Abstract
Background:
A blood test may be a more acceptable routine colorectal cancer (CRC) screening test than faecal occult blood test, flexible sigmoidoscopy or colonoscopy, and could be safer and cheaper. We evaluated the accuracy of a serum matrix metalloproteinase (MMP9) test for CRC in a non-presenting symptomatic population.
Methods:
A cohort, aged 50–69 with lower gastrointestinal symptoms, was identified by community-based survey. Accuracy of serum MMP9 was assessed by comparison with colonoscopy. Logistic regression identified predictors of neoplasia and receiver operating characteristic curve analyses determined the cutoff to maximise the sensitivity.
Results:
Data were available for 748 patients. Overall, 46 cases of neoplasia were identified. Univariate analysis demonstrated that demographic characteristics, behavioural factors, clinical symptoms and raised serum MMP9 concentration were all significantly associated with the presence of neoplasia. Our final logistic regression model had a sensitivity of 79% and specificity of 70%.
Conclusion:
We demonstrated a significant association between serum MMP9 concentration and the presence of neoplasia. Serum MMP9 levels are raised in those with cancer and high-risk adenomas, although MMP9 estimation is likely to have the greatest predictive utility when used as part of a panel of biomarkers. Further work is required to identify biomarkers that are sufficiently accurate for implementing into routine practice.
Similar content being viewed by others
Main
Colorectal cancer (CRC) is a major public health problem (Office for National Statistics, 2010). There are over 37 000 incident cases and over 16 000 deaths in UK each year, incurring an annual expenditure of more than £300 million in surgical, adjuvant and palliative treatment (Macafee et al, 2006; Cancer Research UK, 2010a, 2010b). The 5-year age-standardised relative survival rate is improving but is still only around 50% for men and women with cancer of the colon (Cancer Research UK, 2010c). Survival is strongly associated with stage at presentation: the 5-year relative survival rate for people with localised cancer being 90% and the rate for those with distant disease only 12% (National Cancer Institute, 2010). Most CRCs arise from adenomas, and estimates of the progression rate suggest that there is a long window during which screening could facilitate early detection and adenoma removal (Chen et al, 2003). Colorectal cancer is, therefore, a suitable candidate for mass screening, and a bowel cancer-screening programme has now been introduced in UK. Screening for 60–69-year olds has commenced throughout England with an extension to include those up to age 74 ongoing (Atkin, 2006; Department of Health, 2007).
The screening programme in the UK uses the guaiac faecal occult blood test (FOBt). Meta-analysis of randomised controlled trials estimates that screening for CRC using FOBt reduces mortality from CRC by 16% (Hewitson et al, 2007), but a low positive predictive value (12% for CRC, 46% for all neoplasia) (Hardcastle et al, 1996) means that many positive tests are false and subsequent investigations incur unnecessary costs, risks and anxiety. The faecal occult blood test also has a relatively low acceptability, with reported uptake rates in UK of only 55–60% (UK Colorectal Cancer Screening Pilot Group, 2004; Weller et al, 2007). A large UK study has assessed whether flexible sigmoidoscopy screening can reduce the incidence and mortality of CRC in 55–64-year olds, and concluded that incidence is reduced by a third and mortality by 43% (Atkin et al, 2010). Despite these promising findings, flexible sigmoidoscopy remains costly, invasive and has low acceptability: <50% of people aged 50–75 years accepted an invitation for screening (Verne et al, 1998; Atkin et al, 2010). Colonoscopy is the most accurate way to detect pathology, but it requires secondary care resources, is unacceptable to some, and has an element of risk. A recent review of 37 studies concluded that the rates of perforation and haemorrhage in colonoscopy are generally <0.1% and <0.3%, respectively, but have been shown to be as high as 0.25% for perforation and 2.1% for bleeding (Juillerat et al, 2009, with overview in Arditi et al, 2009). The cost, low acceptability and risk make colonoscopy unsuitable as a routine screening test.
A blood test is likely to be more acceptable for routine screening than FOBt, flexible sigmoidoscopy or colonoscopy and could be safer and cheaper. Matrix metalloproteinases (MMPs) are proteolytic enzymes that are associated with tissue remodelling in normal and pathological processes (Collins et al, 2001). Overexpression of tissue MMPs has been correlated with progression in many tumour types, and overexpression of MMP9 has been found in colorectal adenomas (Parsons et al, 1998) and carcinomas (Garbett et al, 1999; Heslin et al, 2001). A significant positive correlation has also been found between tissue MMP9 and the stage of colorectal tumours at diagnosis (Baker and Leaper, 2003).
Overexpression of MMP9 in tumours led investigators to question whether measurement of serum levels may provide a useful diagnostic test. Serum MMP9 levels have recently been shown to be significantly elevated in CRC patients compared with controls, and higher in late-stage colorectal neoplasia as compared with early-stage disease (Dragutinovic et al, 2011). Our pilot work suggested that serum MMP9 estimation is an acceptable test and has a high sensitivity and negative predictive value for colorectal neoplasia (Hurst et al, 2007). Attention has been drawn to the need for robust serum sampling and processing protocols (Jung, 2008), but despite these concerns, serum MMP9 remains a potentially accurate, low-risk and cost-effective population-screening tool. It is, therefore, important to evaluate its accuracy as a test for CRC in the target population within primary care.
This study aimed to evaluate the accuracy of serum MMP9 as a test for CRC in non-presenting symptomatic people in the community.
Materials and methods
The design of this study is reported in detail elsewhere (Wilson et al, 2006). Briefly, a cohort aged 50–69 years with lower gastrointestinal (GI) symptoms was identified via a community-based postal survey. Accuracy of serum MMP9 estimation was assessed by comparison with the gold standard, colonoscopy.
A total of 30 randomly selected general practices in the South Birmingham area were initially invited to participate in the study, of which 19 responded positively to the invitation. Lists of eligible persons were generated from practice registers. General practitioners (GPs) excluded people under investigation or treatment for CRC, unfit for colonoscopy, unable to give informed consent, or who should not be invited to participate for any other reason (for example, recent bereavement or terminal illness). A self-administered questionnaire has been shown to be a useful tool to assess bowel symptoms with a reasonable agreement with symptoms reported from a patient–doctor interaction (Adelstein et al, 2008). A postal questionnaire assessed potential GI alarm symptoms used in the National Institute for Health and Clinical Excellence (NICE) guidelines for referral of suspected CRC (National Institute for Health and Clinical Excellence (NICE), 2005), the relative acceptability of screening tests for CRC, risk factors for CRC, and willingness to take part in the study. One reminder was sent. Respondents who described any colorectal symptoms (except only abdominal bloating and/or anal symptoms) and indicated their willingness to take part in the study were sent an information leaflet and an invitation to attend a research clinic at their general practice. At the general practice clinic, the study was described, fitness for colonoscopy assessed, a basic medical history obtained and informed consent sought.
Colonoscopies were performed in a dedicated research endoscopy unit based on the Wellcome Trust Clinical Research Facility, Queen Elizabeth Hospital, Birmingham. Colonoscopy findings were categorised as adenocarcinoma, high-risk or low-risk polyp, benign inflammatory disease of the colon, other benign disease of the colon, other benign conditions and no abnormality; the first two categories (adenocarcinoma and high-risk adenoma) being classified as neoplasia for the purposes of the analysis (Atkin and Saunders, 2002).
Two 5 ml blood samples were collected immediately before colonoscopy: one for routine analysis (haemoglobin, erythrocyte sedimentation rate, mean corpuscular volume, white blood cell count) in a purple-top tube containing EDTA (Vacuette, Greiner, Kremsmûnster, Austria), the other for MMP9 determination in a red-top tube with no additive. Samples were kept on ice until the end of the colonoscopy list at which point they were delivered to the laboratory, immediately centrifuged and the serum fraction stored at −80 °C. MMP9 levels were determined on duplicate aliquots of each sample by ELISA assay using a commercially available kit (R&D Systems, Abingdon, UK). All blood samples were analysed in the same laboratory to ensure standardisation of measurement and reporting. The technician undertaking the MMP9 ELISA assay was blinded to each patient's self-reported symptoms. All participants were flagged on the NHS Central Register to maximise the ascertainment of malignancy in those with no abnormality detected during colonoscopy.
Justification of sample size
Any test that might usefully be employed as a symptomatic screen for malignant or premalignant colorectal lesions should have a high specificity to minimise the number of non-malignancies incorrectly identified as malignant. On the basis of our pilot data and conservatively assuming a community prevalence of neoplasia of 6% (Thiis-Evensen et al, 1999; Lieberman et al, 2000), a sample of 700 people would be sufficient to estimate specificity within 4% (95% confidence). If the community prevalence of neoplasia was >6%, our estimate of specificity would have greater precision.
On the basis of our pilot data (3.2% of the age group being suitable and consenting) and assuming an average practice list of 4500 with 18% of people aged 50–69 (Office for National Statistics, 2004), 23 100 people from 29 practices were estimated to be required to identify 700 eligible participants consenting to colonoscopy and MMP9 determination. In the study itself, the required number of patients was reached from a lower number of practices than initially anticipated (n=19), due to a larger than expected average list size (9000) in participating practices.
Methods of data analysis
Data were checked for completeness and accuracy. Outliers were identified and validity was assured. Patients were classified into two pre-specified diagnostic groups; ‘neoplasia’ group: patients diagnosed with adenocarcinoma or high-risk polyps, and ‘non-neoplasia’ group: low-risk polyps, benign tumours or no abnormality.
Continuous data, including MMP9 measurements, were not normally distributed and are presented as medians and inter-quartile ranges. Univariate comparisons used the non-parametric Mann–Whitney U test. Categorical measurements are presented as proportions and compared using χ2 tests. Odds ratios, adjusted for all other predictive variables, were derived from logistic regression modelling to ‘predict’ patients with neoplasia. All appropriate factors (demographics, haematology, reported symptoms and pre-existing medical conditions) were considered in the logistic regression analyses. Actual serum MMP9 concentrations were initially used but an additional variable was created using quartiles (<144, 144 to <260, 260 to <424, 424+ ng ml−1). Each continuous variable was assessed for the assumption of linearity with outcome and appropriate transformations applied where applicable. Logistic regression analyses were based on a complete case analysis using variables (initially on their own), which were significant at or near the 10% level. This was to ensure that clinical relevance in the model was not sacrificed for parsimony. A novel two-stage logistic regression approach was used to exploit the imbalance between the number of positive and negative neoplasia patients. Taking a cutoff point of 0.05 on the predicted probability of neoplasia from the logistic regression model, all patients predicted as positive from this process were re-entered into a second logistic regression, where a cutoff of 0.05 was also taken as the most appropriate. Combining the results of this two-stage process produced a more successful predictive procedure.
Model accuracy was calculated with the aim of achieving a balance of sensitivity and specificity. Receiver operating characteristic curves were plotted, recording sensitivity vs 1-specificity for all probability cut-points of the predictive model. The probability cut-point for prediction of neoplasia for specified levels of sensitivity and specificity can be identified and was chosen to maximise sensitivity as indicated in the study protocol.
Results
Response rates
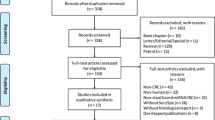
Searches of GP registers identified 21 488 patients aged 50–69, of which 133 (0.6%) were excluded by their GP and 21 355 sent a screening questionnaire (willingness to participate further and symptom profiles), (Figure 1). Responses were received from 53% of those contacted (n=11 355). Colorectal symptoms (except only abdominal bloating and/or anal symptoms) were reported by 27.5% of responders (n=3124), and 2334 (20.6%) reported willingness to take part in the evaluation of MMP9. After attendance at a research clinic, to obtain consent and evaluate fitness for colonoscopy, 751 patients were identified as being eligible for further participation, of which 748 had a colonoscopy and provided a serum sample for MMP9 determination.
Sample characteristics
Slightly lower participation rates were observed among males (χ2=122.8, P=<0.001), younger people (t=7.607, P=<0.001) and in those from the most affluent areas (χ2=20.64, P⩽0.001). However, despite these differential response rates, the final study population was similar to that of the West Midlands region and England as a whole (Office for National Statistics, 2005) with respect to gender (proportion male: 47.6% (study) vs 49.5% in West Midlands and 49.1% in England), age distribution (proportion of study age-group, i.e. 50–69, aged 60–69 years: 41.2% (study) vs 44.5% (West Midlands) vs 43.4% (England)), and deprivation score (very affluent: 13.9% (study) vs 19.4% (West Midlands) vs 25.0% (England)).
The median age of participants was 59 years (IQR: 54–63), 47.6% (n=356) were male, 92.0% (n=688) white, and 25.8% (n=193) lived in areas classified as socioeconomically deprived (Table 1). The most commonly reported symptoms were anal pain (53.0%; median duration of symptoms: 12 weeks; IQR: 3–30 weeks), change in bowel habit to looser stools (45.2%; median duration of symptoms: 10 weeks; IQR: 2.3–26), tiredness (43.7%; median duration: 12 weeks; IQR: 6–26), increased bowel frequency (39.0%; median duration: 10 weeks; IQR: 3–24), rectal bleeding (38.2%; median duration: 6 weeks; IQR: 1–30) and change in bowel consistency to harder stools (33.7%; median duration: 7 weeks; IQR: 2.8–26). Self-reported symptoms and symptom duration fulfilled the NICE guidelines for 2 week referral for 11.2% (n=84) of participants (NICE, 2005).
Colonoscopy findings
Overall, 46 cases of neoplasia (three colorectal adenocarcinomas and 43 high-risk polyps) were identified on colonoscopy; representing 6% of the study population. Other findings included low-risk polyps (n=165) and inflammatory disease (n=12).
Serum MMP9 results
The median serum MMP9 concentration was 260.3 ng ml−1; range (35.7–2133.4; IQR: 144.2–423.9) (Table 1). Crude median MMP9 concentration differed between diagnostic groups, with higher MMP9 levels observed in the neoplasia group than the non-neoplasia group. Categorisation of MMP9 levels into quartiles also demonstrated an association between higher MMP9 levels and neoplasia (χ2=16.7, P=0.001) (Table 2).
Factors associated with the presence of neoplasia
Univariate analyses, corroborated by a review of the relevant clinical literature, demonstrated that increasing age, male gender, weight loss, reporting blood in the stools, the absence of anal pain, changes in bowel habit to harder stools, smoking, drinking alcohol, raised blood pressure, raised white blood count and raised serum MMP9 concentration were all significantly associated with the presence of neoplasia (Table 2). Entering these individual neoplasia predictive factors into a logistic regression model (Table 3), along with potential confounding factors such as recent injuries, arthritis, muscular problems (which may have affected observed MMP9 measurements) and bearing in mind the expected prevalence of 6%, a cutoff on the predicted probability of neoplasia of 0.05 (5%) resulted in a sensitivity of 79% and specificity of 63%. The 249 patients predicted by the model to be in the neoplasia group were then entered into a further logistic regression, (Table 3) and results from the two stages were combined (Table 4). Receiver operating characteristic curves are also presented for the combined logistic regression (Figure 2). Using a cutoff of 0.05 in the two stage model, sensitivity was maintained at 79% but specificity was improved to 70%. Advanced statistical analysis (neural networks, recursive partitions and regression trees) did not give any improvement in model performance.
Discussion
This study investigated the association between MMP9 and colorectal neoplasia in a non-presenting cohort of patients selected on the basis of prompted self-reported symptoms. We have demonstrated a significant association between serum MMP9 concentration and the presence of neoplasia and this study supports previous work, which reported that patients referred with suspected neoplasia had significantly elevated MMP9 levels (Hurst et al, 2007).
Strengths of this study include duplicate determination of serum MMP9 levels and dual data entry to ensure reliability of results. This study has confirmed that MMP9 levels are raised in those with neoplasia, but a more detailed exploration has also identified that this relationship is non-linear. Categorisation of MMP9 concentrations into four groups enabled the predictive value of MMP9 to be modelled more accurately, given that linearity is not a statistical assumption when categorised data are used (unlike the assumptions limiting the analysis of continuous variables).
A potential limitation of our approach is the use of a non-validated questionnaire to assess patient symptoms. This was unavoidable, as no validated measures existed at the time of data collection for this study. However, the questionnaire was based on the NICE urgent referral guidelines for suspected CRC, and its robustness as a data collection tool was established during pilot work. A further limitation is that patient eligibility for study participation was determined with reference to self-reported symptoms (rather than those assessed by a physician). However, other work has shown that there is a good level of agreement between self-reported and physician-assessed symptoms (Adelstein et al, 2008). As an additional safeguard, an algorithm was incorporated into the study database so that the relevant GP could be informed if any of their patients reported symptoms that met the NICE urgent referral criteria, so that clinical investigations could be carried out if necessary.
The use of serum MMP9 estimation has been previously criticised owing to its increased level compared with plasma estimation (Jung, 2008). Matrix metalloproteinase 9 is known to be secreted by platelets and leucocytes when activated by coagulation and fibrinolytic pathways and this effect leads to the elevated levels in serum vs plasma. Some blood-sampling tubes used for serum estimations contain clot activators, which have been shown to result in a 15-fold increase in serum MMP9 levels compared with that of citrate plasma (Jung et al, 2008). This study used blood sampling tubes that did not contain any clot activators. The time elapsed between blood sampling and centrifugation is associated with higher serum MMP9 levels, with a suggested seven-fold increase after 2 h (Gerlach et al, 2007), as demonstrated for a sample left at room temperature for 2 h rather than kept on ice, as in our study. Reassuringly, our data showed no correlation between time to centrifugation and serum MMP9 level (Pearson correlation, r=−0.010, P=0.801).
One study has measured both serum and plasma MMP9 levels in patients with gastric cancer and controls (Wu et al, 2007). This study demonstrated a significant difference between plasma MMP9 levels in cancer patients compared with controls but no such difference for serum levels. Robust methods for serum collection and processing were not described and this could have explained the lack of demonstrated association.
Despite citrate plasma being the suggested sample of choice for estimating circulating MMP9 (Makowski and Ramsby, 2003), serum sampling may still be useful providing that methods of collection and processing are standardised. Serum levels have thus been shown to correlate significantly with plasma levels in two different diseases (Gerlach et al, 2009). Serum MMP9 levels have also been shown to be significantly associated with breast cancer stage and size (Motovali-Bashi et al, 2010), gastric cancer stage (Dragutinovic et al, 2009), stromal reaction in gastric cancer (Shen et al, 2000), and CRC stage (Dragutinovic et al, 2011).
The current study supports our pilot work (Hurst et al, 2007) in demonstrating that relative levels of serum MMP9 concentration may have some potential in the prediction of significant colorectal pathology. The pilot work, which assessed 300 urgent referrals to colorectal outpatients, demonstrated a difference in median MMP9 concentrations between non-neoplastic and neoplastic groups of 443 ng ml−1, The current study, with a larger population, suggests a much smaller difference between the groups (153 ng ml−1). Despite our predictive model having a reasonable sensitivity and specificity, MMP9 alone does not appear sufficiently accurate to be usefully incorporated into clinical practice. Our model, incorporating MMP9, age, gender, weight loss, blood in the stool, harder stools, anal pain, white blood count, smoking and alcohol, achieved a sensitivity of 79% and a specificity of 70%, yet this sensitivity and specificity was achievable only via a relatively complex two-stage regression model. The statistical complexity of this model prohibits its routine implementation into clinical practice.
An accurate biomarker for CRC would have potential as an alternative screening method to FOBt (which has relatively low acceptability), or as an aid to GPs in determining which patients required urgent referral for suspected CRC. Nevertheless, the size of the effect demonstrated by this study is insufficient for us to be able to suggest that serum MMP9 is such a biomarker. Ongoing work will aim to determine whether a panel of biomarkers would be sufficiently accurate to have a useful role as a screening test or to aid referral decisions. Typically, biomarker discovery studies are undertaken on selected groups of patients due to the cost and time involved in recruiting a representative sample of the population. We sent screening questionnaires to 21 355 patients aged 50–69, registered with 19 general practices and this study took 3 years to complete. Our results demonstrate the need for the collection and maintenance of serum and plasma banks to validate the accuracy of putative biomarkers.
Change history
23 January 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adelstein BA, Irwig L, Macaskill P, Katelaris PH, Jones DB, Bokey L (2008) A self administered reliable questionnaire to assess lower bowel symptoms. BMC Gastroenterol 8: 8
Arditi C, Peytremann-Bridevaux I, Burnand B, Eckardt VF, Bytzer P, Agreus L, Dubois RW, Vader JP, Froehlich F, Pittet V, Schussele Filliettaz S, Juillerat P, Gonvers JJ (2009) Appropriateness of colonoscopy in Europe (EPAGE II). Screening for colorectal cancer. Endoscopy 41: 200–208
Atkin WS (2006) Impending or pending? The national bowel cancer screening programme. BMJ 332: 742
Atkin WS, Saunders BP (2002) Surveillance guidelines after removal of colorectal adenomatous polyps. Gut 51 (Suppl 5): V6–V9
Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JMA, Parkin DM, Wardle J, Duffy SW, Cuzick J (2010) Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet 375: 1624–1633
Baker EA, Leaper DJ (2003) The plasminogen activator and matrix metalloproteinase systems in colorectal cancer: relationship to tumour pathology. Eur J Cancer 39: 981–988
Cancer Research UK (2010a) Bowel (colorectal) cancer—UK incidence statistics. http://info.cancerresearchuk.org/cancerstats/types/bowel/incidence/index.htm
Cancer Research UK (2010b) Bowel (colorectal) cancer—UK mortality statistics. http://info.cancerresearchuk.org/cancerstats/types/bowel/mortality/index.htm
Cancer Research UK (2010c) Bowel cancer—survival statistics. http://info.cancerresearchuk.org/cancerstats/types/bowel/survival/index.htm
Chen CD, Yen MF, Wang WM, Wong JM, Chen TH (2003) A case-cohort study for the disease natural history of adenoma-carcinoma and de novo carcinoma and surveillance of colon and rectum after polypectomy: implication for efficacy of colonoscopy. Br J Cancer 88: 1866–1873
Collins HM, Morris TM, Watson SA (2001) Spectrum of matrix metalloproteinase expression in primary and metastatic colon cancer: relationship to the tissue inhibitors of metalloproteinases and membrane type-1-matrix metalloproteinase. Br J Cancer 84: 1664–1670
Department of Health (2007) NHS Cancer Reform Strategy. Department of Health: London
Dragutinovic V, Izrael-Zivkovic L, Radovanovic N (2009) Relation of matrix metalloproteinase-9 to different stages of tumors in the serum of gastric cancer. Dig Dis Sci 54: 1203–1207
Dragutinovic VV, Radonjic NV, Petronijevic ND, Tatic SB, Dimitrijevic IB, Radovanovic NS, Krivokapic ZV (2011) Matrix metalloproteinase-2 (MMP-2) and -9 (MMP-9) in preoperative serum as independent prognostic markers in patients with colorectal cancer. Mol Cell Biochem 355: 173–178
Garbett EA, Reed MW, Brown NJ (1999) Proteolysis in human breast and colorectal cancer. Br J Cancer 81: 287–293
Gerlach RF, Demacq C, Jung K, Tanus-Santos JE (2007) Rapid separation of serum does not avoid artificially higher matrix metalloproteinase (MMP)-9 levels in serum versus plasma. Clin Biochem 40: 119–123
Gerlach RF, Meschiari CA, Marcaccini AM, Palei AC, Sandrim VC, Cavalli RC, Tanus-Santos JE (2009) Positive correlations between serum and plasma matrix metalloproteinase (MMP)-2 or MMP-9 levels in disease conditions. Clin Chem Lab Med 47: 888–891
Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, James PD, Mangham CM (1996) Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet 348: 1472–1477
Heslin MJ, Yan J, Johnson MR, Weiss H, Diasio RB, Urist MM (2001) Role of matrix metalloproteinases in colorectal carcinogenesis. Ann Surg 233: 786–792
Hewitson P, Irwig L, Towler B, Watson E (2007) Screening for colorectal cancer using the faecal occult blood test, Hemoccult (review). Cochrane Database Sys Rev 1: CD001216
Hurst NG, Stocken DD, Wilson S, Keh C, Wakelam MJ, Ismail T (2007) Elevated serum matrix metalloproteinase 9 (MMP-9) concentration predicts the presence of colorectal neoplasia in symptomatic patients. Br J Cancer 97: 971–977
Juillerat P, Peytremann-Bridevaux I, Vader JP, Arditi C, Schussele Filliettaz S, Dubois RW, Gonvers JJ, Froehlich F, Burnand B, Pittet V (2009) Appropriateness of colonoscopy in Europe (EPAGE II). Presentation of methodology, general results, and analysis of complications. Endoscopy 41: 240–246
Jung K (2008) Is serum matrix metalloproteinase 9 a useful biomarker in detection of colorectal cancer? Considering pre-analytical interference that may influence diagnostic accuracy. Br J Cancer 99: 553–554; author reply 555
Jung K, Klotzek S, Stephan C, Mannello F, Lein M (2008) Impact of blood sampling on the circulating matrix metalloproteinases 1, 2, 3, 7, 8, and 9. Clin Chem 54: 772–773
Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G (2000) Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med 343: 162–168
Macafee D, Gemmill L, Lund J (2006) Colorectal cancer: current care, future innovations and economic considerations. Expert Rev Pharmacoecon Outcomes Res 6: 195–206
Makowski GS, Ramsby ML (2003) Use of citrate to minimise neutrophil matrix metalloproteinase-9 in human plasma. Anal Biochem 322: 283–286.
Motovali-Bashi M, Sadeghi M, Hemmati S (2010) Serum MMP-9 level associated with initiation and progression steps of breast cancer in the Iranian population. Reprod Sci 17: 585–589
National Cancer Institute (2010) Surveillance, survival and end results. Stat Fact Sheets
National Institute for Health and Clinical Excellence (NICE) (2005) Referral guidelines for suspected cancer: Clinical guidelines CG2
Office for National Statistics (2004) Mid-2002 Population Estimates; quinary age groups and sex for local authorities in England and Wales; estimated resident population. http://www.statistics.gov.uk/statbase/Product.asp?vlnk=10687&image.x=18&image.y=9
Office for National Statistics (2005) T 15: Mid-2005 Population Estimates; Quinary age groups and sex for Primary Care Organisations (PCOs) for England; estimated resident population (experimental). On boundaries as at 1 October 2006 http://www.statistics.gov.uk/StatBase/ssdataset.asp?vlnk=9585&Pos=2&ColRank=1&Rank=96
Office for National Statistics (2010) Bowel cancer. Colorectal cancer incidence and mortality by sex, England, 1971–2007. http://www.statistics.gov.uk/CCI/nugget.asp?ID=2162&Pos=&ColRank=1&Rank=374
Parsons SL, Watson SA, Collins HM, Griffin NR, Clarke PA, Steele RJ (1998) Gelatinase (MMP-2 and -9) expression in gastrointestinal malignancy. Br J Cancer 78: 1495–1502
Shen KH, Chi CW, Lo SS, Kao HL, Lui WY, Wu CW (2000) Serum matrix metalloproteinase-9 level associated with stromal reaction in patients with gastric cancer. Anticancer Res 20: 1307–1310
Thiis-Evensen E, Hoff GS, Sauar J, Majak BM, Vatn MH (1999) Flexible sigmoidoscopy or colonoscopy as a screening modality for colorectal adenomas in older age groups? Findings in a cohort of the normal population aged 63–72 years. Gut 45: 834–839
UK Colorectal Cancer Screening Pilot Group (2004) Results of the first round of a demonstration pilot of screening for colorectal cancer in the United Kingdom. BMJ 329: 133
Verne JE, Aubrey R, Love SB, Talbot IC, Northover JM (1998) Population based randomized study of uptake and yield of screening by flexible sigmoidoscopy compared with screening by faecal occult blood testing. BMJ 317: 182–185
Weller D, Coleman D, Robertson R, Butler P, Melia J, Campbell C, Parker R, Patnick J, Moss S (2007) The UK colorectal cancer screening pilot: results of the second round of screening in England. Br J Cancer 97: 1601–1605
Wilson S, Wakelam M, Hobbs FDR, Ryan A, Dunn J, Redman V, Patrick F, Colbourne L, Martin A, Ismail T (2006) Evaluation of the accuracy of serum MMP-9 as a test for colorectal cancer in a primary care population: study protocol. BMC Cancer 6: 258
Wu CY, Wu MS, Chiang EP, Chen YJ, Chen CJ, Chi NH, Shih YT, Chen GH, Lin JT (2007) Plasma matrix metalloproteinase-9 level is better than serum matrix metalloproteinase-9 level to predict gastric cancer evolution. Clin Cancer Res 13: 2054–2060
Acknowledgements
Cancer Research UK (CRUK) funded this study. We thank the general practices, hospital staff and all the men and women who participated. We also thank the Midland Research Practices Consortium (MidReC) for their help.
Ethical approval
Ethical approval for this study was obtained from South Birmingham Local Research Ethics Committee (Ref 05/Q2707/133). R&D approval was granted by Birmingham and Solihull PCT Consortium (Ref PC66/769), Redditch and Bromsgrove Primary Care Trust, and University Hospitals Birmingham R&D Office (Queen Elizabeth Hospital, Birmingham).
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Wilson, S., Damery, S., Stocken, D. et al. Serum matrix metalloproteinase 9 and colorectal neoplasia: a community-based evaluation of a potential diagnostic test. Br J Cancer 106, 1431–1438 (2012). https://doi.org/10.1038/bjc.2012.93
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.93
Keywords
This article is cited by
-
Serum matrix metalloproteinase-9 in colorectal cancer family-risk population screening
Scientific Reports (2015)
-
Assessing the value of matrix metalloproteinase 9 (MMP9) in improving the appropriateness of referrals for colorectal cancer
British Journal of Cancer (2013)