 3. These are broadly categorised as assumptions related to the general pathway, recurrence and further modelling.
Cost and resource data
All costs in the model are in UK pounds sterling £ (2010 value). Three sources of data were used to parameterise the cost component of the economic evaluation. NHS Reference Costs 09/10, information provided by the Histopathology Department at Birmingham City Hospital and data collected as part of the United Kingdom Gynaecological Oncology Surgical Outcomes and Complications audit (UKGOSOC), which is a prospective web-based audit examining outcomes of surgery in gynaecological oncology particularly focused on complications. In all cases, patients only require a maximum of one unit of each cost depending on their treatment pathway, with the itemised costs shown in Table 4.
Costs are given for blue dye and 99mTc when administered separately, however, no cost was available for the two procedures combined, and therefore it is assumed that the cost for both blue dye and 99mTc is 10% greater than 99mTc alone (the more expensive of the two). The impact of this assumption on model results is examined through sensitivity analysis.
Outcomes
This economic evaluation focuses on how the different treatment scenarios impact on the mortality and morbidity of the patients and the costs of the different treatments. Therefore, the economic analysis is based on the following outcomes:
-
1
Case of death avoided for 2 years
-
2
Case of survival free of morbidity for 2 years
-
3
Case of survival free of long-term morbidity for 2 years.
The definitions of short-term and long-term morbidity in this study are the same as those proposed by van der Zee et al (2008) for complications, in which short-term morbidity is defined as the occurrence of wound breakdown or wound infection (requiring antibiotics); and long-term morbidity is defined as lymphedema present over two consecutive visits >1 year after primary therapy or recurrent erysipelas (>1 episode of erysipelas requiring antibiotics).
For each of these outcomes, IFL is the reference scenario. There are no studies that have shown a difference in the QoL estimates for women that receive the different options considered in this analysis. Therefore, the option of using the QALY as an outcome measure was not available in this study.
The results are presented using the incremental cost-effectiveness ratio (ICER), which is defined as the difference in costs between two options divided by the difference in their effects (which in this case are the outcome measures described above) (Gray et al, 2011).
Analysis
The model estimates the mean costs associated with each of the treatment strategies and assumes that all women entering the model are aged 65 years, which is informed by the findings of the systematic review. The time horizon of the model is 2 years, which was chosen as any groin recurrences that might appear as a result of a false-negative SLN biopsy would be expected to be detected within this time frame (van der Zee et al, 2008). Owing to this short-time horizon with the majority of costs and events occurring in the first year, no discounting was applied.
Sensitivity analysis
Probabilistic and one-way sensitivity analyses were carried out in order to examine the robustness of the model results to uncertainties in the model parameters and the assumptions made. The one-way sensitivity analysis undertaken is described in Table 5:
Results
Outcomes
For overall survival for 2 years, (IFL) was the most effective strategy. For all types of survival free of morbidity the (99mTc+blue dye+ultrastaging) strategy was found to be the most effective.
Costs
The (IFL) strategy was the cheapest, costing £9367 per women treated for presumed stage I or stage II vulval cancer. The most expensive was found to be the (99mTc+blue dye+H&E) strategy costing £10 648 per patient (Table 6), which is due to the extra costs incurred as a result of the additional false-negative patients associated with this strategy having a groin node recurrence in the future, and receiving subsequent additional treatment and care.
Incremental analysis
In the case of the overall survival outcome for 2 years, the (IFL) strategy dominates all other strategies as it is both cheaper and averts the greatest mortality.
Results—survival free of morbidity for 2 years
For the outcome of survival free of morbidity for 2 years only the strategies of (blue dye+ultrastaging), (99mTc+ultrastaging) and (99mTc+blue dye+ultrastaging) remain un-dominated by any of the alternative treatment strategies (Table 6).
In terms of survival free of morbidity for 2 years, the most effective strategy is the (99mTc+blue dye+ultrastaging) strategy, but this comes at a greater cost, generating an ICER of £41 200 compared with (99mTc+Ultrastaging) (costs £400 more than (99mTc+Ultrastaging) with an extra 0.0097 of effectiveness), meaning that the strategy requires an investment of £41 200 to generate one additional case of survival free of morbidity compared with the strategy of (99mTc+ultrastaging). The strategy of (99mTc+ultrastaging) is both slightly less effective in terms of overall survival free of morbidity and slightly less costly than (99mTc+blue dye+ultrastaging). The ICER for (99mTc+ultrastaging) is ∼£4900 compared with (blue dye+ultrastaging). The ICER for (blue dye+ultrastaging) is ∼£2400 compared with (IFL), that is, a financial outlay of £2400 is necessary to generate one additional case of survival free of morbidity for 2 years compared with the (IFL).
Results—survival free of long-term morbidity for 2 years
With respect to survival free of long-term morbidity for 2 years, as with survival free of morbidity the strategies of (blue dye+ultrastaging), (99mTc+ultrastaging) and (99mTc+blue dye+ultrastaging) remained un-dominated by any of the alternative treatment strategies (Table 6).
The most effective strategy is the (99mTc+blue dye+ultrastaging) strategy, but this comes at a greater cost, generating an ICER of £74 300, that is, the strategy requires an investment of £74 300 to generate one additional case of survival free of long-term morbidity compared with the strategy of (99mTc+ultrastaging). The strategy of (99mTc+ultrastaging) is both slightly less effective in terms of overall survival free of long-term morbidity and slightly less costly than (99mTc+blue dye+ultrastaging). The ICER for (99mTc+ultrastaging) is ∼£8.900, that is, an additional financial outlay of £8900 is necessary to generate one case of survival free of long-term morbidity compared with the strategy of (blue dye+ultrastaging).
Sensitivity analysis
The results of the sensitivity analysis are described in the Appendices. With respect to the one-way sensitivity analysis, only the cost of 99mTc and blue dye implemented during the same procedure has any impact on the conclusions drawn from the model. At baseline, it was assumed that this procedure would cost 10% more than the cost of 99mTc alone. However, if this was varied from being equal to the cost of 99mTc alone to costing 50% more than 99mTc alone, then this would lead the ICER values for (99mTc+blue dye+ultrastaging) compared with (99mTc+ultrastaging) to range from £4700–£195 700 and £8400–£352 600 for a case of survival free of morbidity and survival free of long-term morbidity for 2 years, respectively.
Figure 3 shows the cost-effectiveness acceptability frontier from the probabilistic sensitivity analysis for the outcome of survival free of morbidity for 2 years. It can be seen that as the willingness to pay (WTP) crosses the ICER between two non-dominated strategies, the choice of optimal strategy changes, with a discontinuity in the curve being seen. Up to a WTP of £3500 the (IFL) strategy is the most cost-effective, and then from £3500 to ∼£42 000 the (99mTc+ultrastaging) strategy is the most cost-effective, finally for a WTP greater than ∼£42 000 the (99mTc+blue dye+ultrastaging) strategy becomes the most cost-effective.
Discussion
The results of the base–case analyses using the outcome of cost per death averted for 2 years have shown that for women with presumed stage I and stage II vulval cancer the treatment strategy of (IFL) is both less costly and more effective than any of the other strategies that utilise SLN biopsy. This result is not surprising given that this procedure seeks to reduce the potential for future recurrences at the expense of increased patient morbidity.
When considering the outcome measures of survival free of morbidity and survival free of long-term morbidity for 2 years the (99mTc+ultrastaging) strategy, where ultrastaging is administered in the case of a negative H&E test was the most cost-effective strategy. It is also likely that the (99mTc+ultrastaging+blue dye) strategy is cost-effective when compared with that of (99mTc+ultrastaging). However, there is some debate about this as it is difficult to judge the acceptability thresholds of the outcome measures used in this study (although some attempt is made below). This is in contrast to the QALY where there are clearer thresholds that can help to inform the acceptability of an intervention. It can therefore be concluded that the SLN biopsy that includes both 99mTc and ultrastaging is cost-effective in terms of the morbidity-free outcomes for 2 years compared with IFL, although there is some uncertainty about exactly what is the most cost-effective SLN biopsy option.
It is noted that the strategies that included blue dye only as the approach to the SLN biopsy, and H&E only for the histopathology were never found to be cost-effective and were always dominated by other strategies (other strategies being less costly and more effective). This finding emphasises that using blue dye and H&E for the identification of the SLN and the identification of metastasis, respectively, are not sensitive enough to be used on their own.
Further one-way deterministic sensitivity analysis found that the cost of administering 99mTc and blue dye together has the potential to have a significant impact on the results obtained from this economic evaluation. As this is a combined technique in which two types of SLN biopsy are implemented in the same procedure, it is very difficult to obtain a well-informed cost for this approach. The results here demonstrate the importance of this parameter on the model results, but also reinforce the view that at the very least (99mTc+ultrastaging) is certainly a cost-effective approach to SLN biopsy.
This economic evaluation has had the advantage of being able to utilise the best available data in the model established in a systematic review of the evidence (Meads et al, 2013), particularly the sensitivity and specificity of the procedures used to identify the SLN and any metastasis. All assumptions used in the model were agreed by a panel of experts a priori, with key assumptions being examined through the use of sensitivity analysis. Owing to the scarcity of vulval cancer, many of the data points used in this model were based on quite small samples. However, the resultant uncertainly in these parameter values was examined through the use of probabilistic sensitivity analysis.
The major limitation of this study is the absence of preference-based QoL estimates that differentiate between the impact of SLN biopsy and IFL on morbidity, making a cost-utility analysis using the QALY as the outcome measure impossible. This is unfortunate as there are thresholds for the acceptance of medical interventions using the QALY in the UK (Devlin and Parkin, 2004), which are not available for the outcome measures used in this study.
In order to provide some guidance as to the acceptability of the strategies considered in this research, an attempt is made to link the standard QALY thresholds to the morbidity-related outcomes used in this study. It can be said that a patient with 2 years survival free of morbidity will accumulate 2 QALYs within the time horizon of the model. Strictly this should be reduced to allow for discounting in the second year, but the difference will be small. A patient who either does not survive 2 years or who survives with appreciable morbidity may still accumulate some QALYs within the 2 years. Therefore, the value of an additional positive outcome using this measure is somewhat less than 2 QALYs. Using the upper NICE threshold of £30 000/QALY (Devlin and Parkin, 2004), the WTP for an additional positive outcome would be somewhat less than £60 000, although this is subject to the limitation that the 2 years time horizon means that no value is being attached to any survival beyond 2 years.
Instead of the QALY, three outcome measures have been considered in this study: overall mortality, survival free of morbidity and survival free of long-term morbidity, all considered over a maximum of 2 years. The inevitable difficulty with this selection is that it is very difficult to know which primary outcome measure is the most clinically relevant. Intuitively overall survival would seem to be best choice, however, in this setting this outcome provides little insight. IFL, while the cheapest strategy considered in this analysis, is a highly morbid procedure that is most effective at reducing the probability of a groin recurrence in the future and hence patient mortality. The option of SLN biopsy has been introduced into practice with the aim of reducing patient morbidity, but at the expense of the increased possibility of women having a false-negative diagnosis, with a resultant potential increase in mortality. Therefore, it was inevitable that in this study IFL has been shown to be the most effective procedure in terms of overall survival. Perhaps the most appropriate outcome measure in this study is survival free of morbidity, as this also incorporates all types of morbidity and the impact of overall survival into the outcome. Survival free of long-term morbidity has also been considered because oedema, which is a long-term complication, has been found to have a more significant impact on women treated with IFL compared with those receiving SLN biopsy (Oonk et al, 2009).
This analysis has highlighted the importance of obtaining overall QoL values that describe the impact of SLN biopsy and IFL and their related complications over time. A previous study attempted to identify these values but did not find a difference in overall QoL estimates between 62 women receiving either SLN biopsy or IFL despite the observed increased morbidity among women that underwent the IFL (Oonk et al, 2009). This may be because the study was too small to detect a difference or because of the type of QoL questionnaires administered, although this result could also be explained by the extra peace of mind that the IFL provides due to the increased possibility of a false-negative result with SLN biopsy. Intuitively there would need to be a difference in QoL between these two groups, as if this were not the case, IFL with its increased effectiveness at reducing the risk of a groin recurrence and therefore patient mortality, but with its much higher risk of morbidity, would always be preferred. Future work should be undertaken to examine QoL in these treatment groups using an alternative questionnaire and larger sample size.
Change history
12 November 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Barton P, Bryan S, Robinson S (2004) Modelling in the economic evaluation of health care: selecting the appropriate approach. J Health Serv Res Policy 9 (2): 110–118.
Brennan A, Chick SE, Davies R (2006) A taxonomy of model structures for economic evaluation of health technologies. Health Econ 15 (12): 1295–1310.
Crosbie EJ, Winter-Roach B, Sengupta P, Sikand KA, Carrington B, Murby B, Slade RJ (2010) The accuracy of the sentinel node procedure after excision biopsy in squamous cell carcinoma of the vulva. Surg Oncol 19 (4): e150–e154.
de Hullu JA, Hollema H, Lolkema S, Boezen M, Boonstra H, Burger MP, Aalders JG, Mourits MJ, van der Zee AG (2002) Vulvar carcinoma. The price of less radical surgery. Cancer 95 (11): 2331–2338.
de Hullu JA, Hollema H, Piers DA, Verheijen RH, van Diest PJ, Mourits MJ, Aalders JG, van der Zee AG (2000) Sentinel lymph node procedure is highly accurate in squamous cell carcinoma of the vulva. J Clin Oncol 18 (15): 2811–2816.
Devlin N, Parkin D (2004) Does NICE have a cost-effectiveness threshold and what other factors influence its decisions? A binary choice analysis. Health Econ 13 (5): 437–452.
Elit L, Voruganti S, Simunovic M (2005) Invasive vulvar cancer in a woman with human immunodeficiency virus: case report and review of the literature. Gynecol Oncol 98 (1): 151–154.
Fonseca-Moutinho JA (2005) Recurrent vulvar cancer. Clin Obstet Gynecol 48 (4): 879–883.
Gray AM, Clarke PM, Wolstenholme JL, Wordsworth S (2011) Applied Methods of Cost-effectiveness Analysis 1st edn. Oxford University Press: Oxford.
Hacker NF (2005) ‘Vulvar cancer,’ In Practical Gynaecologic Oncology Berek JS, Hacker NF, (eds) Williams & Wilkins: Philadelphia, PA, USA, pp 585–602.
Hampl M, Hantschmann P, Michels W, Hillemanns P (2008) Validation of the accuracy of the sentinel lymph node procedure in patients with vulvar cancer: results of a multicenter study in Germany. Gynecol Oncol 111 (2): 282–288.
Macnab JC, Walkinshaw SA, Cordiner JW, Clements JB (1986) Human papillomavirus in clinically and histologically normal tissue of patients with genital cancer. N Engl J Med 315 (17): 1052–1058.
Meads C, Sutton AJ, Makysiak S, Kowalska M, Zapalska A, Rogozinska E, Baldwin P, Rosenthal A, Ganesan R, Borowiack E, Barton P, Roberts T, Sundar S, Khan K (2013) Sentinel lymph node (SLN) status in vulval cancer: Systematic quantitative reviews and decision analytic model-based economic evaluation. HTA Available at http://www.hta.ac.uk/2338 (Accessed 18 September 2013).
Moore RG, Robison K, Brown AK, Disilvestro P, Steinhoff M, Noto R, Brard L, Granai CO (2008) Isolated sentinel lymph node dissection with conservative management in patients with squamous cell carcinoma of the vulva: a prospective trial. Gynecol Oncol 109 (1): 65–70.
Oonk MH, van Hemel BM, Hollema H, de Hullu JA, Ansink AC, Vergote I, Verheijen RH, Maggioni A, Gaarenstroom KN, Baldwin PJ, van Dorst EB, Van der Velden J, Hermans RH, van der Putten HW, Drouin P, Runnebaum IB, Sluiter WJ, van der Zee AG (2010a) Size of sentinel-node metastasis and chances of non-sentinel-node involvement and survival in early stage vulvar cancer: results from GROINSS-V, a multicentre observational study. Lancet Oncol 11 (7): 646–652.
Oonk MH, van Hemel BM, Hollema H, de Hullu JA, Ansink AC, Vergote I, Verheijen RH, Maggioni A, Gaarenstroom KN, Baldwin PJ, van Dorst EB, Van der Velden J, Hermans RH, van der Putten HW, Drouin P, Runnebaum IB, Sluiter WJ, van der Zee AG (2010b) Size of sentinel-node metastasis and chances of non-sentinel-node involvement and survival in early stage vulvar cancer: results from GROINSS-V, a multicentre observational study. Lancet Oncol 11 (7): 646–652.
Oonk MH, van Os MA, de Bock GH, de Hullu JA, Ansink AC, van der Zee AG (2009) A comparison of quality of life between vulvar cancer patients after sentinel lymph node procedure only and inguinofemoral lymphadenectomy. Gynecol Oncol 113 (3): 301–305.
Selman TJ (2009) Non-invasive and minimally invasive diagnosis and therapy of lymphadenopathy in gynaecological cancers—Systematic reviews of the evidence. PhD University of Birmingham, Birmingham, UK.
Selman T.J., Luesley D.M., Acheson N., Khan K.S., Mann C.H. (2005) A systematic review of the accuracy of diagnostic tests for inguinal lymph node status in vulvar cancer. Gynecol Oncol 99 (1): 206–214.
van der Zee AG, Oonk MH, de Hullu JA, Ansink AC, Vergote I, Verheijen RH, Maggioni A, Gaarenstroom KN, Baldwin PJ, van Dorst EB, Van der Velden J, Hermans RH, van der Putten H, Drouin P, Schneider A, Sluiter WJ (2008) Sentinel node dissection is safe in the treatment of early-stage vulvar cancer. J Clin Oncol 26 (6): 884–889.
Acknowledgements
This work was supported by the Health Technology Assessment, National Institute of Health Research, United Kingdom—project number 09/112/03.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Appendices
Appendix A
Detailed decision trees showing patient pathways.
Note: Patients who have a local recurrence are given a primary excision. Patients who have a groin recurrence following IFL+RT are given chemotherapy. Patients who have a groin recurrence following an IFL only are given RT.
Note: Patients who have an IFL with or without RT may still go on to have either a local or groin recurrence. In the case of a local recurrence, all patients are given a primary excision. Patients who have a groin recurrence having previously received an IFL+RT are given chemotherapy, while for those who have only previously received an IFL are given RT.
Note: Patients who have a false-negative biopsy test result, subsequently go on to have a groin recurrence. In this case, all the patients receive both an IFL+RT.
Note: Patients who have a true-negative biopsy test do not subsequently go on to have a groin recurrence. However, a local recurrence is still possible, and under these circumstances the patients are given a primary excision.
Appendix B
Appendix C
Calculation of histopathology test accuracy parameters
The focus of this section is in linking data describing the prevalence of metastasis in the literature with the final outcomes for each of the histopathology testing strategies among patients that already have an identified SLN, namely, TP, FP, TN and FN.
Following the identification of the SLN(s) using a SLN biopsy, their histopathological assessment considered in this economic evaluation is the same as that described by van der Zee et al (2008). H&E staining of the lymph node is used, and then if no metastasis is seen, ultrastaging with immunohistochemistry is then undertaken to confirm absence/presence of metastases.
The following calculations describe the possible outcomes for patients that have a detected SLN that is then subject to histopathology. As previously described, two approaches to histopathology are considered, these being H&E + ultrastaging and H&E alone. These are each considered in turn:
H&E + ultrastaging
Among patients with an identified SLN that was subject to H&E+ultrastaging, van der Zee et al (2008) describe that 6 out of 259 patients with unifocal vulval cancer and a negative SLN following H&E and ultrastaging were subsequently diagnosed with a groin recurrence (giving a negative predictive value of 253/259 for H&E and ultrastaging). And therefore by definition:
Number of false negatives (FN)=6
Number of true negatives (TN)=253
A systematic review (Meads et al, 2013) failed to find any evidence of patients testing false positive for metastasis (26 studies were considered), and so it is assumed here that FP=0.
Taking the above values for FN and TN, and the assumption that FP=0, this means that the assumed prevalence of metastasis in this study cannot fall below 2.3% (6/259).
The number of disease (metastasis) negative (DN) can be calculated from the sum of the patients that test true negative (TN) and false positive (FP) for metastasis (TN+FP):
DN=TN+FP
As described in the table of parameters shown in Appendix B, the proportion of patients with metastasis (p) is taken to be 0.335 (135/403). From this, the number of disease (metastasis) positive (DP) can be calculated:
DP=DN × p/(1−p)
Taking the previously calculated values for FN and DP, the number of true positives can now be calculated:
Number of true positives (TP)=DP−FN
Now that we have values for FN, TN, FP and TP, which are based on values obtained from the literature, which include the assumed prevalence of metastasis, it is straightforward to calculate what proportion of patients will test for each of these possibilities for H&E +ultrastaging, with the baseline parameters shown in the Table below.
For H&E alone
As part of the study by Oonk, et al (2010a, 2010b) 80 out of 135 patients that were found to have metastasis were initially found positive by H&E with the remainder being found positive through ultrastaging. This gives the sensitivity of H&E (SensH&E) to be 59% (80/135). However, this alone cannot be used to directly calculate the TP and FN values for H&E, as the value for DP (used below) incorporates information on the negative predictive value of Ultrstaging+H&E (253/259). This must also be considered here, as patients that have a groin recurrence after ultrastaging+H&E will certainly do the same for the less-sensitive option of H&E on its own.
Therefore, taking the number of disease (metastasis) positive (DP) described above for H&E +ultrastaging, the number of true positives and false negatives detected by H&E can be given as follows:
Number of true positives (TPH&E)=SensH&E*DP
Number of false negatives (FNH&E)=DP−TPH&E
Taking the number of true negatives detected by H&E (TNH&E) to be the same as for H&E +ultrastaging and again assuming that FPH&E=0.
The values for FNH&E, TNH&E, FPH&E, and TPH&E allow the proportion of patients that test for each of these possibilities for H&E alone to be calculated, with the values used at baseline shown in Table 4.
In all cases, the values taken from the literature, for example, prevalence of metastasis, are varied as part of the probabilistic sensitivity analysis in order to show their impact on the model results.
Appendix D
Probabilistic sensitivity analysis
The results described by the cost-effectiveness point estimates do not consider any uncertainty in relation to the model input parameters. Probabilistic sensitivity analysis (PSA) was therefore undertaken to assess the impact of the uncertainty in the model parameters on the results and conclusions obtained from the model. The costs in the model are all unit costs for specific procedures and are treated as fixed, however the number of bed days were varied. The probabilities in the tree, these being the proportions of patients that follow each branch were also varied.
The standard distribution used in this analysis for the proportions is the beta distribution. The beta distribution is described by two parameters a and b. A beta (α, β) distribution is able to precisely represent the uncertainty in a proportion when the only available information is α positive cases and β, negative cases. In all cases in this study exact numbers were available, and so these were used to inform the parameters of each Beta distribution directly. The bed days were described by a gamma distribution. The method of moments approach was used to estimate the parameters of the gamma distribution, where:
α=(mean^2)/(s.e.^2)
β=(s.e.^2)/(mean)
* It is assumed that the negative predictive value of HE + ultrastaging is independent of the proportion of patients with metastasis.
Appendix E
Sensitivity analysis—results
Probabilistic sensitivity analysisSurvival at 2 years
For all values of a WTP from £0 to £100 000 for the overall survival outcome measure, the (IFL) strategy was found to be the most cost-effective, and so the cost-effectiveness acceptability frontier for overall survival for 2 years is not shown.
Survival free of morbidity for 2 years
See manuscript for cost-effectiveness acceptability frontier for the outcome measure of survival free of morbidity for 2 years.
Survival free of long-term morbidity for 2 Years
One-way sensitivity analysis
The results of the one-way sensitivity analysis are shown in the table below:
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Sutton, A., Barton, P., Sundar, S. et al. Cost-effectiveness of sentinel lymph node biopsy vs inguinofemoral lymphadenectomy in women with vulval cancer. Br J Cancer 109, 2533–2547 (2013). https://doi.org/10.1038/bjc.2013.631
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.631
Keywords
This article is cited by
-
Lymphoscintigraphy and sentinel lymph node biopsy in vulvar carcinoma: update from a European expert panel
European Journal of Nuclear Medicine and Molecular Imaging (2020)
-
Japan Society of Gynecologic Oncology guidelines 2015 for the treatment of vulvar cancer and vaginal cancer
International Journal of Clinical Oncology (2018)