Abstract
Background:
The possible presence of early tumour dissemination is the rationale behind the use of systemic adjuvant chemotherapy in patients with operable breast cancer. Circulating tumour cells (CTC) in peripheral blood may represent the possible presence of early tumour dissemination. However, relatively few studies were designed to investigate the relationship between the change of CTC status and the efficacy of adjuvant chemotherapy in operable breast cancer patients.
Methods:
In a prospective study, we established a multimarker real-time quantitative PCR platform to detect CTC in peripheral blood of breast cancer patients. By using this platform, we detected CTC in peripheral blood of 94 operable breast cancer patients. Control group consisted of 20 patients with benign breast disease and 20 healthy volunteers. For 72 patients who underwent systemic adjuvant chemotherapy, the dynamic CTC status at three different time points (1 day before initiation of chemotherapy, 1 week after three cycles of chemotherapy and 1 week after all cycles of chemotherapy) was observed.
Results:
Circulating tumour cells were detected in 56% (53 out of 94) of patients with operable breast cancer. The specificity was 95%. Seventy-two patients who received systemic adjuvant chemotherapy were followed up. After three cycles of chemotherapy, 47% (18 out of 38) of patients who were CTC-positive before chemotherapy changed into negative status. In addition, another 5% (2 out of 38) of patients had changed into negative status after all cycles of chemotherapy.
Conclusion:
Systemic adjuvant chemotherapy had a significant impact on CTC status, and this effect could be observed after three cycles of chemotherapy. Circulating tumour cells detection had the potential to be used to evaluate the efficacy of systemic adjuvant chemotherapy immediately after the chemotherapy was finished in operable breast cancer patients.
Similar content being viewed by others
Main
Metastasis is the main cause of death in breast cancer patients. Either by haematal routes or by lymphangial routes, breast cancer cells can invade into circulation system and finally cause distant metastasis. Breast cancer cells can be detected in peripheral blood, which are known as circulating tumour cells (CTC). Many studies have confirmed that CTC can be detected in the early stage of breast cancer (Pierga et al, 2004; Ring et al, 2004; Benoy et al, 2006; Pierga et al, 2007), and the presence of CTC is associated with haematogenous dissemination and bad prognosis (Wulfing et al, 2006; Xenidis et al, 2006; Molloy et al, 2011).
In clinical practice, the possible presence of hematogenous dissemination is the rationale behind the use of adjuvant chemotherapy in operable breast cancer patients (Schabel, 1977; Pantel and Brakenhoff, 2004). Indeed, the efficacy of adjuvant chemotherapy can be assessed currently only retrospectively in clinical trials, following an observation period of at least 5 years. Consequently, the introduction of new therapies in the clinic takes a long time. Especially, it is not possible to tailor therapy to an individual patient. By contrast, CTC can be detected dynamically by sequential sampling of peripheral blood; hopefully, it can be used to evaluate the efficacy of adjuvant chemotherapy immediately after chemotherapy is finished. However, owing to the heterogeneity of breast cancer cells and instability of gene expression, no single marker can represent all kinds of breast cancer cells (Perou et al, 2000), so multimarker assays with both high sensitivity and specificity are required. On the other hand, there are very few CTC present in the blood of operable breast cancer patients, compared with metastatic patients. In this respect, it has been difficult to show a prognostic value of CTC analyses (Benoy et al, 2006; Pierga et al, 2007). Therefore, relatively few studies were designed to investigate the relationship between the change of CTC status and the efficacy of chemotherapy in operable breast cancer patients.
In the present study, by combining three widely used mRNA markers, including cytokeratin 19 (CK19), human mammaglobin (hMAM) and small breast epithelial mucin (SBEM) (Miksicek et al, 2002; Benoy et al, 2004; Roncella et al, 2008; Daskalaki et al, 2009; Tjensvoll et al, 2009; Valladares-Ayerbes et al, 2009; Van der Auwera et al, 2010; Molloy et al, 2011), we established a multimarker real-time quantitative PCR (QPCR) platform to detect CTC in peripheral blood of breast cancer patients. Then, we sequentially observed the dynamic CTC status in peripheral blood of operable breast cancer patients who underwent systemic adjuvant chemotherapy at three different time points (1 day before initiating of chemotherapy, 1 week after three cycles of chemotherapy and 1 week after all cycles of chemotherapy), and tried to figure out whether CTC detection had the potential to be used to evaluate the efficacy of adjuvant chemotherapy immediately after chemotherapy was finished in operable breast cancer patients.
Materials and methods
Breast cancer cell line
MCF-7 cells were maintained in RPMI 1640 (GIBCO, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS, GIBCO) and 1% penicilin-streptomycin solution (GIBCO). Cells were grown at 37 °C in a 5% CO2 atmosphere incubator.
Patient selection
Ninety-four patients with operable breast cancer (aged 28–85 years) treated at the Department of Breast Surgery of Jiangsu Province Hospital between 2010 and 2011 were recruited in this study consecutively and were sampled for the first time before surgery. For every patient enroled, a complete diagnostic evaluation was done consisting of chest X-rays, mammography, liver ultrasonography and whole-body bone scan to exclude distant metastasis. For 72 patients who underwent systemic adjuvant chemotherapy (according to NCCN 2010 guidelines of breast cancer), peripheral blood samples were additionally obtained at three different time points (1 day before initiation of chemotherapy, 1 week after three cycles of chemotherapy, 1 week after all cycles of chemotherapy).
In order to define baseline expression in peripheral blood of the multiple mRNA markers used in this study, peripheral blood from control subjects was collected. Twenty healthy volunteers (aged 26–72 years) and 20 patients with benign breast disease (aged 28–65 years) treated at the Department of Breast Surgery of Jiangsu Province Hospital between 2010 and 2011 were enroled as control subjects. None of the control subjects had a history or clinical evidence of malignancy.
All of the patients and donors gave their informed consent, and the study has been approved by the Ethical and Scientific Committee of our Institution.
Blood processing
To reduce blood contamination by epithelial cells from the skin, the first 2 ml of blood was discarded and the collection tube was disconnected before withdrawing the needle at the end of the procedure. Peripheral blood (10 ml in EDTA) was collected and then shipped at room temperature within 2 h to the molecular diagnostic laboratory for immediate processing by Ficoll density gradient centrifugation (Ficoll-Paque Plus; TBDscience, Tianjin, China), and cell pellets were kept at −80 °C until RNA extraction.
RNA extraction and cDNA synthesis
Total RNA was isolated from blood samples and cell line using TRIzol Reagent (TaKaRa, Dalian, China) according to the manufacturer’s protocol. Quantification and purity assessment were performed by optical density measurement at 260 and 280 nm. The RNA quality was also checked by 1.5% non-denaturing agarose gel electrophoresis. RNA integrity was tested by real-time QPCR amplification of the β-actin housekeeping gene. RNA samples from the human breast cancer cell line MCF-7 served as a positive control.
Reverse transcription of RNA was carried out with the PrimeScript RT Master Mix system (TaKaRa). Complimentary DNA was synthesised from 2 μg of total RNA isolated from peripheral blood mononuclear cells of healthy volunteers, breast benign disease patients and breast cancer patients in a total volume of 40 μl, according to the manufacturer’s instructions.
Primers
The primers of CK19, SBEM and the ‘housekeeping gene’ β-actin were designed by the Primer5 software (PREMIER, Palo Alto, CA, USA), and hMAM primer was derived from a previously published article (Benoy et al, 2004). All primers were designed to be intron-spanning to preclude amplification of genomic DNA. All primers were synthesised by Invitrogen (Shanghai, China). The forward and reverse primers are listed in Table 1. Serially diluted cDNA synthesised from RNA of human breast cancer cell line MCF-7 was used to generate standard curves of control and marker genes. The efficiency of the primers β-actin, CK19, hMAM and SBEM was 1.00, 0.97, 0.98 and 0.96, respectively.
Multimarker real-time QPCR
Real-time QPCR for the ‘housekeeping gene’ β-actin and marker genes (CK19, hMAM and SBEM) was performed for every cDNA sample either from control subjects or from breast cancer patients. All PCR reactions were performed on the Eppendorf realplex (Eppendorf, Hamburg, Germany) using the fluorescent SYBR Green I methodology. The PCR cycle at which the fluorescence arises above the background signal is called the cycle threshold (Ct).
Real-time QPCR was performed with SYBR Premix Ex Taq (TaKaRa) according to the manufacturer’s instructions in a final volume of 20 μl containing 10 μl of 2 × SYBR Premix Ex Taq, 0.4 μl of 10 μ m PCR forward primer, 0.4 μl of 10 μ m PCR reverse primer, 0.4 μl of 50 × ROX reference dye, 2 μl of cDNA template and 6.8 μl of dH2O. The thermal cycling conditions comprised 10 min at 95 °C and 40 cycles of 10 s denaturation at 95 °C, 15 s annealing at 55 °C and 45 s extension at 72 °C.
The CK19, hMAM and SBEM mRNA quantities were analysed in triplicate, normalised against β-actin as a control gene. As described by Livak and Schmittgen (2001), results are expressed as relative gene expression (RGE) using the 2−ΔΔCt method. Relative gene expression value ‘1’ of the multiple mRNA markers (CK19, hMAM and SBEM) was derived from the mRNA expression in peripheral blood of a healthy volunteer.
Real-time QPCR positivity was defined as gene expression beyond the cut-off threshold, which was set for each gene marker at three s.d. from the mean expression in healthy control blood samples (Mikhitarian et al, 2008). Positivity shown for the multimarker method is defined as positivity for at least one of the markers.
Statistical analysis
All data were analysed by the Statistical Package for the Social Science version 12.0 (SPSS, Chicago, IL, USA). The Pearson’s χ2 test or, in the case of low frequencies per cell, the Fisher’s exact method was used to assess the relationship between rates of positive samples and patient characteristics. The Wilcoxon test for paired non -normally distributed groups was used to compare the dynamic change of CTC status before and after systemic adjuvant chemotherapy. Two-sided P values<0.05 were considered statistically significant.
Results
Study inclusion and patient characteristics
A total of 94 patients with operable breast cancer were included and peripheral blood was obtained for the first time before surgery. Seventy-two patients who underwent systemic adjuvant chemotherapy were additionally sampled 1 day before the initiation of chemotherapy, 1 week after three cycles of chemotherapy and 1 week after all cycles of chemotherapy. The median age was 54.5 years (range: 28–85 years), 79% (74 out of 94) of patients were of >45 years, 60% (56 out of 94) of patients were of postmenopausal status, 28% (26 out of 94) of patients had stage III disease at diagnosis, 70% (66 out of 94) of patients had tumours >2 cm, 48% (45 out of 94) of patients had infiltrated axillary lymph nodes, 29% (27 out of 94) of patients had tumours with histological grade 3, 30% (28 out of 94) of patients had tumours that were ER- and PR-negative and 27% (25 out of 94) of patients had tumours that were HER2-positive (Table 2). Totally, 77% (72 out of 94) of patients underwent systemic adjuvant chemotherapy.
RGE of multiple markers in normal control peripheral blood samples
In this study, baseline gene expression was precisely quantitated in 40 normal peripheral blood samples by real-time QPCR (Table 3). The median RGE value of CK19, hMAM and SBEM in normal control peripheral blood cells was 0.88, 1.38 and 1.04, respectively. To get maximum specificity, a cut-off value for marker positivity, that is, abnormal expression was set at three s.d. from the mean 2−ΔΔCt value for each gene. The cut-off RGE value set up for CK19, hMAM and SBEM was 3.77, 6.62 and 3.27, respectively.
A multimarker real-time QPCR analysis of CTC in patients with operable breast cancer
The median RGE value of CK19, hMAM and SBEM in the peripheral blood of patients with operable breast cancer was 2.51, 3.34 and 1.41, respectively. It was found that 49% (46 out of 94) of patients were positive for CK19, 34% (32 out of 94) of patients were positive for hMAM and 13% (12 out of 94) of patients were positive for SBEM (Table 3). Totally, 56% (53/94) of patients were positive for at least one marker. The sensitivity of the individual marker CK19, hMAM and SBEM was 49%, 34% and 13%, respectively, and the specificity was 97.5%, 97.5% and 100%, respectively. By using the multimarker method, the sensitivity was 56% and the specificity was 95% (Table 4). Neither distribution of patients nor primary tumour tissue characteristics was significantly different between the CTC-positive and CTC-negative patients (P>0.05) (Table 2).
The dynamic change of CTC status before and after chemotherapy
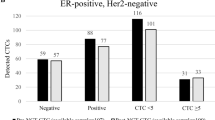
Among 72 patients who underwent systemic adjuvant chemotherapy, 53% (38 out of 72) of patients were CTC-positive and 47% (34 out of 72) of patients were CTC-negative before initiation of chemotherapy. Patients who were CTC-negative before chemotherapy continued to be negative after chemotherapy. Among 38 patients with positive status before chemotherapy, 18 patients changed into negative status after three cycles of chemotherapy and another two patients changed into negative status after all cycles of chemotherapy. In total, 53% (20 out of 38) of patients with positive status before chemotherapy changed into negative status after chemotherapy (Figure 1, Table 5). Circulating tumour cells’ status had a significant change before and after chemotherapy, and systemic adjuvant chemotherapy had a significant impact on CTC status in patients with operable breast cancer (P<0.01).
The dynamic change of CTC status at three different time points during following-up time. A total of 38 patients were CTC-positive and 34 patients were CTC-negative before chemotherapy. In all, 20 patients were CTC-positive and 52 patients were CTC-negative after three cycles of chemotherapy. There was a statistical significant difference between time points before chemotherapy and after three cycles of chemotherapy (P<0.001). After all cycles of chemotherapy, the number of positive patients was 18 and the number of negative patients was 54. There was no statistical significant difference between time points after three cycles and after all cycles (P=0.7).
Discussion
There are three widely used methods for CTC detection: the CellSearch System (Veridex LLC, Raritan, NJ, USA), the AdnaTest Breast Cancer Select/Detect (AdnaGen AG, Langenhagen, Germany) and multimarker real-time QPCR assays. In a study by Van der Auwera et al (2010), the sensitivity of the multimarker (CK19 and hMAM) real-time QPCR assay significantly exceeded that of the CellSearch System (Veridex LLC) and the AdnaTest. In the present study, three widely used markers, including CK19, hMAM and SBEM, were tested by real-time QPCR in the peripheral blood of breast cancer patients. Results showed that CK19-, hMAM- and SBEM-mRNA were positive in 49% (46 out of 94), 34% (32 out of 94) and 13% (12 out of 94) of the operable breast cancer patients, respectively (Table 4). However, when using the multimarker assay (positivity is defined as positivity for at least one of the markers), the sensitivity was improved to 56% (53 out of 94), which was higher than other similar studies (Pierga et al, 2008; Daskalaki et al, 2009; Xenidis et al, 2009; Chen et al, 2010; Krishnamurthy et al, 2010); meanwhile the specificity was 95% (38 out of 40). It shows the multimarker real-time QPCR assay we used has both high sensitivity and specificity for CTC detection. However, because of lack of prognostic data, our results should be adopted cautiously.
Established clinical prognostic markers (that is, axillary lymph node metastasis, negative ER/PR status and positive HER2 status) cannot precisely predict the relapse for individual patient, but CTC are supposed to represent occult burden of systemic disease and hopefully become another predictive marker for early-stage breast cancer patients. In this study, we explored the correlation between detection of multimarker-positive CTC and clinicopathological characteristics of patients with operable breast cancer. We found that there was no significant association between detection of multimarker-positive CTC and any established clinical prognostic markers, which was consistent with other research (Xenidis et al, 2006; Apostolaki et al, 2007; Mikhitarian et al, 2008; Chen et al, 2010; Molloy et al, 2011). Therefore, we hypothesised that the occurrence of CTC may be independent with established prognostic markers and CTC may be another independent prognostic factor for breast cancer.
We monitored the dynamic change (before and after systemic adjuvant chemotherapy) of CTC status in peripherial blood of operable breast cancer patients. Results showed that after three cycles of chemotherapy, 47% (18 out of 38) of patients who were CTC-positive before chemotherapy changed into negative status. And after all cycles of chemotherapy were finished, another two patients changed into negative status, which means 53% (20 out of 38) of patients who were CTC-positive before chemotherapy changed into negative status. It indicates that systemic adjuvant chemotherapy could kill CTC in some patients, and this effect could be observed after three cycles of chemotherapy. Notably, 47% (18 out of 38) of patients remained CTC-positive after chemotherapy, which suggests that the chemotherapy regimen offered may be less effective or inactive for some patients. For the former patients, effective chemotherapy regimen may be needed whereas for the latter ones, the failure of adjuvant chemotherapy may be due to insensitivity of chemotherapeutic drugs offered or the presence of dormant cancer stem cells, which were insensitive to adjuvant chemotherapy (Abraham et al. 2005; Balic et al, 2006). For these patients, therefore, new therapies may be needed, as either changing chemotherapeutic drugs or using other therapies.
In conclusion, we have established a sensitive and specific platform to detect CTC in peripheral blood of breast cancer patients. We found that systemic adjuvant chemotherapy had a significant impact on CTC status, and this effect could be observed after three cycles of chemotherapy. Therefore, CTC detection had the potential to be used to evaluate the efficacy of adjuvant chemotherapy immediately after chemotherapy was finished in operable breast cancer patients. However, owing to the short follow-up time, our results should be interpreted with caution until verified from a long-term follow-up aimed to prognosis.
Change history
23 January 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abraham BK, Fritz P, McClellan M, Hauptvogel P, Athelogou M, Brauch H (2005) Prevalence of CD44+/CD24-/low cells in breast cancer may not be associated with clinical outcome but may favor distant metastasis. Clin Cancer Res 11 (3): 1154–1159
Apostolaki S, Perraki M, Pallis A, Bozionelou V, Agelaki S, Kanellou P, Kotsakis A, Politaki E, Kalbakis K, Kalykaki A, Vamvakas L, Georgoulias V, Mavroudis D (2007) Circulating HER2 mRNA-positive cells in the peripheral blood of patients with stage I and II breast cancer after the administration of adjuvant chemotherapy: evaluation of their clinical relevance. Ann Oncol 18 (5): 851–858
Balic M, Lin H, Young L, Hawes D, Giuliano A, McNamara G, Datar RH, Cote RJ (2006) Most early disseminated cancer cells detected in bone marrow of breast cancer patients have a putative breast cancer stem cell phenotype. Clin Cancer Res 12 (19): 5615–5621
Benoy IH, Elst H, Philips M, Wuyts H, Van Dam P, Scharpe S, Van Marck E, Vermeulen PB, Dirix LY (2006) Real-time RT-PCR detection of disseminated tumour cells in bone marrow has superior prognostic significance in comparison with circulating tumour cells in patients with breast cancer. Br J Cancer 94 (5): 672–680
Benoy IH, Elst H, Van der Auwera I, Van Laere S, van Dam P, Van Marck E, Scharpe S, Vermeulen PB, Dirix LY (2004) Real-time RT-PCR correlates with immunocytochemistry for the detection of disseminated epithelial cells in bone marrow aspirates of patients with breast cancer. Br J Cancer 91 (10): 1813–1820
Chen Y, Zou TN, Wu ZP, Zhou YC, Gu YL, Liu X, Jin CG, Wang XC (2010) Detection of cytokeratin 19, human mammaglobin, and carcinoembryonic antigen-positive circulating tumor cells by three-marker reverse transcription-PCR assay and its relation to clinical outcome in early breast cancer. Int J Biol Markers 25 (2): 59–68
Daskalaki A, Agelaki S, Perraki M, Apostolaki S, Xenidis N, Stathopoulos E, Kontopodis E, Hatzidaki D, Mavroudis D, Georgoulias V (2009) Detection of cytokeratin-19 mRNA-positive cells in the peripheral blood and bone marrow of patients with operable breast cancer. Br J Cancer 101 (4): 589–597
Krishnamurthy S, Cristofanilli M, Singh B, Reuben J, Gao H, Cohen EN, Andreopoulou E, Hall CS, Lodhi A, Jackson S, Lucci A (2010) Detection of minimal residual disease in blood and bone marrow in early stage breast cancer. Cancer 116 (14): 3330–3337
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25 (4): 402–408
Mikhitarian K, Martin RH, Ruppel MB, Gillanders WE, Hoda R, Schutte del H, Callahan K, Mitas M, Cole DJ (2008) Detection of mammaglobin mRNA in peripheral blood is associated with high grade breast cancer: interim results of a prospective cohort study. BMC Cancer 8: 55
Miksicek RJ, Myal Y, Watson PH, Walker C, Murphy LC, Leygue E (2002) Identification of a novel breast- and salivary gland-specific, mucin-like gene strongly expressed in normal and tumor human mammary epithelium. Cancer Res 62 (10): 2736–2740
Molloy TJ, Devriese LA, Helgason HH, Bosma AJ, Hauptmann M, Voest EE, Schellens JH, van't Veer LJ (2011) A multimarker QPCR-based platform for the detection of circulating tumour cells in patients with early-stage breast cancer. Br J Cancer 104 (12): 1913–1919
Pierga JY, Bidard FC, Denis MG, de Cremoux P (2007) Prognostic value of peripheral blood double detection of CK19 and MUC1 mRNA positive cells detected by RT-quantitative PCR in 94 breast cancer patients with a follow up of 9 years. Mol Oncol 1 (3): 267–268
Pierga JY, Bonneton C, Vincent-Salomon A, de Cremoux P, Nos C, Blin N, Pouillart P, Thiery JP, Magdelenat H (2004) Clinical significance of immunocytochemical detection of tumor cells using digital microscopy in peripheral blood and bone marrow of breast cancer patients. Clin Cancer Res 10 (4): 1392–1400
Pantel K, Brakenhoff RH (2004) Dissecting the metastatic cascade. Nat Rev Cancer 4 (6): 448–456
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D (2000) Molecular portraits of human breast tumours. Nature 406 (6797): 747–752
Pierga JY, Bidard FC, Mathiot C, Brain E, Delaloge S, Giachetti S, de Cremoux P, Salmon R, Vincent-Salomon A, Marty M (2008) Circulating tumor cell detection predicts early metastatic relapse after neoadjuvant chemotherapy in large operable and locally advanced breast cancer in a phase II randomized trial. Clin Cancer Res 14 (21): 7004–7010
Ring A, Smith IE, Dowsett M (2004) Circulating tumour cells in breast cancer. Lancet Oncol 5 (2): 79–88
Roncella S, Ferro P, Bacigalupo B, Dessanti P, Pronzato P, Franceschini MC, Prattico L, Carletti AM, Canessa PA, Fontana V, Fais F, Pistillo MP, Fedeli F (2008) Assessment of RT-PCR detection of human mammaglobin for the diagnosis of breast cancer derived pleural effusions. Diagn Mol Pathol 17 (1): 28–33
Schabel FM (1977) Rationale for adjuvant chemotherapy. Cancer 39 (6 Suppl): 2875–2882
Tjensvoll K, Gilje B, Oltedal S, Shammas VF, Kvaloy JT, Heikkila R, Nordgard O (2009) A small subgroup of operable breast cancer patients with poor prognosis identified by quantitative real-time RT-PCR detection of mammaglobin A and trefoil factor 1 mRNA expression in bone marrow. Breast Cancer Res Treat 116 (2): 329–338
Valladares-Ayerbes M, Iglesias-Diaz P, Diaz-Prado S, Ayude D, Medina V, Haz M, Reboredo M, Antolin S, Calvo L, Anton-Aparicio LM (2009) Diagnostic accuracy of small breast epithelial mucin mRNA as a marker for bone marrow micrometastasis in breast cancer: a pilot study. J Cancer Res Clin Oncol 135 (9): 1185–1195
Van der Auwera I, Peeters D, Benoy IH, Elst HJ, Van Laere SJ, Prove A, Maes H, Huget P, van Dam P, Vermeulen PB, Dirix LY (2010) Circulating tumour cell detection: a direct comparison between the CellSearch System, the AdnaTest and CK-19/mammaglobin RT-PCR in patients with metastatic breast cancer. Br J Cancer 102 (2): 276–284
Wulfing P, Borchard J, Buerger H, Heidl S, Zanker KS, Kiesel L, Brandt B (2006) HER2-positive circulating tumor cells indicate poor clinical outcome in stage I to III breast cancer patients. Clin Cancer Res 12 (6): 1715–1720
Xenidis N, Ignatiadis M, Apostolaki S, Perraki M, Kalbakis K, Agelaki S, Stathopoulos EN, Chlouverakis G, Lianidou E, Kakolyris S, Georgoulias V, Mavroudis D (2009) Cytokeratin-19 mRNA-positive circulating tumor cells after adjuvant chemotherapy in patients with early breast cancer. J Clin Oncol 27 (13): 2177–2184
Xenidis N, Perraki M, Kafousi M, Apostolaki S, Bolonaki I, Stathopoulou A, Kalbakis K, Androulakis N, Kouroussis C, Pallis T, Christophylakis C, Argyraki K, Lianidou ES, Stathopoulos S, Georgoulias V, Mavroudis D (2006) Predictive and prognostic value of peripheral blood cytokeratin-19 mRNA-positive cells detected by real-time polymerase chain reaction in node-negative breast cancer patients. J Clin Oncol 24 (23): 3756–3762
Acknowledgements
This work was supported in part by Wu Jie-Ping Foundation (320.670010009), the National Natural Science Foundation of China (81071753), the Six Kinds of Outstanding Talent Foundation of Jiangsu Province (2010-ws-079 to Wei He and 2009 to Qiang Ding), the Science and Education for Health Foundation of Jiangsu Province (RC2007054), the Natural Science Foundation of Jiangsu Province (BK2008476, BK2009438 and BK2010581), the Program for Development of Innovative Research Team in the First Affiliated Hospital of NJMU (IRT-008) and a project Funded by the Priority Academic Program Development of Jiangsu higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Chong, Mh., Zhao, Y., Wang, J. et al. The dynamic change of circulating tumour cells in patients with operable breast cancer before and after chemotherapy based on a multimarker QPCR platform. Br J Cancer 106, 1605–1610 (2012). https://doi.org/10.1038/bjc.2012.157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.157
Keywords
This article is cited by
-
Heterogeneous circulating tumor cells correlate with responses to neoadjuvant chemotherapy and prognosis in patients with locally advanced breast cancer
Breast Cancer Research and Treatment (2023)