Abstract
Background:
Bevacizumab is commonly used in combination with chemotherapy in the treatment of metastatic colorectal cancer, but to date, despite extensive research, no predictive or prognostic biomarkers for bevacizumab have been identified. The development of bevacizumab-induced arterial hypertension has recently been suggested as a potential predictive biomarker.
Methods:
Blood pressure was recorded during the BOXER study, a phase II study of capecitabine, oxaliplatin (CAPOX) plus bevacizumab as peri-operative treatment in 45 patients with poor-risk colorectal liver-only metastases unsuitable for upfront resection. In this analysis, the development of bevacizumab-induced hypertension was correlated with clinical outcomes.
Results:
Fifteen percent of patients developed ⩾grade 1 hypertension while receiving neoadjuvant chemotherapy, and 4% developed grade 3 hypertension. There was no correlation between the development of hypertension and radiological response rate (P=0.642), progression-free survival (P=0.644) or overall survival (P=0.480) in those who developed hypertension compared with those who did not.
Conclusion:
Bevacizumab-induced hypertension did not predict radiological response or survival in our study. The results highlight a number of important issues regarding the use of hypertension as a biomarker.
Similar content being viewed by others
Main
Angiogenesis is the process of new blood vessel formation and is critical for tumour cell survival, growth, invasion and metastases. To date, bevacizumab, a humanised monoclonal antibody to VEGF-A, has been one of the most successful anti-angiogenic agents in the treatment of metastatic colorectal cancer (mCRC). The addition of bevacizumab to combination chemotherapy has demonstrated prolonged progression-free survival (PFS) and overall survival (OS) in the first- and second-line setting (Hurwitz et al, 2004; Kabbinavar et al, 2005; Saltz et al, 2008). With the introduction of targeted agents, the relevance of prognostic and predictive markers in patient selection has become increasingly relevant. However, despite extensive research, the mechanisms responsible for the antitumour activity of antiangiogenic agents is not fully understood, and although many potential biomarkers have been proposed and investigated none have yet been validated for clinical use.
Hypertension is one of the most common side effects of bevacizumab; in the pivotal Hurwitz study, all-grade hypertension was demonstrated in 22.4% of those treated with irinotecan, fluorouracil and leucovorin (IFL) plus bevacizumab compared with 8.3% who received IFL alone (Hurwitz et al, 2004). This has been consistently demonstrated in phase II/III clinical trials of bevacizumab in the treatment of colorectal cancer (Table 1). A recent meta-analysis demonstrated that the relative risk of colorectal cancer patients developing grade 3/4 hypertension when treated with bevacizumab was 4.87, P=0.0001 (Loupakis et al, 2010).
A number of retrospective studies have suggested that the development of bevacizumab-induced arterial hypertension may correlate with clinical outcome in colorectal cancer patients (Table 2). These results are in contrast to a meta-analysis of six large randomised controlled trials of bevacizumab in combination with chemotherapy across a number of tumour types. Of the two colorectal studies included in the meta-analysis, only the AVF2107g trial of IFL, with or without bevacizumab, demonstrated that the development of hypertension predicted for PFS and OS (Hurwitz et al, 2004).
We previously conducted a multicentre phase II study of capecitabine, oxaliplatin (CAPOX) plus bevacizumab as peri-operative treatment in 45 patients with poor-risk colorectal liver-only metastases unsuitable for upfront resection (BOXER study) (Wong et al, 2011). The overall response rate was 78% (95% CI: 63–89%), which allowed 12/30 (40%) patients with initial non-synchronous unresectable CLM to be converted to resectable. In addition, 10/15 (67%) patients with synchronous resectable CLM underwent liver resection, with four patients being observed to have excellent response to treatment. In light of the emerging data suggesting hypertension as a potential biomarker, we analysed the patients treated within the BOXER trial to assess whether the development of hypertension was associated with outcome in this prospective multicentre phase II study.
Materials and methods
To be eligible for the study, patients had to have a recorded blood pressure of <145/90 mm Hg−1 before commencing treatment and no evidence of proteinuria at baseline as defined by >1 g of protein per 24 h by a 24-hour urine collection. Blood pressure measurements were taken after the patient had been in a resting position for ∼5 min and performed before each cycle; repeated measurement of blood pressure for verification was undertaken if the initial reading was 140 mm Hg systolic and/or 90 mm Hg diastolic. Worse-grade toxicity was assessed using common toxicity criteria adverse event (NCI-CTCAE) v3.0, and malignant hypertension was classified as a targeted adverse event. Patients received oxaliplatin (130 mg m−2) and bevacizumab (7.5 mg kg−1) intravenously on day 1 every 3 weeks. Capecitabine was given orally at a dose of 1700, mg m−2 per day in two split doses for 14 days repeated every 3 weeks. No dose reductions of bevacizumab were made, and toxicity attributable to bevacizumab required bevacizumab treatment to be withheld. Any missed doses of bevacizumab were not made up. Treatment response and operability was reassessed after every 12 weeks of treatment, and those whose liver metastases became operable proceeded to metastatectomy. After recovery from surgery, patients received another 12 weeks of CAPOX plus bevacizumab at the same dose schedule as preoperative block.
Hypertension was prospectively recorded using CTCAE v3.0; for the purpose of analysis hypertension was defined as grade ⩾1 hypertension (asymptomatic, transient (<24 h) increase by 20 mm Hg or to >150/100 if previously normal: intervention not indicated). Fisher’s exact test was used to analyse the association between the development of hypertension and radiological response. The Kaplan–Meier method was used to estimate OS and PFS, and groups were compared using the log-rank test; separate analyses were performed for each grade of hypertension (grade 1–3).
Results
The median number of bevacizumab-containing cycles was eight. For those patients proceeding to liver resection, the median number of preoperative cycles of CAPOX plus bevacizumab was four. Overall, the treatment was well tolerated and grade 3/4 toxicity was low. Fifteen percent of patients developed ⩾grade 1 hypertension while receiving neoadjuvant chemotherapy. Only 4% developed grade 3 hypertension. In four cases, the hypertension was recorded on a single occasion, and in the remaining cases it occurred more than once (range 1–6). The onset of hypertension was early (cycle 1–3) in 75% of cases. Three patients required antihypertensive therapy during their chemotherapy. Of those who developed hypertension, three had a past medical history of controlled hypertension and were on at least one antihypertensive at trial entry (range 1–3).
There was no difference in radiological response between those who developed hypertension and those who did not (71% vs 78% P=0.642). No statistical comparison was possible between the grade of hypertension and outcome or individual responses (CR, PR, SD, PD) because of the small numbers.
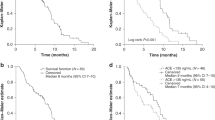
Progression-free survival at 12 months was 49% in the non-hypertension group vs 57% in the hypertension group (P=0.664) (Figure 1). In addition, there was no difference in PFS according to the grade of hypertension (P=0.886).
Overall survival at 12 months was 67% in the hypertension group and 91% in the non-hypertensive group (P=0.826) (Figure 2). There was no difference in OS according to grade of hypertension (P=0.480).
Discussion
Our results demonstrate that hypertension is a common side effect of bevacizumab, occurring in 15% of patients; however, in contrast to recent data, the development of hypertension was not predictive of outcome in this study. Our study is limited by the small patient numbers, and our conflicting results may be related to the high overall response rate or simply the low incidence of hypertension in this study. The overall rate of hypertension in this study was lower than the previously published rates, potentially a consequence of the highly selected patient population. Our findings highlight the complexities of the use of hypertension as a potential biomarker, in particular the presence of coexistent hypertension, complicating interpretation of retrospective analyses.
The data suggesting an association between the development of hypertension and outcome have been mostly, similar to ours, retrospective analyses of blood pressure, with considerable variation in the method of recording and definition of hypertension. It is well documented that blood pressure is affected by multiple factors, which can be patient or operator related, and even small changes in blood pressure cuff position or bladder volume at the time of recording can affect readings. The CTCAE grading for hypertension is also relatively subjective, which may contribute to the lack of reproducibility demonstrated in these studies. Alternatively, more accurate methods of blood pressure monitoring include ambulatory blood pressure measurement; however, the feasibility of ambulatory monitoring is limited in daily clinical practice.
It remains unclear whether baseline blood pressure, the rate of rise, the absolute rise, the timing of onset or the duration of hypertension are all equally relevant factors. In particular, the clinically important cutoff values for percentage rise in blood pressure have yet to be established. In one study, a predictive effect was demonstrated in patients with grade ⩾2–4 hypertension (De Stefano et al, 2011), and in another the benefit was seen with any grade of hypertension (Osterlund et al, 2011). Certainly, the most common rise in blood pressure does not appear to be very high (10–20 mm Hg systolic), and the incidence of hypertensive crisis in most studies is low (0.1%). In addition, the median time to onset of hypertension is not well documented.
Before the emergence of evidence demonstrating KRAS mutation as a predictive biomarker for the lack of response to anti-EGFR antibodies, the severity of skin rash developed by patients was the only consistent biomarker for response. The EVEREST study demonstrated that dose escalation of cetuximab in patients who did not initially develop an intense rash resulted in a higher incidence of grade 3 skin reactions, which correlated with an increase in response rates (Van Cutsem et al, 2007). On a similar basis, the prevalence of hypertension with anti-angiogenics led to the suggestion that dose titration of bevacizumab until blood pressure elevation may lead to better anti-tumour efficacy and improved outcomes (Maitland and Ratain, 2006). Although the incidence of hypertension does appear to increase with higher doses of bevacizumab (Kabbinavar et al, 2003), there is currently no evidence to suggest that this results in improved outcomes.
Patients receiving anti-angiogenic agents should have their blood pressure monitored throughout the treatment, with more frequent assessments during the first cycle of treatment. Trial guidelines and bevacizumab prescribing information routinely recommend treating bevacizumab-induced hypertension with an ACE inhibitor or calcium channel blocker and continuing treatment rather than reducing the dose of the bevacizumab, so as not to deny patients potential benefit. Little is known about the effect of treating bevcizumab-induced hypertension and whether this could potentially negate the benefit of bevacizumab.
Certainly, we remain in need of a biomarker for bevacizumab; nevertheless, despite recent data we are left with a number of unanswered questions regarding the role of hypertension as a biomarker. In particular, how do we, and more importantly should we, prospectively validate an adverse event as a biomarker? The clinical impact of severe hypertension is not insignificant, and is associated with the risk of cardiovascular complications and arterial thromboembolic events (Ranpura et al, 2010, 2011). With a median survival of patients with mCRC up to 24 months, it is becoming increasingly relevant to focus on potential long-term side effects in this group of patients.
Factors that predict bevacizumab-induced hypertension could assist in the prospective selection of patients for treatment; in a breast cancer study, VEGF genotype predicted clinically significant hypertension and those with VEGF-1498TT and VEGF-634 CC were largely protected from serious hypertension (Schneider et al, 2008). However, these studies have yet to be replicated in colorectal cancer.
There is no doubt that the identification of hypertension as a potential biomarker has increased our understanding of the mechanism of action of anti-angiogenic agents, yet how we implement this knowledge remains uncertain. A number of prospective studies currently evaluating factors such as flow-mediated vasodilation, nitric oxide activity and vascular dysfunction are ongoing; however, given the complexities associated with the use of an adverse event as a biomarker, significant research is still needed to identify alternative biomarkers for bevacizumab.
Change history
23 January 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Allegra CJ, Yothers G, O'Connell MJ, Sharif S, Colangelo LH, Lopa SH, Petrelli NJ, Goldberg RM, Atkins JN, Seay TE, Fehrenbacher L, O'Reilly S, Chu L, Azar CA, Wolmark N (2009) Initial safety report of NSABP C-08: A randomized phase III study of modified FOLFOX6 with or without bevacizumab for the adjuvant treatment of patients with stage II or III colon cancer. J Clin Oncol 27 (20): 3385–3390
De Stefano A, Carlomagno C, Pepe S, Bianco R, De Placido S (2011) Bevacizumab-related arterial hypertension as a predictive marker in metastatic colorectal cancer patients. Cancer Chemother Pharmacol 68 (5): 1207–1213
Giantonio BJ, Catalano PJ, Meropol NJ, O'Dwyer PJ, Mitchell EP, Alberts SR, Schwartz MA, Benson AB (2007) Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol 25 (12): 1539–1544
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350 (23): 2335–2342
Kabbinavar F, Hurwitz HI, Fehrenbacher L, Meropol NJ, Novotny WF, Lieberman G, Griffing S, Bergsland E (2003) Phase II, randomized trial comparing bevacizumab plus fluorouracil (FU)/leucovorin (LV) with FU/LV alone in patients with metastatic colorectal cancer. J Clin Oncol 21 (1): 60–65
Kabbinavar FF, Schulz J, McCleod M, Patel T, Hamm JT, Hecht JR, Mass R, Perrou B, Nelson B, Novotny WF (2005) Addition of bevacizumab to bolus fluorouracil and leucovorin in first-line metastatic colorectal cancer: results of a randomized phase II trial. J Clin Oncol 23 (16): 3697–3705
Kozloff M, Yood MU, Berlin J, Flynn PJ, Kabbinavar FF, Purdie DM, Ashby MA, Dong W, Sugrue MM, Grothey A (2009) Clinical outcomes associated with bevacizumab-containing treatment of metastatic colorectal cancer: the BRiTE observational cohort study. Oncologist 14 (9): 862–870
Loupakis F, Bria E, Vaccaro V, Cuppone F, Milella M, Carlini P, Cremolini C, Salvatore L, Falcone A, Muti P, Sperduti I, Giannarelli D, Cognetti F (2010) Magnitude of benefit of the addition of bevacizumab to first-line chemotherapy for metastatic colorectal cancer: meta-analysis of randomized clinical trials. J Exp Clin Cancer Res 29: 58
Maitland ML, Ratain MJ (2006) Terminal ballistics of kinase inhibitors: there are no magic bullets. Ann Intern Med 145 (9): 702–703
Osterlund P, Soveri LM, Isoniemi H, Poussa T, Alanko T, Bono P (2011) Hypertension and overall survival in metastatic colorectal cancer patients treated with bevacizumab-containing chemotherapy. Br J Cancer 104 (4): 599–604
Ranpura V, Hapani S, Chuang J, Wu S (2010) Risk of cardiac ischemia and arterial thromboembolic events with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis of randomized controlled trials. Acta Oncol 49 (3): 287–297
Ranpura V, Hapani S, Wu S (2011) Treatment-related mortality with bevacizumab in cancer patients: a meta-analysis. JAMA 305 (5): 487–494
Saltz LB, Clarke S, Diaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, Couture F, Sirzen F, Cassidy J (2008) Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 26 (12): 2013–2019
Scartozzi M, Galizia E, Chiorrini S, Giampieri R, Berardi R, Pierantoni C, Cascinu S (2009) Arterial hypertension correlates with clinical outcome in colorectal cancer patients treated with first-line bevacizumab. Ann Oncol 20 (2): 227–230
Schneider BP, Wang M, Radovich M, Sledge GW, Badve S, Thor A, Flockhart DA, Hancock B, Davidson N, Gralow J, Dickler M, Perez EA, Cobleigh M, Shenkier T, Edgerton S, Miller KD (2008) Association of vascular endothelial growth factor and vascular endothelial growth factor receptor-2 genetic polymorphisms with outcome in a trial of paclitaxel compared with paclitaxel plus bevacizumab in advanced breast cancer: ECOG 2100. J Clin Oncol 26 (28): 4672–4678
Van Cutsem E, Humblet Y, Gelderblom H, Vermorken JB, Viret F, Glimelius B, Ciardiello F, Gallerani E, Amellal N, Peeters M (2007) Cetuximab dose-escalation study in patients with metastatic colorectal cancer (mCRC) with no or slight skin reactions on cetuximab standard dose treatment (EVEREST): Pharmacokinetic and efficacy data of a randomized study. Gastrointest Cancers Symp (abstract: 237)
Wong NS, Fernando NH, Nixon AB, Cushman S, Aklilu M, Bendell JC, Morse MA, Blobe GC, Ashton J, Pang H, Hurwitz HI (2011) A phase II study of capecitabine, oxaliplatin, bevacizumab and cetuximab in the treatment of metastatic colorectal cancer. Anticancer Res 31 (1): 255–261
Acknowledgements
The authors acknowledge NHS funding from the NIHR Biomedical Research Centre and the Peter Stebbings Memorial Charity. Educational grant and bevacizumab provided by Roche for BOXER study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Dewdney, A., Cunningham, D., Barbachano, Y. et al. Correlation of bevacizumab-induced hypertension and outcome in the BOXER study, a phase II study of capecitabine, oxaliplatin (CAPOX) plus bevacizumab as peri-operative treatment in 45 patients with poor-risk colorectal liver-only metastases unsuitable for upfront resection. Br J Cancer 106, 1718–1721 (2012). https://doi.org/10.1038/bjc.2012.152
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.152
Keywords
This article is cited by
-
Application via mechanical dropper alleviates sufentanil-induced cough: a prospective, randomized, single-blinded trial
Trials (2019)
-
Effects of small-dose remifentanil combined with index of consciousness monitoring on gastroscopic polypectomy: a prospective, randomized, single-blinded trial
Trials (2018)
-
Development of hypertension within 2 weeks of initiation of sorafenib for advanced hepatocellular carcinoma is a predictor of efficacy
International Journal of Clinical Oncology (2015)
-
Targeted therapies in colorectal cancer—an integrative view by PPPM
EPMA Journal (2013)
-
Correlation of bevacizumab-induced hypertension and outcomes of metastatic colorectal cancer patients treated with bevacizumab: a systematic review and meta-analysis
World Journal of Surgical Oncology (2013)