Abstract
Background:
Interferon (IFN)-based therapies could eradicate hepatitis C (HCV) and reduce the risk of hepatocellular carcinoma (HCC). However, HCC could still happen after sustained virological response (SVR). We aimed to develop a simple scoring system to predict the risk of HCC development among HCV patients after antiviral therapies.
Methods:
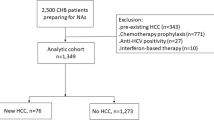
From 1999 to 2009, 1879 patients with biopsy-proven HCV infection treated with IFN-based therapies were analyzed.
Results:
Multivariable analysis showed old age (adjusted HR (aHR)=1.73, 95% CI=1.13–2.65 for aged 60–69 and aHR=2.20, 95% CI=1.43–3.37 for aged ⩾70), Male gender (aHR=1.74, 95% CI=1.26–2.41), platelet count <150 × 109/l (HR=1.91, 95% CI=1.27–2.86), α-fetoprotein ⩾20 ng ml−1 (HR=2.23, 95% CI=1.58–3.14), high fibrotic stage (HR=3.32, 95% CI=2.10–5.22), HCV genotype 1b (HR=1.53, 95% CI=1.10–2.14), and non SVR (HR=2.40, 95% CI=1.70–3.38) were independent risk factors for HCC. Regression coefficients were used to build up a risk score and the accuracy was evaluated by using the area under the receiver operating characteristic curve (AUC). Three groups as low-, intermediate-, and high-risk are classified based on the risk scores. One hundred sixty patients (12.78%) in the derivation and 82 patients (13.08%) in the validation cohort developed HCC with AUC of 79.4%, sensitivity of 84.38%, and specificity of 60.66%. In the validation cohort, the 5-year HCC incidence was 1.81%, 12.92%, and 29.95% in low-, intermediate-, and high-risk groups, with hazard ratios 4.49 in intermediate- and 16.14 in high-risk group respectively. The risk reduction of HCC is greatest in patients with SVR, with a 5-year and 10-year risk reduction of 28.91% and 27.99% respectively.
Conclusion:
The risk scoring system is accurate in predicting HCC development for HCV patients after antiviral therapies.
Similar content being viewed by others
Main
HCV infection is one of the causative risk factors of chronic liver disease and greatly contributes to the etiology of hepatocellular carcinoma (HCC) (Lavanchy, 2009). HCC incidence in patients with HCV-related cirrhosis has increased recently in several parts of the world (Rahman El-Zayadi et al, 2001; El-Serag 2004; Fattovich et al, 2004). Prevention of complications associated with chronic HCV infection is one of the most important issues in public health worldwide. Interferon/pegylated-interferon in combination with ribavirin (RBV) therapy is widely used in the treatment of chronic HCV infection (McHutchison et al, 1998; Manns et al, 2001; Fried et al, 2002; Hadziyannis et al, 2004). Curative therapy may prevent these complications (Papatheodoridis et al, 2001; Craxi and Camma, 2005). Introduction of antiviral therapy among high-risk patients could reduce the incidence of hepatic decompensation and possibly the development of HCC (Veldt et al, 2007). The IFN-based therapy can reduce HCC development and prolong survival in patients especially in those who have achieved a sustained virological response (SVR) (Papatheodoridis et al, 2001; Craxi and Camma, 2005). Therefore, the accurate risk stratification for HCC development for HCV patients is important. Risk factors for disease progression in chronic hepatitis C could be host, viral, or environmental factors. Host factors include older age at the time of infection, male gender, genetic susceptibility, diabetes mellitus (DM) and obesity (Abe et al, 2010; Fabris et al, 2011; Hung et al, 2011). Viral factors include HCV RNA level and genotype (Bruno et al, 2007; Lee et al, 2008; Hung et al, 2011). Increasing HCV RNA levels have been associated with a stepwise increase in HCC risk (Lee et al, 2010). HCV genotype is also a contentious risk factor for HCC, such as genotype 1b (Lee et al, 2008; Hung et al, 2011), and amino acid variations in the NS5A and E2-PePHD region (Hung et al, 2008). In addition, environmental factors, such as aflatoxin, Cannabis Sativa exposure, and alcohol use also play a role in liver carcinogenesis (Chen et al, 2007; Mallat et al, 2008).
There is consensus in guidelines about when and how to treat this disease and who should be treated (European Association for the Study of the Liver, 2011; Marc et al, 2011). Since antiviral therapy could reduce risk of HCC, there is a lack of standard guidance about the assessment of HCC risk in chronic hepatitis C after antiviral therapy. Several scoring systems have been proposed for chronic hepatitis, in which most studies were limited in HBV carrier (Yuen et al, 2009; Yang et al, 2010, 2011).
For most clinicians, a simple risk score comprising routinely measured parameters is preferred. In this study, we aimed to develop and validate a simple scoring system for HCC from a large cohort of chronic HCV patients after interferon based therapies.
Patients and methods
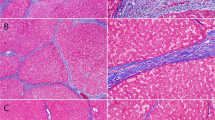
From January 1999 to October 2009, 1879 consecutive patients with biopsy-proven chronic HCV infection who have been treated with interferon (IFN) or pegylated interferon (peg-IFN) plus ribavirin therapies were enrolled. All patients had positive HCV antibody, detectable HCV RNA in serum and elevated alanine aminotransferase (ALT) levels for more than 6 months before enrollment. Patients with decompensated liver disease, and hepatitis other than hepatitis C (hepatitis B, autoimmune hepatitis and alcohol abuse) were excluded. Patients with HCC developed before treatment or within 6 months after the end of therapy were also excluded. All patients underwent liver biopsies within 6 months before the start of therapy. Specimens of liver biopsy were evaluated according to a modified Knodell histology index; fibrosis score 4 was defined as cirrhosis (Desmet et al, 1994). None of the patients had history of hepatic encephalopathy, esophageal variceal hemorrhage or ascites before therapy. This study has been approved by the institutional review board of Chang Gung Memorial hospital.
Treatments and follow-up
For HCV therapy, the regimens consisted of peg-IFN alfa-2a (Pegasys, F Hoffmann-La Roche, Basel, Switzerland; 180 μg/week subcutaneously); peg-IFN alfa-2b (Peg-Intron, Schering-Plough, Kenilworth, NJ; 1–1.5 μg/kg/week subcutaneously) or IFN alfa-2b (Intron-A, Schering-Plough, Kenilworth, NJ; 3 or 5 million units subcutaneously thrice weekly). In addition, oral ribavirin (Rebetol, Schering Plough, Kenilworth, NJ) was prescribed daily. The daily dose of ribavirin was 1000 mg for patients who weighed less than 75 kg and 1200 mg for patients more than 75 kg. Ribavirin dosing was modified according to the drop of hemoglobin. The duration of therapy was 24 weeks for genotype 2, and 48 weeks for genotype 1 patients. Serum HCV RNA was assessed prior to, at the end, and 24 weeks after therapy. SVR was defined as absence of serum HCV RNA at week 24 after treatment. Detectable HCV RNA at week 24 after treatment was defined as non-SVR. After completion of antiviral therapy, all patients were regularly followed every 3–6 months. The end of follow up was either the time of HCC development or the date of last follow-up. The observation was closed on December 31, 2012. Patients who died of non-HCC etiologies or who lost regular follow up was treated as censored data. The follow-up studies included clinical assessment, biochemical tests and HCC screening using serum α-fetoprotein and ultrasonography (US). A new space-occupying lesion detected or suspected at the time of US would be further examined by computed tomography and/or MRI, selective hepatic angiography or fine needle aspiration. Diagnosis of HCC adopted the guidelines of the American Association for the Study of Liver Disease in 2005 (Bruix et al, 2005). Except the histological proof, HCC could be diagnosed if there is one typical HCC feature on a dynamic image and/or a-fetoprotein >200 ng/ml with tumor size larger than 2 cm in a cirrhotic liver, or two typical HCC features of dynamic images for tumor size between 1 and 2 cm in a cirrhotic liver.
Laboratory investigations
Antibody to HCV was assessed using third generation enzyme-linked immunosorbent array (Ax SYM HCV 3.0, Abbott Laboratories, Chicago, IL). Qualitative detection of HCV RNA was performed by a standardized qualitative reverse transcription-polymerase chain reaction (RT-PCR) assay (Amplicor, Roche Diagnostics, Branchburg, NJ), using biotinylated primers for the 50 noncoding region. The lowest detection limit of this assay was 100 copies/ml (50 IU ml−1). Serum HCV RNA levels were determined by a branched-DNA (b-DNA) signal amplification assay (VERSANT HCV RNA 3.0. Assay, Bayer Diagnostics, Emeryville, CA, USA). This assay was a sandwich nucleic acid hybridization procedure with a detectable limit at 3400 copies ml−1. Genotyping of HCV was performed by reverse hybridization assay (Inno-LiPATM HCV II; Innogenetics NV, Gent, Belgium) using the HCV-Amplicor products.
Statistical analysis
We randomly allocated our study patients into model derivation and validation sets in a 2 : 1 ratio. The derivation cohort was used to development the risk assessment model, and the validation cohort was used to test the final model. All analyses of data from the derivation cohort were performed before the analyses of data from validation cohort. Chi-squared test or t-test was used for comparison of categorical or continuous variables. Time to HCC diagnosis was defined from the date documented of SVR or not, to the date of HCC diagnosis. Kaplan–Meier method and the log-rank test were used to compare the cumulative risks of development of HCC in different groups of patients. Cox’s proportional hazards model was performed to determine the relationship between clinical variables and the development of HCC. A simple risk score devised by using significant variables obtained from forward multivariable analysis with P⩽0.05. The score was the weighted sum of those variables of which the weights were defined as the quotient (rounded to nearest integer) of corresponding estimated coefficients from a Cox’s regression analysis divided by the smallest regression coefficient. The discrimination capabilities was presented by receiver operating characteristic (ROC) curve in the form of a plot depicting sensitivity divided by 1 minus specificity based on the derivation cohort. We excluded the subjects who did not complete 5 years of follow-up without having the HCC and calculated the ROC curve. The accuracy was measured by the area under ROC curve (AUC). The score was then categorized into three groups, namely low-, intermediate-, and high-risk, with different cutoff values. The final model was applied to the validation cohort in predicting the risk of HCC. All statistical tests were two-sided, and P⩽0.05 was considered statistically significant.
Results
Table 1 lists the clinical and laboratory data of the derivation and validation cohorts. There were 1252 and 627 cases in deviation and validation cohorts respectively. No significant differences existed between two cohorts.
Predictors of HCC and derivation of prediction score
At the end of follow up, 160 of 1252 (12.8%) patients in the derivation cohort developed HCC. Table 2 demonstrated the association between clinical characteristics and HCC. Variables such as old age, high ALT levels, low platelet counts, high AFP levels, advanced fibrotic stage, HCV genotype 1b, diabetes mellitus (DM), and non-SVR were significantly associated with HCC development. Univariate analysis by Cox’s regression analysis revealed that the development of HCC was significantly associated with old age (hazard ratio (HR)=2.18, 95% CI=1.44–3.29 for aged 60–69 and 3.70, 95% CI=2.45–5.60 for aged ⩾70), high ALT levels (HR=3.20, 95% CI=0.75–13.64 for aged 40-79 and 4.73, 95% CI=1.17–19.12 for aged ⩾80), platelet count <150 × 109 l−1 (HR=4.79, 95% CI=3.36–6.84), AFP⩾20 ng/ml (HR=4.38, 95% CI=3.18–6.02), HCV G1b (HR=1.97, 95% CI=1.44–2.70), advanced fibrotic stage (HR=6.32, 95% CI=4.2–9.51), DM (HR=2.31, 95% CI=1.66–3.21), and non-SVR (HR=3.94, 95% CI=2.87–5.41). Further multivariable analysis revealed that old age group (adjusted HR (aHR)=1.73, 95% CI=1.13–2.65 for aged 60–69 and aHR=2.20, 95% CI=1.43–3.37 for aged ⩾70), male gender (aHR=1.74, 95% CI=1.26–2.41), platelet count <150 × 109 l−1 (HR=1.91, 95% CI=1.27–2.86), AFP⩾20 ng ml−1 (HR=2.23, 95% CI=1.58–3.14), HCV G1b (HR=1.53, 95% CI=1.10–2.14), advanced fibrotic stage (HR=3.32, 95% CI=2.10–5.22), and non-SVR (HR=2.40, 95% CI=1.70–3.38) were independent risk factors for HCC development after antiviral therapies (Table 3).
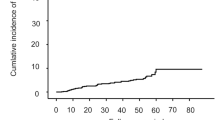
Subsequently, a simple risk score devised by using significant variables in the multivariable model according to its contribution of regression coefficients (Table 4). The score ranged from 0 to 9. To avoid bias, we excluded the subjects who did not complete the 5 years of follow-up without having the HCC and calculated the ROC curve. ROC curve was performed and the area under ROC was 79.4% (Figure 1). The optimal cut-off point was score 5. For clinical and informative application, patients were further categorized into three risk groups as low- (score⩽4), median (5⩽ score ⩽6), and high-risk group (score⩾7) with 703 (56.2%), 356 (28.4%), and 193 patients (15.4%) respectively. In the low-, intermediate-, and high-risk groups, 25 (3.56%), 61 (17.13%), and 74 patients (38.34%) developed HCC respectively during the period of follow-up (P<0.001) (Figure 2A). By applying the cutoff point of 5, 135 patients with HCC were correctly identified and 678 without HCC were correctly identified Thus, the sensitivity and specificity of this cutoff value to detect HCC was 84.38% and 60.66%. The positive and negative predictive values were 36.19% and 93.62%. The 5- and 10-year HCC incidence rates were 2.68% and 6.36% respectively in the low-risk category; 14.35% and 22.99% respectively in the intermediate-risk category (HR=5.06; 95% CI, 3.18–8.06); and 25.75% and 58.37% respectively in the high-risk category (HR=12.89; 95% CI, 8.18–20.32).
We further illustrate four subjects with different risk factors. Patient A indicated group of men gender with age between 60–70 years-old, platelet<150 × 109 l−1, AFP⩾20 ng ml−1, HCV G1b genotype. Suppose his fibrosis stage was 3–4 and failure of treatment, the 5-year and 10-year risk of HCC were 62.27% and 90.56% respectively. If he can achieve SVR, the 5-year and 10-year risk may reduce to 33.36% and 62.57%, respectively. If his fibrosis stage was 0–2, the 5-year and 10-year risks may reduce 13.95% and 25.27% when achieving SVR. For patient B with aged 60-70, male, platelet <150 × 109 l−1, AFP<20 ng ml−1, HCV G1b genotype and fibrosis stage 3-4, he changed from high risk group to intermediate risk group if the HCV treatment had response. The 5-year and 10-year risks can reduce from 35.42% to 16.65% and from 65.31% to 35.65%, respectively. If fibrosis stage was 0–2 of patient B, the 5-year and 10-year risk may reduce 7.01% and 14.89%. For patient C with aged 60–70, male, platelet ⩾150 × 109 l−1, AFP<20 ng/ml, HCV non-G1b genotype and fibrosis stage 3–4, the 5-year and 10-year risk may reduce 7.86% and 16.39% and changed from intermediate risk group to low risk group. Even in the lowest risk patient D, although risk category were all low, SVR still reduce HCC risk 6.45% in advanced fibrosis and 2.06% in mild fibrosis patients at 10 years. These results indicated that the HCC risk reduction is greater for patients with higher risk score after SVR (Supplementary Table).
Validation of results
At the end of follow-up, eighty-two of 627 patients (13.1%) in the validation cohort developed HCC. 349 patients (55.66%) had scores less than 5 and 180 patients (28.71%) had scores of 5 to 6; and 98 patients (15.63%) had scores ⩾7. The corresponding numbers of patients developing HCC were 12 (3.44%), 28 (15.56%), and 42 patients (42.86%) respectively. By applying the cutoff score of 5, 70 patients and 337 patients with and without HCC were correctly identified. Thus, the overall sensitivity and specificity of this cutoff score to detect HCC was 85.37% and 60.42%. The positive and the negative predictive value were 34.83% and 94.34%. The difference in HCC incidence among the risk categories was significant (Figure 2B). The 5- and 10-year HCC incidence were 1.81% and 6.78% respectively in the low-risk category; 12.92% and 21.06% respectively in the intermediate-risk category (HR=4.49; 95% CI, 2.28–8.82); and 29.95% and 63.79% respectively in the high-risk category (HR=16.14; 95% CI, 8.48–30.70).
Finally, we have also identified a subset of patients who belong to ‘no risk ’of HCC development. They are 6 patients with score 0, and 104 patients with score 1. After IFN based treatment, these 110 patients with score 0–1 did not have HCC development until the end of follow-up.
Discussion
In this study, we developed a simple score composed of routinely available clinical and laboratory parameters to predict the risk of HCC in chronic HCV patients after antiviral therapies. This predictive score is accurate and reproducible. Patients with a prediction score of <5, 5–6, and ⩾7 had distinctly different risk of HCC development. Notably, patients with score 0–1 are ‘no risk’ of HCC. In both the training and validation cohorts, more than half of the patients belonged to the low-risk category and had low incidence of HCC (7% at 10 years). In contrast, approximately 21% of patients had gradated risk of HCC development across the intermediate to high-risk groups. Identification of patients risk could initiate an individualized surveillance program for HCV patients after antiviral therapies.
Compared with current guidelines (Bruix et al, 2005; Omata et al, 2010), the present predictive score provides more refined and systematic stratification of HCC risk for patients after antiviral therapy. It was obvious that IFN-based therapy decreased the risk of HCC in sustained responders. However, the incidence of HCC may still gradually increase over a period of time. This suggested that the risk of developing HCC was not completely eliminated even in patients who achieved a sustained response to the IFN therapy. In the present study, we found that 93 of 1185 (7.84%) of SVR patients developed HCC during follow-up (Table 2). Based on the estimated results of multivariable Cox’s regression model, if patients can achieve SVR, the average five years risk reduction of HCC is 4.8%, and the ten years risk reduction is 10.7% when taking into account the effects of age, gender, platelet, AFP, fibrotic stage and HCV genotype. The scoring system also suggests that patients with histology of cirrhosis or with platelet level less than 150 × 109 l−1 have intermediate to high risk of developing HCC. These findings concur with previous reports that patients with cirrhosis or even liver decompensation are at substantial risk of HCC development (Ueno et al, 2001; Kubo et al, 2004; Lu et al, 2006; Amarapurkar et al, 2009). In addition, among non-cirrhotic patients, the risk of HCC development remains low unless patients have age ⩾60 years. These findings echo large epidemiologic studies that demonstrated old age to be a risk factor for HCC development (Asahina et al, 2010). Notably, the HCC risk reduction is greatest for patients with highest risk score when SVR is acheieved. For example, in the present study, in male patients with age between 60–70 years-old, platelet <150 × 109 l−1, AFP ⩾20 ng ml−1, HCV G1b genotype, and advanced fibrotic stages (who is with the highest risk scores), the 5-year and 10-year risk of HCC were reduced from 62.27% to 33.36% and 90.56% to 62.57% respectively after SVR (Supplementary Table). Furthermore, SVR also reduce the risk category in advanced fibrosis patients. The information is very useful for clinical practice.
The predictive score has potential clinical implications. In our study found that an AFP level ⩾20 ng ml−1 was a risk factor development of HCC. Previous reports also revealed that AFP and AFP-13 is an independent predictor for the HCC development (Durazo et al, 2008). AFP-L3, an isoform of AFP, is an independent predictor for the HCC development, with 10% as the cut-off (Durazo et al, 2008). Unfortunately, check up of AFP-L3 is not available in our hospital. According to previous cost-effective analysis, annual or semiannual surveillance by ultrasound scan and/or AFP is considered to be cost effective when the incidence of HCC exceeds 1% to 2% per year (Andersson et al, 2008; Nouso et al, 2008). In one study, the incremental cost-effectiveness ratio of an HCC surveillance program by abdominal ultrasonography was $56 000 when the annual HCC incidence was 1% but decreased to $29 900 when the annual incidence increased to 4% (Nouso et al, 2008). In the present study, the score can help to identify no risk or low-risk patients for whom close HCC surveillance may not be cost effective. This maybe important for patients who have undertaken antiviral therapies, as well as regions where universal screening may not be feasible.
Other groups have also evaluated the use of predictive models for HCC in patients with chronic HCV (Lee et al, 2012). In recent one study derived a risk function normogram from 3644 Taiwan patients observed for a mean of 11 years (Lee et al, 2012). A normogram comprising sex, age, ALT, liver cirrhosis, and HCV RNA/genotype had good accuracy in predicting HCC. The main strengths of the study include the large number of patients and the multicenter design. However, most of the patients initially were not treated, thus just representing patients seen in the primary care setting. Hence, the predictors in that study will be less helpful to general practitioners taking care of patients in hospital base. Our study model has several unique features. The present scoring system devised from large cohorts of treated patients observed for a long period. The large number of patients developing HCC (171 in the derivation cohort and 73 in the validation cohort) allowed accurate evaluation of different risk factors. Second, the score was validated with another sizable cohort, and was confirmed with high accuracy. Third, the seven parameters used in the score could be commonly measured in clinic, and the simple calculation of the score could facilitate implementation of routinely clinical use.
Our study still has a few limitations. First, it is a retrospective study. Second, all patients were Taiwanese residents in a single center with relative uniform of patients. Risk factors for HCC may differ in other countries and different races in which the therapeutic response to HCV therapy may be different. Therefore, the scoring system needs to be further validated before generalization to western populations. Anyway, the scoring system is applicable and reproducible in other geographic areas.
As for the time interval between surveillance tests, both the AASLD (Bruix et al, 2005) and the Asian Pacific Association of the Study of Liver (APASL) (Omata et al, 2010) recommend serum AFP level measurements, combined with US, for HCC surveillance at 6-month intervals for patients with chronic hepatitis. However, no study was conducted to determine the ideal surveillance interval for patients after antiviral therapies, especially for patients achieving SVR. Therefore, the ideal surveillance interval for treatment-experienced patients should be different, and may range from 3 to 12 months. In our study, we propose that surveillance of high-risk patients should be performed with 3–6 month interval. However, a 12 month-interval for surveillance may be enough for low-risk patients.
In conclusion, as we know, SVR of HCV could reduce the risk of HCC. For the high risk patients who did not achieve SVR before, we have to do more effort to eradicate the HCV virus in order to reduce HCC. In patients who could not achieve SVR or who are still within high risk category even after SVR, selection of an intensive HCC surveillance program is important to early detect HCC, followed by early treatment which could increase patients’ survival.
Change history
29 October 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abe H, Ochi H, Maekawa T, Hayes CN, Tsuge M, Miki D, Mitsui F, Hiraga N, Imamura M, Takahashi S, Ohishi W, Arihiro K, Kubo M, Nakamura Y, Chayama K (2010) Common variation of IL28 affects gamma-GTP levels and inflammation of the liver in chronically infected hepatitis C virus patients. J Hepatol 53: 439–443.
Amarapurkar D, Han KH, Chan HL, Ueno Y Asia-Pacific Working Party on Prevention of Hepatocellular Carcinoma (2009) Application of surveillance programs for hepatocellular carcinoma in the Asia-Pacific Region. J Gastroenterol Hepatol 24: 955–961.
Andersson KL, Salomon JA, Goldie SJ, Goldie SJ, Chung RT (2008) Cost effectiveness of alternative surveillance strategies for hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol 6: 1418–1424.
Asahina Y, Tsuchiya K, Tamaki N, Hirayama I, Tanaka T, Sato M, Yasui Y, Hosokawa T, Ueda K, Kuzuya T, Nakanishi H, Itakura J, Takahashi Y, Kurosaki M, Enomoto N, Izumi N (2010) Effect of aging on risk for hepatocellular carcinoma in chronic hepatitis C virus Infection. Hepatology 52: 518–527.
Bruix J, Sherman M American Association for the Study of Liver Diseases (2005) Management of hepatocellular carcinoma-an update. Hepatology 42: 1208–1236.
Bruno S, Crosignani A, Maisonneuve P, Rossi S, Silini E, Mondelli MU (2007) Hepatitis C virus genotype 1b as a major risk factor associated with hepatocellular carcinoma in patients with cirrhosis: A seventeen-year prospective cohort study. Hepatology 46: 1350–1356.
Chen CH, Wang MH, Wang JH, Hung CH, Hu TH, Lee SC, Tung HD, Lee CM, Changchien CS, Chen PF, Hsu MC, Lu SN (2007) Aflatoxin exposure and hepatitis C virus in advanced liver disease in a hepatitis C virus endemic area in Taiwan. Am J Trop Med Hyg 77: 747–752.
Craxi A, Camma C (2005) Prevention of hepatocellular carcinoma. Clin Liver Dis 9: 329–346.
Desmet VJ, Gerber M, Hoofnagle JH, Manns M, Scheuer PJ (1994) Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology 19: 1513–1520.
Durazo FA, Blatt LM, Corey WG, Lin JH, Han S, Saab S, Busuttil RW, Tong MJ (2008) Des-γ-carboxyprothrombin, α-fetoprotein and AFP-L3 in patients with chronic hepatitis, cirrhosis and hepatocellular carcinoma. J Gastroenterol Hepatol 23: 1541–1548.
El-Serag HB (2004) Hepatocellular carcinoma: recent trends in the United States. Gastroenterology 127: S27–S34.
European Association for the Study of the Liver (2011) EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J Hepatol 55: 245–264.
Fabris C, Falleti E, Cussigh A, Bitetto D, Fontanini E, Bignulin S, Cmet S, Fornasiere E, Fumolo E, Fangazio S, Cerutti A, Minisini R, Pirisi M, Toniutto P (2011) IL-28B rs12979860 C/T allele distribution in patients with liver cirrhosis: Role in the course of chronic viral hepatitis and the development of HCC. J Hepatol 54: 716–722.
Fattovich G, Stroffolini T, Zagni I, Donato F (2004) Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 127: S35–S50.
Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Gonçales FL Jr, Häussinger D, Diago M, Carosi G, Dhumeaux D, Craxi A, Lin A, Hoffman J, Yu J (2002) Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N. Engl J Med 347: 975–982.
Hadziyannis SJ, Sette H Jr, Morgan TR, Balan V, Diago M, Marcellin P, Ramadori G, Bodenheimer H Jr, Bernstein D, Rizzetto M, Zeuzem S, Pockros PJ, Lin A, Ackrill AM (2004) Peginterferon-alpha2a and ribavirin combination therapy in chronic hepatitis C: A randomized study of treatment duration and ribavirin dose. Ann Intern Med 140: 346–355.
Hung CH, Chen CH, Lee CM, Wu CM, Hu TH, Wang JH, Yen YH, Lu SN (2008) Association of amino acid variations in the NS5A and E2-PePHD region of hepatitis C virus 1b with hepatocellular carcinoma. J Viral Hepat 15: 58–65.
Hung CH, Lee CM, Wang JH, Hu TH, Chen CH, Lin CY, Lu SN (2011) Impact of diabetes mellitus on incidence of hepatocellular carcinoma in chronic hepatitis C patients treated with interferon-based antiviral therapy. Int J Cancer 128: 2344–2352.
Kubo S, Tanaka H, Shuto T, Takemura S, Yamamoto T, Uenishi T, Tanaka S, Ogawa M, Sakabe K, Yamazaki K, Hirohashi K (2004) Correlation between low platelet count and multicentricity of hepatocellular carcinoma in patients with chronic hepatitis C. Hepatol Res 30: 221–225.
Lavanchy D (2009) The global burden of hepatitis C. Liver Int 29: 74–81.
Lee CM, Hung CH, Lu SN, Changchien CS (2008) Hepatitis C virus genotypes: clinical relevance and therapeutic implications. Chang Gung Med J 31: 16–25.
Lee MH, Yamg HI, Lu SN, Jen CL, You SL, Wang LY, Yuan Y, Litalien G, Chen CJ (2012) Clinical scoring prediction of long-term risk for hepatocellular carcinoma among hepatitis C virus infected patients. Hepatol Internal 6: 22–43.
Lee MH, Yang HI, Lu SN, Jen CL, Yeh SH, Liu CJ, Chen PJ, You SL, Wang LY, Chen WJ, Chen CJ (2010) Hepatitis C virus seromarkers and subsequent risk of hepatocellular carcinoma: Long-term predictors from a community-based cohort study. J Clin Oncol 28: 4587–4593.
Lu SN, Wang JH, Liu SL, Hung CH, Chen CH, Tung HD, Chen TM, Huang WS, Lee CM, Chen CC, Changchien CS (2006) Thrombocytopenia as a surrogate for cirrhosis and a marker for the identification of patients at high-risk for hepatocellular carcinoma. Cancer 107: 2212–2222.
Mallat A, Hezode C, Lotersztajn S (2008) Environmental factors as disease accelerators during chronic hepatitis C. J Hepatol 48: 657–665.
Manns MP, McHutchison JG, Gordon SC, Rustgi VK, Shiffman M, Reindollar R, Goodman ZD, Koury K, Ling M, Albrecht JK (2001) Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomized trial. Lancet 358: 958–965.
Marc G, Ghany MG, Nelson DR, Ghany MG, Nelson DR, Strader DB, Thomas DL, Seeff LB American Association for Study of Liver Diseases (2011) An update on treatment of genotype 1 chronic hepatitis C virus infection: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology 54 (4): 1433–1444.
McHutchison JG, Gordon SC, Schiff ER, Shiffman ML, Lee WM, Rustgi VK, Goodman ZD, Ling MH, Cort S, Albrecht JK (1998) Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C Hepatitis Interventional Therapy Group. N Engl J Med 339: 1485–1492.
Nouso K, Tanaka H, Uematsu S, Shiraga K, Okamoto R, Onishi H, Nakamura S, Kobayashi Y, Araki Y, Aoki N, Shiratori Y (2008) Cost-effectiveness of the surveillance program of hepatocellular carcinoma depends on the medical circumstances. J Gastroenterol Hepatol 23: 437–444.
Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT, Shiina S, Cheng AL, Jia JD, Obi S, Han KH, Jafri W, Chow P, Lim SG, Chawla YK, Budihusodo U, Gani RA, Lesmana CR, Putranto TA, Liaw YF, Sarin SK (2010) Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int 4: 439–474.
Papatheodoridis GV, Papadimitropoulos VC, Hadziyannis SJ (2001) Effect of interferon therapy on the development of hepatocellular carcinoma in patients with hepatitis C virus-related cirrhosis: a meta-analysis. Aliment Pharmacol Ther 15: 689–698.
Rahman El-Zayadi A, Abaza H, Shawky S, Mohamed MK, Selim OE, Badran HM (2001) Prevalence and epidemiological features of hepatocellular carcinoma in Egypt—a single center experience. Hepatol Res 19: 170–179.
Ueno S, Tanabe G, Sako K, Hiwaki T, Hokotate H, Fukukura Y, Baba Y, Imamura Y, Aikou T (2001) Discrimination value of the new western prognostic system (CLIP score) for hepatocellular carcinoma in 662 Japanese patients: Cancer of the Liver Italian Program. Hepatology 34: 529–534.
Veldt BJ, Heathcote EJ, Wedemeyer H, Reichen J, Hofmann WP, Zeuzem S, Manns MP, Hansen BE, Schalm SW, Janssen HL (2007) Sustained virological response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med 147: 677–684.
Yang HI, Sherman M, Su J, Chen PJ, Liaw YF, Iloeje UH, Chen CJ (2010) Nomograms for risk of hepatocellular carcinoma in patients with chronic hepatitis B Virus Infection. J Clin Oncol 28: 2437–2444.
Yang HI, Yuen MF, Chan HL, Han KH, Chen PJ, Kim DY, Ahn SH, Chen CJ, Wong VW, Seto WK REACH-B Working Group (2011) Risk estimation for hepatocellular carcinoma in chronic hepatitis B (REACH-B): development and validation of a predictive score. Lancet Oncol 12: 568–574.
Yuen MF, Tanaka Y, Fong DY, Fung J, Wong DK, Yuen JC, But DY, Chan AO, Wong BC, Mizokami M, Lai CL (2009) Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B. J Hepatol 50: 80–88.
Acknowledgements
The work is partially supported by the grant from Chang Gung Memorial Hospital, CMRPG8A0401.
Author contributions
Guarantor of the article: Tsung-Hui Hu.
Specific author contributions: Contributed to conception and design of the study, data interpretation, drafting and critical revision of the manuscript: Kuo-Chin Chang, Tsung-Hui Hu; contributed to the analysis and interpretation of data: Kuo-Chin Chang, Tsung-Hui Hu; contributed to the analysis and interpretation of data of manuscript: Kuo-Chin Chang, Yi-Ying Wu, Chao-Hung Hung, Sheng-Nan Lu, Chuan-Mo Lee, King-Wah Chiu, Ming-Chao Tsai, Po-Lin Tseng, Chao-Min Huang, Chung-Lung Cho, Hsiu-Hsi Chen and Tsung-Hui Hu. Tsung-Hui Hu had full access to all of the data and takes full responsibility for the veracity of the data and analysis. All authors interpreted the data, and prepared and approved the paper for submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Chang, KC., Wu, YY., Hung, CH. et al. Clinical-guide risk prediction of hepatocellular carcinoma development in chronic hepatitis C patients after interferon-based therapy. Br J Cancer 109, 2481–2488 (2013). https://doi.org/10.1038/bjc.2013.564
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.564
Keywords
This article is cited by
-
VFMAP predicted hepatocellular carcinoma development in patients with chronic hepatitis C who were treated with direct-acting antiviral and achieved sustained virologic response
Journal of Medical Ultrasonics (2023)
-
The Epidemiology of Hepatocellular Carcinoma in the USA
Current Gastroenterology Reports (2019)
-
Prediction of the very early occurrence of HCC right after DAA therapy for HCV infection
Hepatology International (2018)
-
A Circulating MicroRNA Signature Capable of Assessing the Risk of Hepatocellular Carcinoma in Cirrhotic Patients
Scientific Reports (2017)
-
Surveillance of the Patients with High Risk of Hepatocellular Cancer
Journal of Gastrointestinal Cancer (2017)