Abstract
Background:
The pathogenesis of lymph node metastases in preinvasive breast cancer – ductal carcinoma in situ (DCIS) – remains controversial. The one-step nucleic acid amplification (OSNA) assay is a novel molecular method that can assess a whole node and detect clinically relevant metastases. In this retrospective cohort study, we determined the performance of the OSNA assay in DCIS and the pathogenesis of node-positive DCIS.
Methods:
The subjects consisted of 623 patients with DCIS who underwent sentinel lymph node (SN) biopsy. Of these, 2-mm-sectioned nodes were examined using frozen-section (FS) histology in 338 patients between 2007 and 2009, while 285 underwent OSNA whole node assays between 2009 and 2011. The SN-positivity rate was compared between cohorts, and the characteristics of OSNA-positive DCIS were investigated.
Results:
The OSNA detected more cases of SN metastases than FS histology (12 out of 285, 4.2% vs 1 out of 338, 0.3%). Most of the metastases were micrometastases. The characteristics of high-risk DCIS (i.e., mass formation, size, grade, and comedo) and preoperative breast biopsy (i.e., methods or time to surgery) were not valid for OSNA assay–positive DCIS.
Conclusion:
The OSNA detects more SN metastases in DCIS than FS histology. Further examination of the primary tumours and follow-up of node-positive DCIS are needed to elucidate the pathogenesis.
Similar content being viewed by others
Main
Ductal carcinoma in situ (DCIS), the most common type of preinvasive breast cancer, consists of clonal proliferation of cells that appear malignant and accumulate within the lumen of mammary ducts (Burstein et al, 2004). By definition, DCIS does not metastasise to the lymph nodes as the tumour is limited to the epithelial layer and does not reach lymphatic vessels.
Axillary surgery in patients with DCIS has changed dramatically over the years (Shapiro-Wright and Julian, 2010). In the early 1980s, axillary dissection was the standard procedure, but metastases were rarely detected using conventional histology (<1%; Silverstein et al, 1987). In the 1990s, the sentinel lymph node (SN) concept was introduced for the clinical management of breast cancer (Krag et al, 1993; Giuliano et al, 1994). Among patients with a preoperative diagnosis of DCIS, SN biopsy is used for patients with a higher likelihood of developing occult invasive lesions (high-risk DCIS: i.e., large, high-grade, or comedo-type tumours; or palpable or mammographic masses) and those undergoing mastectomy (McMasters et al, 2002; Ansari et al, 2008). To prevent false-negative diagnoses, pathologists began to concentrate on the evaluation of SNs by adopting a step-sectioning procedure (Giuliano et al, 1995). Intensive examination of SNs resulted in an increase in the detection of metastases in patients with DCIS. A meta-analysis showed that the incidence of SN metastases is 3.7% in patients with a postoperative diagnosis of DCIS (Ansari et al, 2008).
The diagnostic accuracy of both DCIS and lymph node metastases is dependent on the rigour of the examination. If fewer sections from the primary tumour or lymph node are examined, more microinvasions or micrometastases may not be identified. In most of the previous reports on DCIS with nodal metastasis, histological examination procedures for primary tumours are not mentioned in detail or do not cover the entire tumour spread, particularly in large tumours. Thus, these previous reports do not rigorously exclude microinvasive cancers.
Similarly, conventional histopathological examinations of lymph nodes are non-standardised and have limited ability to detect metastases accurately due to the partial evaluation of nodes. The one-step nucleic acid amplification (OSNA) assay (Sysmex, Kobe, Japan) was developed to overcome these limitations of the histopathological examination of lymph nodes. This assay is approved and commercialised for clinical use throughout Europe and Japan. It can be used to assess whole lymph nodes, and yields semi-quantitative results for the detection of clinically relevant nodal metastases >0.2 mm in size by the detection and amplification of cytokeratin 19 (CK19) mRNA (Tsujimoto et al, 2007; Visser et al, 2008; Schem et al, 2009; Tamaki et al, 2009; Feldman et al, 2011; Snook et al, 2011). The OSNA assay can distinguish macrometastases (>2 mm in size) and micrometastases (>0.2 mm to ⩽2 mm in size) from low-volume metastases corresponding to isolated tumour cells (⩽0.2 mm in size) according to the Cancer Staging Manual of the Union International Contre le Cancer (UICC; Sobin et al, 2009). Previously, we showed that when the OSNA whole node assay is applied to invasive breast cancers, more metastases, particularly micrometastases, are detected than those detected by routine histopathological examinations (Osako et al, 2011a).
Therefore, we hypothesise that a combination of detailed histological examination of primary breast tumours and the OSNA whole lymph node assay can accurately elucidate the incidence and characteristics of node-positive DCIS and suggest the pathogenesis. In this single-centre retrospective cohort study, we compared the performance of the detection of SN metastases using the OSNA whole node assay and routine frozen-section (FS) histology using a 2-mm-sectioned lymph node in patients with DCIS examined in detail; this was done to reveal the non-sentinel node (nonSN) status as well as the clinicopathological characteristics of OSNA assay–positive patients.
Patients and methods
Patients and tumours
The study subjects consisted of consecutive patients with pure DCIS who underwent SN biopsy between January 2007 and March 2011 at the Cancer Institute Hospital, Tokyo, Japan. The exclusion criteria were as follows: (1) SN mapping without the use of a radioisotope tracer, (2) metastasis detected only in nonSNs, (3) previous excision of a primary tumour, (4) heterochronous ipsilateral breast cancer recurrence, (5) neoadjuvant drug therapy, and (6) male gender. Patients who underwent FS histology for detection of SN metastases after the introduction of the OSNA assay were also excluded. From 21 April 2009, onward, the OSNA assay, instead of the FS histology method, was used for the detection of SN metastases in our institute. Therefore, this study involves two distinct cohorts categorised on the basis of the method used for the detection of SN metastases: patients who were earlier assessed using FS histology examination (FS cohort) and patients who were later assessed by the OSNA assay (OSNA cohort). Furthermore, in September 2009, we switched the method of detection of further nonSN metastases from a permanent histological method to the OSNA assay.
When a patient had several mammographic findings, the priority for the determination of the findings was mass, calcification, architectural distortion, and focal asymmetric density. When a patient had several presurgical breast biopsies, the priority for the determination of the biopsy method was incisional biopsy, vacuum-assisted needle biopsy, needle biopsy without vacuum assistance, ductoscopic biopsy, and fine-needle aspiration cytology. The immunohistochemical cutoff for oestrogen and progesterone receptor positivity was 10% cell positivity irrespective of the intensity.
Histological examination of primary tumours
Partial mastectomy materials were sectioned continuously from the nipple side to the periphery at 5-mm intervals. All sections were histologically examined with haematoxylin and eosin staining. Total mastectomy materials were sectioned continuously from the nipple to the periphery at 5- to 7-mm intervals. The sectioning was performed to cover the entire tumour spread using macroscopic and radiologic findings as references. Most of the sections within the tumour spread were histologically confirmed with haematoxylin and eosin staining.
Sentinel lymph node biopsy procedure
The radioisotope tracer used was 1.5 mCi/ml 99mTc-phytate. One day prior to surgery, the tracer was injected into the intradermal and subdermal space in the tumour area and retro-tumoural space. In all cases, lymphoscintigraphy was performed 1 h after the injection. In addition, 2- to 3-ml indigo carmine (a vital dye; Daiichi Sankyo, Tokyo, Japan) was injected in the peri-tumoural space or areola at surgery. Before surgery for the primary tumour, SNs were identified using a hand-held gamma-probe with guidance from the staining of the vessels and nodes. Radioactive and/or blue nodes were considered SNs and excised. When one or more SNs were positive, complete axillary lymph node dissection was performed immediately.
Frozen-section histology for SNs
All SNs were step sectioned at 2-mm intervals by surgeons. Two serial sections were taken for each 2-mm lymph node section. Each section was intraoperatively assessed by FS histology with haematoxylin and eosin staining. Immunohistochemistry was not routinely used for the evaluation of SNs. The FS specimens were reviewed and classified into three categories – macrometastasis, micrometastasis, or negative – according to the seventh edition of the UICC Staging Manual (Sobin et al, 2009).
Permanent histology for nonSNs
All nonSNs in axillary dissection materials were cut in half along the long axis after formalin fixation. One of the cut surfaces was examined after haematoxylin and eosin staining. Approximately 5–7 nodes were embedded in paraffin in a single cassette. Immunohistochemical staining was not used to evaluate nonSNs.
One-step nucleic acid amplification assay for SNs and nonSNs
The OSNA assay for lymph nodes has been described previously in detail (Tsujimoto et al, 2007). Briefly, after the removal of extranodal tissue, whole lymph nodes were homogenised with 4-ml lysis buffer solution (Lynorhag; Sysmex, Kobe, Japan) and centrifuged at 10 000 g at room temperature. A total of 2-μl supernatant was analysed with the RD-100i System (Sysmex), an automated molecular detection system that uses a reverse transcription loop–mediated isothermal amplification method (Notomi et al, 2000), and the LynoampBC Kit (Sysmex). The degree of amplification was detected on the basis of a reaction by-product, pyrophosphate (Mori et al, 2001). The resultant change in turbidity on precipitation of magnesium pyrophosphate in turn correlated with the CK19 mRNA copy number per microlitre of the original lysate via a standard curve established beforehand with three calibrators containing different CK19 mRNA copy numbers. A standard positive control sample containing 5000, copies/μl CK19 mRNA and a negative control sample containing no CK19 mRNA were used for quality assurance in every assay run. Lymph nodes that exceeded the specified maximum weight of 600 mg were cut into two or more pieces and processed as separate nodes. Thus, up to four lymph nodes were analysed in a single run.
The numbers of CK19 mRNA copies per microlitre in the measurement sample as well as the 1 : 10 diluted sample were calculated; based on these copy numbers, the result (i.e., positive or negative) was assessed in accordance with the cutoff level determined in the study of Tsujimoto et al (2007). Positive nodes were categorised as ++, +, or +I (positive with inhibited reaction), according to the criteria shown in Table 1. Positive (++) and (+) were considered equivalent to UICC macrometastasis and micrometastasis, respectively (Tsujimoto et al, 2007). Positive (+I) was considered to include both UICC macro- and micrometastasis.
All SNs and a small number of nonSNs surrounding SNs were assessed intraoperatively. Almost all nonSNs in axillary dissection materials were assessed postoperatively. The nonSNs were placed in tubes and immediately frozen at −80 °C in a deep freezer (My Bio Cube; Nihon Freezer, Tokyo, Japan). The frozen nonSNs were assessed at a later date, using the same protocol, as fresh nodes.
Statistical analyses
To compare the patient characteristics of the FS and OSNA cohorts, Student’s t-test (for age), the Mann–Whitney U-test (for the period from breast biopsy to surgery, number of SNs removed, and number of specimens examined), and the χ2-test with Yates’ continuity correction (for other characteristics) were performed. To compare the detection rates of SN metastases between the FS and OSNA cohorts, a two-population Z-test with Yates’ continuity correction was performed for SN metastases (positive vs negative). To reveal the characteristics of patients with OSNA assay–positive DCIS, Student’s t-test, the Mann–Whitney U-test, and the χ2-test with Yates’ continuity correction were performed for the above-mentioned characteristics in the OSNA cohort. P-values <0.05 were considered statistically significant, and confidence intervals were set at the 95% level. All statistical analyses were performed with the statistical software R (version 2.10.1, http://www.r-project.org/).
Results
Patient characteristics
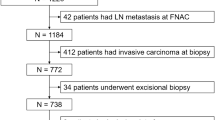
Between January 2007 and March 2011, 828 patients were diagnosed with pure DCIS of the breast, and 695 (83.9%) of them underwent SN biopsy. Of these 695 patients, 623 were eligible for this study. The FS and OSNA cohorts contained 338 and 285 patients, respectively. The demographic characteristics of both cohorts are presented in Table 2. All patients were Asian women. Almost all the characteristics of the two cohorts, except presurgical biopsy method (needle biopsy vs others), were similar; the proportion of patients in the OSNA cohort who received needle biopsy was higher than that in the FS cohort (OSNA 209 out of 285, 73.3% vs FS 219 out of 338, 64.8%; P=0.022). The histological characteristics of the primary tumour were similar between both cohorts. The median number of specimens examined from surgically removed breast tissue was more than 20 blocks for both cohorts.
Detection of SN metastases
Sentinel lymph nodes were positive for metastasis more frequently in the OSNA cohort than in the FS cohort (OSNA 12 out of 285, 4.2%; 95% confidence interval 2.3–7.4% vs FS 1 out of 339, 0.3%; 95% confidence interval 0.0–1.9%, P=0.0018; Table 3).
Sentinel lymph node and nonSN status in SN-positive patients
All SN-positive patients underwent axillary lymph node dissection. In the FS cohort, only one patient had SN metastasis. In this patient, two nodes involved macrometastases (case #1, Table 4); however, there were no metastases in nonSNs. In the OSNA cohort, 12 patients had SN metastases (cases #2–13). In all 12 patients, SN metastasis was confined to one node, and the CK19 mRNA copy number was low (median, 430 copies/μl; mean, 652 copies/μl; range, 250–1400 copies/μl). Of these 12 patients, 4 underwent permanent histology examination (cases #2–5) and 8 underwent the OSNA assay (cases #6–13) for the detection of nonSN metastases. Of the latter eight patients, three had nonSN metastases (cases #8, #11, and #12) and two had low CK19 mRNA expression in nonSNs (cases #6 and #10).
Characteristics of patients with OSNA assay–positive DCIS
In the OSNA cohort, 12 patients had SN metastases and 273 did not have metastases. The number of SNs removed in the SN-positive patients was larger than that in the SN-negative patients (median, 3; range, 1–6 vs median, 2; range, 1–7, respectively, P=0.045; Table 5). Other characteristics including pathological size, grade, subtype, palpability, mammographic finding, breast biopsy method, and the period from biopsy to surgery were not significantly different between cohorts.
Discussion
This study features a combination of detailed histological examination of primary breast tumours to exclude microinvasive cancers and whole lymph node analysis using the OSNA assay to detect micrometastases >0.2 mm in size. To our knowledge, this is the first report in which all whole SNs in DCIS were evaluated using a molecular assay. The incidence of SN-positive DCIS in the FS cohort was very low compared with the results of previous studies (Ansari et al, 2008), even considering that FS histology is a less-precise examination than permanent histology (Layfield et al, 2011). Thus, the histological examination procedure for primary tumours adapted in this study appears to exclude patients with microinvasive cancers more thoroughly than procedures used in previous studies. In the patients with DCIS examined in detail, the OSNA whole node assay detected more cases of SN metastases than routine FS histology. Moreover, 4% of DCIS patients were found to have SN metastases.
One of the possible pathogeneses of nodal metastasis in DCIS is true metastases from occult invasive lesions of primary tumours. Occult invasive lesions can manifest in two forms: (1) occult invasion between the specimen surfaces of the surgical materials and (2) multicentric occult cancer in the conserved breast (i.e., in partial mastectomy cases) or in materials not examined (i.e., in total mastectomy cases). In terms of occult invasion between the specimen surfaces, although the present histological examination procedure for primary tumours is extensive, invasive lesions of <5 mm in size can be missed by chance. Ductal carcinoma in situ patients who have large, high-grade or comedo-type tumours, or palpable or mammographic masses are more likely to have occult invasion (Ansari et al, 2008). However, none of these characteristics of high-risk DCIS were significantly correlated with OSNA-positive tumours. Furthermore, the possibility of multicentric cancers appears to be low, because almost all patients in this study had preoperative mammography, ultrasonography, and magnetic resonance imaging.
Another possible pathogenesis is false-positive results from the OSNA assay. Lymph nodes with contaminating epithelial cells, benign intranodal inclusions, or iatrogenic dissemination of benign epithelial or tumour cells can cause false-positive diagnoses. However, as we will discuss later, the incidences of such events appear to be low. Several clinical trials demonstrate a high specificity (96–98%) for the OSNA assay (Visser et al, 2008; Schem et al, 2009; Tamaki et al, 2009; Feldman et al, 2011; Snook et al, 2011).
The incidence of false-positive diagnoses appears to be low for several reasons. First, the rigorous SN biopsy with radioisotope tracer before breast surgery and the removal of extranodal tissue before homogenisation minimises contamination. Second, although benign intranodal epithelial inclusions such as heterotopic mammary glands, benign glandular inclusions, and benign Mullerian inclusions are inevitable (Maiorano et al, 2003; Peng et al, 2008; Corben et al, 2010; Fellegara et al, 2011), their presence is very rare in axillary lymph nodes. In a large series with more than 3500 specimens, only 7 occurrences (<0.2%) of ectopic breast tissue in SNs were identified (Maiorano et al, 2003). Moreover, the malignant transformation of benign epithelial inclusions is hypothesised in the genesis of nodal metastases in association with DCIS. However, only few cases of pelvic or para-aortic lymph nodes have been reported to date (Prade et al, 1995). Third, a prior invasive diagnostic biopsy can iatrogenically displace benign epithelial or tumour cells into the lymphatic system; these dislocated cells can be passively transported to the SN (King et al, 2004; Moore et al, 2004; Bleiweiss et al, 2006; Tvedskov et al, 2012). The results of a large cohort study show that surgical excision biopsy increases isolated tumour cells and micrometastases in SNs (Tvedskov et al, 2012). In this study, the number of patients who had preoperative needle biopsy of the primary breast lesion in the OSNA cohort was higher than that in the FS cohort. This supports the hypothesis that a mechanical displacement of epithelial cells rather than true metastatic deposition explains the higher detection rate of positive SNs with the OSNA assay. However, we did not find any significant differences in breast biopsy methods or the period from biopsy to surgery between the OSNA-positive and OSNA-negative patients. Moreover, an iatrogenic dissemination usually does not spread to nonSNs (Tvedskov et al, 2012). The OSNA assay can evaluate nonSN status more accurately than routine single-section permanent histology (Osako et al, 2011a). In this study, five of eight patients whose nonSNs were assessed by the OSNA assay had metastasis or low CK19 mRNA expression in their nonSNs. Thus, true metastases could have occurred in at least 60% of the patients with SN-positive DCIS.
Therefore, true metastases from occult invasion between the specimen surfaces or iatrogenic dissemination of benign epithelial or tumour cells can be considered the pathogenesis of nodal metastases in DCIS. However, the clinicopathological characteristics and nonSN status of SN-positive DCIS do not clearly support either pathogenesis. These results might be related to the low number of OSNA assay–positive patients. Further deeper-cut examination of the primary tumours and follow-up of the node-positive DCIS patients are needed to elucidate their pathogeneses. Deeper-cut examinations will reveal whether node-positive DCIS has occult invasion. In addition, the follow-up of node-positive DCIS patients will elucidate the prognostic impact of nodal metastases, as iatrogenic dissemination does not have any prognostic impact.
A potential limitation of the use of the OSNA whole node assay is the inability to store materials for other analyses. This could be a critical limitation when planning therapeutic strategies for DCIS patients with nodal metastasis. In fact, in a scenario of tumour heterogeneity, it is not always the case that the in situ component should have the same hormone receptor status and HER2 profile of the nodal metastases. Another potential limitation in the use of the OSNA whole node assay for the analysis of nodes is its inability to find other possible coexisting pathologies such as lymphomas.
The management of SN-positive DCIS through further axillary lymph node dissection and adjuvant systemic therapy remains controversial (Ansari et al, 2008). Regarding axillary dissection, it is difficult to manage patients who have metastases with DCIS differently from those with invasive cancer, because surgeons cannot know the final pathology of the primary tumour intraoperatively. For invasive cancers, current guidelines recommend further axillary dissection for patients with SN metastases (Lyman et al, 2005; NCCN, 2011). Therefore, in this study, all patients with node-positive DCIS underwent further axillary dissection. According to the results of the American College of Surgeons Oncology Group Z-0011 trial, further axillary dissection is unnecessary for patients with only one or two positive SNs who have undergone partial mastectomy with radiation therapy and systemic chemotherapy (Giuliano et al, 2010). However, systemic chemotherapy is sometimes merely overtreatment. Furthermore, there is no evidence supporting the omission of safe axillary dissection in patients who have undergone total mastectomy.
Adjuvant systemic therapy for patients with node-positive DCIS is also controversial. Considering possible occult microinvasion in primary tumours and the low tumour burden in SNs, node-positive DCIS might be treated as pT1miN1miM0 according to the seventh UICC staging. For patients with pT1miN1miM0 tumours, the current guidelines recommend considering endocrine therapy for hormone receptor–positive tumours and chemotherapy for hormone receptor–negative tumours (NCCN, 2011). However, adjuvant systemic therapy, particularly chemotherapy, can be overtreatment for node-positive DCIS as the 10-year survival rate of pure DCIS approaches 98% (Ernster et al, 2000), and the possibility of iatrogenic epithelial dissemination cannot be ruled out.
In conclusion, whole lymph node analysis using the OSNA assay detected more SN metastases than FS histology with 2-mm-sectioned nodes in DCIS patients examined in detail. The true metastases from occult invasion of the primary tumour or iatrogenic dissemination of benign epithelial or tumour cells by the preoperative breast biopsy can be cited as the pathogenesis of nodal metastases in DCIS. However, the clinicopathological characteristics and nonSN status of SN-positive DCIS do not clearly support either pathogenesis. Further deeper-cut examination of the primary tumours and follow-up of node-positive DCIS patients are needed to clearly elucidate the pathogenesis.
Change history
23 January 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ansari B, Ogston SA, Purdie CA, Adamson DJ, Brown DC, Thompson AM (2008) Meta-analysis of sentinel node biopsy in ductal carcinoma in situ of the breast. Br J Surg 95(5): 547–554
Bleiweiss IJ, Nagi CS, Jaffer S (2006) Axillary sentinel lymph nodes can be falsely positive due to iatrogenic displacement and transport of benign epithelial cells in patients with breast carcinoma. J Clin Oncol 24(13): 2013–2018
Burstein HJ, Polyak K, Wong JS, Lester SC, Kaelin CM (2004) Ductal carcinoma in situ of the breast. N Engl J Med 350(14): 1430–1441
Corben AD, Nehhozina T, Garg K, Vallejo CE, Brogi E (2010) Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma. Am J Surg Pathol 34(8): 1211–1216
Ernster VL, Barclay J, Kerlikowske K, Wilkie H, Ballard-Barbash R (2000) Mortality among women with ductal carcinoma in situ of the breast in the population-based surveillance, epidemiology and end results program. Arch Intern Med 160(7): 953–958
Feldman S, Krishnamurthy S, Gillanders W, Gittleman M, Beitsch PD, Young PR, Streck CJ, Whitworth PW, Levine EA, Boolbol S, Han LK, Hermann R, Hoon DS, Giuliano AE, Meric-Bernstam F (2011) A novel automated assay for the rapid identification of metastatic breast carcinoma in sentinel lymph nodes. Cancer 117(12): 2599–2607
Fellegara G, Carcangiu ML, Rosai J (2011) Benign epithelial inclusions in axillary lymph nodes: report of 18 cases and review of the literature. Am J Surg Pathol 35(8): 1123–1133
Giuliano AE, Dale PS, Turner RR, Morton DL, Evans SW, Krasne DL (1995) Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg 222(3): 394–399; discussion 399-401
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, McCall LM, Morrow M (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305(6): 569–575
Giuliano AE, Kirgan DM, Guenther JM, Morton DL (1994) Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg 220(3): 391–398; discussion 398-401
Giuliano AE, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch AM, Saha S, Hunt KK, Morrow M, Ballman K (2010) Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg 252(3): 426–432; discussion 432-33
King TA, Ganaraj A, Fey JV, Tan LK, Hudis C, Norton L, Cody HS, Borgen PI (2004) Cytokeratin-positive cells in sentinel lymph nodes in breast cancer are not random events: experience in patients undergoing prophylactic mastectomy. Cancer 101(5): 926–933
Krag DN, Weaver DL, Alex JC, Fairbank JT (1993) Surgical resection and radiolocalization of the sentinel lymph node in breast cancer using a gamma probe. Surg Oncol 2(6): 335–339; discussion 340
Layfield DM, Agrawal A, Roche H, Cutress RI (2011) Intraoperative assessment of sentinel lymph nodes in breast cancer. Br J Surg 98(1): 4–17
Lyman GH, Giuliano AE, Somerfield MR, Benson AB, Bodurka DC, Burstein HJ, Cochran AJ, Cody HS, Edge SB, Galper S, Hayman JA, Kim TY, Perkins CL, Podoloff DA, Sivasubramaniam VH, Turner RR, Wahl R, Weaver DL, Wolff AC, Winer EP (2005) American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol 23(30): 7703–7720
Maiorano E, Mazzarol GM, Pruneri G, Mastropasqua MG, Zurrida S, Orvieto E, Viale G (2003) Ectopic breast tissue as a possible cause of false-positive axillary sentinel lymph node biopsies. Am J Surg Pathol 27(4): 513–518
McMasters KM, Chao C, Wong SL, Martin RC, Edwards MJ (2002) Sentinel lymph node biopsy in patients with ductal carcinoma in situ: a proposal. Cancer 95(1): 15–20
Moore KH, Thaler HT, Tan LK, Borgen PI, Cody HS (2004) Immunohistochemically detected tumor cells in the sentinel lymph nodes of patients with breast carcinoma: biologic metastasis or procedural artifact? Cancer 100(5): 929–934
Mori Y, Nagamine K, Tomita N, Notomi T (2001) Detection of loop-mediated isothermal amplification reaction by turbidity derived from magnesium pyrophosphate formation. Biochem Biophys Res Commun 289(1): 150–154
NCCN (2011) National Comprehensive Cancer Nnetwork clinical practice guidelines in oncology. Breast cancer ver. 2, 2011. http://www.nccn.org/professionals/physician_gls/PDF/breast.pdf
Notomi T, Okayama H, Masubuchi H, Yonekawa T, Watanabe K, Amino N, Hase T (2000) Loop-mediated isothermal amplification of DNA. Nucleic Acids Res 28(12): E63
Osako T, Iwase T, Kimura K, Yamashita K, Horii R, Akiyama F (2011a) Accurate staging of axillary lymph nodes from breast cancer patients using a novel molecular method. Br J Cancer 105(8): 1197–1202
Osako T, Iwase T, Kimura K, Yamashita K, Horii R, Yanagisawa A, Akiyama F (2011b) Intraoperative molecular assay for sentinel lymph node metastases in early stage breast cancer: a comparative analysis between one-step nucleic acid amplification whole node assay and routine frozen section histology. Cancer 117(19): 4365–4374
Peng Y, Ashfaq R, Ewing G, Leitch AM, Molberg KH (2008) False-positive sentinel lymph nodes in breast cancer patients caused by benign glandular inclusions: report of three cases and review of the literature. Am J Clin Pathol 130(1): 21–27; quiz 146
Prade M, Spatz A, Bentley R, Duvillard P, Bognel C, Robboy SJ (1995) Borderline and malignant serous tumor arising in pelvic lymph nodes: evidence of origin in benign glandular inclusions. Int J Gynecol Pathol 14(1): 87–91
Schem C, Maass N, Bauerschlag DO, Carstensen MH, Loning T, Roder C, Batic O, Jonat W, Tiemann K (2009) One-step nucleic acid amplification-a molecular method for the detection of lymph node metastases in breast cancer patients; results of the German study group. Virchows Arch 454(2): 203–210
Shapiro-Wright HM, Julian TB (2010) Sentinel lymph node biopsy and management of the axilla in ductal carcinoma in situ. J Natl Cancer Inst Monogr 2010(41): 145–149
Silverstein MJ, Rosser RJ, Gierson ED, Waisman JR, Gamagami P, Hoffman RS, Fingerhut AG, Lewinsky BS, Colburn W, Handel N (1987) Axillary lymph node dissection for intraductal breast carcinoma—is it indicated? Cancer 59(10): 1819–1824
Snook KL, Layer GT, Jackson PA, de Vries CS, Shousha S, Sinnett HD, Nigar E, Singhal H, Chia Y, Cunnick G, Kissin MW (2011) Multicentre evaluation of intraoperative molecular analysis of sentinel lymph nodes in breast carcinoma. Br J Surg 98(4): 527–535
Sobin LH, Gospodarowicz MK, Wittekind C (2009) UICC International Union Against Cancer. TNM Classification of Malignant Tumours, 7th edn. Wiley-Blackwell: New York, NY
Tamaki Y, Akiyama F, Iwase T, Kaneko T, Tsuda H, Sato K, Ueda S, Mano M, Masuda N, Takeda M, Tsujimoto M, Yoshidome K, Inaji H, Nakajima H, Komoike Y, Kataoka TR, Nakamura S, Suzuki K, Tsugawa K, Wakasa K, Okino T, Kato Y, Noguchi S, Matsuura N (2009) Molecular detection of lymph node metastases in breast cancer patients: results of a multicenter trial using the one-step nucleic acid amplification assay. Clin Cancer Res 15(8): 2879–2884
Tsujimoto M, Nakabayashi K, Yoshidome K, Kaneko T, Iwase T, Akiyama F, Kato Y, Tsuda H, Ueda S, Sato K, Tamaki Y, Noguchi S, Kataoka TR, Nakajima H, Komoike Y, Inaji H, Tsugawa K, Suzuki K, Nakamura S, Daitoh M, Otomo Y, Matsuura N (2007) One-step nucleic acid amplification for intraoperative detection of lymph node metastasis in breast cancer patients. Clin Cancer Res 13(16): 4807–4816
Tvedskov TF, Jensen MB, Kroman N, Balslev E (2012) Iatrogenic displacement of tumor cells to the sentinel node after surgical excision in primary breast cancer. Breast Cancer Res Treat 131(1): 223–229
Visser M, Jiwa M, Horstman A, Brink AA, Pol RP, van Diest P, Snijders PJ, Meijer CJ (2008) Intra-operative rapid diagnostic method based on CK19 mRNA expression for the detection of lymph node metastases in breast cancer. Int J Cancer 122(11): 2562–2567
Acknowledgements
We thank all staff working in the Breast Oncology Center of the Cancer Institute Hospital of the Japanese Foundation for Cancer Research, including Masujiro Makita, Seiichiro Nishimura, Yumi Miyagi, Kotaro Iijima, Hidetomo Morizono, Takehiko Sakai, Masahiko Tanabe, and Rie Gokan. In addition, we also thank all staff working in the Division of Pathology of the Cancer Institute of the Japanese Foundation for Cancer Research, including Yuichi Ishikawa, Kengo Takeuchi, Kyoko Yamashita, Tsu Miyagi, and Yuki Takano. Finally, we are grateful to Tadashi Kiniwa, Kazuki Kishi, and Kenji Iwakabe (Sysmex Corporation) for their helpful advice. This work was supported by a Grant-in-Aid for Young Scientists (B) (no. 21791264) from the Japanese Ministry of Education, Culture, Sports, Science, and Technology, and a Research Grant from the Foundation for Promotion of Cancer Research in Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Osako, T., Iwase, T., Kimura, K. et al. Incidence and possible pathogenesis of sentinel node micrometastases in ductal carcinoma in situ of the breast detected using molecular whole lymph node assay. Br J Cancer 106, 1675–1681 (2012). https://doi.org/10.1038/bjc.2012.168
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.168
Keywords
This article is cited by
-
Prognostic impact and possible pathogenesis of lymph node metastasis in ductal carcinoma in situ of the breast
Breast Cancer Research and Treatment (2019)
-
A new molecular-based lymph node staging classification determines the prognosis of breast cancer patients
British Journal of Cancer (2017)
-
Isolated tumour cells and micrometastases in intraductal breast cancer: a simple mechanical question in some cases
British Journal of Cancer (2013)
-
Reply: Isolated tumour cells and micrometastases in intraductal breast cancer: a simple mechanical question in some cases
British Journal of Cancer (2013)
-
Molecular detection of lymph node metastasis in breast cancer patients treated with preoperative systemic chemotherapy: a prospective multicentre trial using the one-step nucleic acid amplification assay
British Journal of Cancer (2013)