Abstract
Renal impairment (RI) is seen in over a quarter of patients with newly diagnosed multiple myeloma (NDMM). It is not clear if reversal of RI improves the outcome to that expected for NDMM patients without RI. We evaluated 1135 consecutive patients with NDMM seen at the Mayo Clinic between January 2003 and December 2012. RI was defined as having a creatinine clearance (CrCl) <40ml/min. The median overall survival (OS) for patients with RI at diagnosis receiving and not receiving novel agent induction therapy was not reached vs 46 months (P<0.001). The median OS for patients with CrCl ⩾40 ml/min at diagnosis, CrCl <40 ml/min at diagnosis but improved to ⩾40 ml/min and CrCl <40 ml/min at diagnosis and remained <40 ml/min, were 112, 56 and 33 months, respectively (P<0.001). The complete renal response rate for patients with RI at diagnosis receiving novel agent induction therapy compared to the rest was 40 vs 16% (P<0.001). In conclusion, patients with reversal of RI have improved outcomes, but it remains inferior to patients with normal renal function at diagnosis. These results have implications for identifying early treatment strategies for patients at risk of developing renal insufficiency.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is the second most common hematologic malignancy among adults in the United States.1 Renal impairment (RI) is relatively common in patients with newly diagnosed MM (NDMM), ~20–40%,2, 3 and forms one of the defining features for diagnosis of symptomatic disease.4 RI in NDMM patients is often multifactorial and can be secondary to any of the following disease-related factors such as cast nephropathy, hypercalcemia, hyperuricemia, coexistent amyloidosis, light-chain deposition disease and so on.5, 6 RI is associated with a higher rate of treatment-related toxicity, early mortality and reduced overall survival (OS), especially when renal failure is advanced and dialysis support is required.7, 8, 9, 10 The effective management of RI associated with MM requires the prompt institution of anti-myeloma therapy and supportive measures.11
The incorporation of novel therapeutic agents such as immunomodulators (thalidomide, lenalidomide and pomalidomide) and proteasome inhibitors (bortezomib and carfilzomib) as well as improved supportive care options have led to significant improvements in the OS of patients with MM.12, 13, 14, 15, 16 These beneficial effects have also been described in newly diagnosed MM patients with RI.17, 18, 19 Although it has been shown that improvement in renal function can lead to improved survival in patients with MM,19, 20 it is not clear whether complete recovery of renal function improves survival outcomes to that experienced by MM patients who did not have RI at diagnosis. Thus, we addressed this question in a large cohort of patients with NDMM seen over the last decade at a single institution.
Patients and methods
We identified NDMM patients seen at the Mayo Clinic, Rochester between 1 January 2003 and 31 December 2010 within 90 days of their diagnosis. Patients with light-chain amyloidosis with organ involvement confirmed via tissue biopsy were excluded from the current study. Approval for this study was obtained from the Mayo Clinic Institutional Review Board in accordance with the federal regulations and the principles of the Declaration of Helsinki.
Host and disease variables at diagnosis that were examined for prognostic significance included age, bone marrow plasma cell percentage, molecular cytogenetics status by fluorescent in situ hybridization (FISH), stage based on international staging system classification,21 plasma cell labeling index, serum monoclonal protein spike, urine monoclonal protein spike, hemoglobin, serum creatinine and lactate dehydrogenase (LDH). Levels >192 IU/dl for LDH were considered elevated. Patients who had a FISH analysis performed on their plasma cells were categorized as having high-risk disease if any of the following abnormalities: t(4;14), t(14;16) or t(14;20) were present at any time during their disease course, or a deletion 17p within 30 days of the diagnosis or any time before the diagnosis.22, 23 The initial treatment regimen used for induction was recorded and drugs such as thalidomide, lenalidomide and bortezomib were categorized as novel agents.
Serum creatinine at diagnosis and at last follow-up was obtained from clinical records and the creatinine clearance (CrCl) was calculated by the modification of diet in renal disease (MDRD) equation using the simplified four-variable MDRD formula: glomerular filtration rate=186.3 × (serum creatinine)−1.154 x (age in years)−0.203 × 1.212 (if patient is black) x 0.742 (if female).24 RI in NDMM patients was defined as an estimated glomerular filtration rate (eGFR)<40 ml/min/1.73 m2. For the analyses in this study, patients were categorized based on their renal function at diagnosis and response to therapy: group 1: CrCl⩾40 at diagnosis, group 2: CrCl<40 at diagnosis but improved to ⩾40 after therapy and group 3: CrCl<40 at diagnosis and remained <40 after therapy. The degree of restoration of renal function was evaluated according to the International Myeloma Working Group (IMWG) criteria, which considered renal complete response as a sustained increase in baseline eGFR to ⩾60 ml/min.11 Renal partial response was defined as an increase of eGFR from <15–30–59 ml/min and renal minor response as sustained improvement of baseline eGFR of <15 ml/min to 15–29 ml/min or if baseline eGFR was 15–29 ml/min, improvement to 30–59 ml/min. Early mortality was defined as death within 6 months of diagnosis. The primary end point of this study was OS, which was defined as the time from diagnosis to death with patients alive at the time of last follow-up censored at that date. The secondary end points were rate of early mortality and renal response in patients with RI.
The Fisher’s exact test was used to assess for differences in nominal variables. Differences in continuous variables were compared using the Wilcoxon signed-rank test. Cox proportional hazard analysis was used to identify factors that were prognostic for reversal of RI and OS. Survival curves were constructed according to the Kaplan-Meier method and the curves were compared using log-rank test. All analyses were performed using JMP 10.0 (SAS Institute Inc., Cary, NC, USA).
Results
The study included 1135 patients with NDMM seen between 1 January 2003 and 31 December 2010. The characteristics of these patients are described in Table 1. The median age at diagnosis was 65 years (range 22–93); 682 (60%) were male. The median estimated follow-up for the entire group from diagnosis was 76 months (95% confidence interval (CI) 72–79) and 515 (45%) patients had died at the time of this analysis.
Baseline renal function and relationship with clinical features
The median creatinine at diagnosis was 1.1 mg/dl (range 0.4 to 11) with 124 (11%) patients presenting with a creatinine over 2 mg/dL. The median CrCl was 67 ml/min (range 4–219 ml/min) with 690 (61%), 322 (28%) and 123 (11%) of the patients with CrCl⩾Â60 ml/min, 30–59 ml/min and <30 ml/min, respectively. Comparison of baseline patient and disease-related features between patients with RI (CrCl<40 ml/min; N=192, 17%) vs those with CrCl⩾40 ml/min (N=943, 83%) are listed in Table 1. Patients with RI tended to be older (P<0.001), female (P=0.024), were more likely to have light-chain-only disease (P<0.001) and have a higher tumor burden (that is, international staging system 3; P<0.001), plasma cell labeling index (P=0.011), LDH (P<0.001) and bone marrow plasma cell percentage (P<0.001). There were 763 (67%) patients who received one or more of the novel agents as part of their initial therapy, of which 109 (14%) patients had a CrCl<40 ml/min at baseline.
Impact of renal function at diagnosis on survival and early mortality
The median OS of the entire group of patients was 89 months (95% CI 74–112). The median OS from diagnosis for those with a creatinine >2 mg/dl was 42 months (95% CI 29–55) compared with 99 months (95% CI 87 to not reached) for the rest; (P<0.001; Figure 1a). The median OS (95% CI) from diagnosis among patients with CrCl⩾40 ml/min and <40 ml/min were 112 (88 to not reached) and 43 months (33–55), respectively (P<0.001; Figure 1b). Of the 192 patients with CrCl<40 ml/min, 32 (16%) required dialysis at diagnosis. The OS of patients requiring dialysis compared to those with CrCl<40 ml/min not requiring dialysis was 45% vs 31% (P=0.58). The rate of early mortality among patients with CrCl⩾40 ml/min and <40 ml/min were 6 and 16%, respectively (P<0.001).
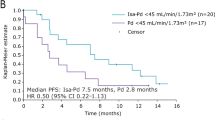
Among the patients with CrCl<40 ml/min at diagnosis, the median OS from diagnosis for those receiving a novel agent was 67 months compared with 24 months for those not receiving a novel agent-based induction (P<0.001; Figure 2). The rate of early mortality among patients with CrCl<40 ml/min at diagnosis receiving a novel agent was 10% compared with 24% for those not receiving a novel agent-based induction regimen (P=0.011).
Improvement in renal function and its relationship with survival and early mortality
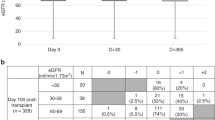
Of the 192 patients with a CrCl<40 ml/min at diagnosis, any improvement in CrCl was seen in 152 (82%) patients. The median time to the best CrCl was 4 months (range <1–34 months) from diagnosis. Only the absence of light-chain MM predicted for recovery of renal function to a CrCl to ⩾40 ml/min in a proportional hazards model (hazard ratio 1.96, 95% CI 1.27–3.14; P=0.002).
Upon applying the IMWG criteria for renal response to the 192 patients with a CrCl<40 ml/min at diagnosis, 56 (29%) had a complete response, 16 (8%) had a partial response, 51 (27%) had a minimal response and 69 (36%) had an not reached. The renal complete response rate for patients with CrCl<40 ml/min at diagnosis receiving novel agent induction therapy compared to those not receiving novel agent induction therapy was 40 vs 16% (P<0.001). The renal complete response rate in patients with CrCl<40 ml/min at diagnosis was higher for those receiving bortezomib-based induction therapies compared to those receiving immunomodulator-based induction therapies, however, this was not statistically significant (45 vs 28%; P=0.09).
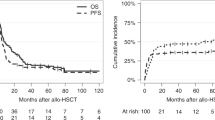
Upon categorizations based on the renal response to therapy as described in the methods, patients in group 2 (N=103, 9%) had a median OS of 56 months compared with 33 months for patients in group 3 (N=89, 8%; P=0.006), but this was still significantly lower than the median OS for patients in group 1 (N=943, 83%), which was 112 months (P<0.001; Figure 3a). A landmark analysis at 6 months, to allow for sufficient duration of therapy, revealed a median OS from diagnosis of not reached, 67 months and 51 months for patients in groups 1, 2 and 3, respectively (P=0.175 between groups 2 and 3; P=0.007 between groups 1 and 2; Figure 3b).
(a) Kaplan-Meier plot comparing overall survival between groups 1, 2, and 3 based on their renal function at diagnosis and response to therapy: group 1, CrCl⩾40 at diagnosis; group 2, CrCl<40 at diagnosis but improved to ⩾40 after therapy; and group 3, CrCl<40 at diagnosis and remained <40 after therapy. (b) Kaplan-Meier plot comparing overall survival at a 6-month landmark based on their renal function at diagnosis and response to therapy: group 1, CrCl⩾40 at diagnosis; group 2, CrCl<40 at diagnosis but improved to ⩾40 after therapy; and group 3, CrCl<40 at diagnosis and remained <40 after therapy.
Improvement in renal function and its relationship with early mortality
An analysis of early mortality (death within 6 months of diagnosis) between the three groups was performed. The rates of early mortality were 6, 9 and 25% for groups 1, 2 and 3, respectively (P=0.003 between groups 2 and 3; P=0.298 between groups 1 and 2). When the analysis was restricted to only patients who received novel agent induction therapy, the rate of early mortality among the NDMM patients with RI was not statistically different between those who received bortezomib-based induction and immunomodulator-based induction with lenalidomide or thalidomide (9 vs 11%, P=0.100). We then examined the last available creatinine in each of the patients. When evaluated over the course of their disease, patients in group 2 were more likely to eventually worsen their renal function again leading to RI toward the end of their follow-up in this study compared to patients in group 1 (34 vs 9%; P<0.001).
Predictors of worse OS at diagnosis
In a univariable analysis assessing predictors for OS, CrCl<40 ml/min, no novel agent induction therapy, age ⩾70, international staging system stage 3, high-risk FISH and LDH>192 IU/dl were all found to predict for worse OS; however, only age ⩾70 (P<0.001), high-risk FISH (P<0.001) and lack of novel agent induction therapy (P=0.008) retained their negative prognostic significance in a multivariable analysis (Table 2). Though plasma cell labeling index was found to be significant in the univariable analysis predicting for OS, it was excluded from the multivariable analysis due to more than half of the patients not having it performed.
Discussion
The current IMWG definition of MM-related RI requires a serum creatinine of 2 g/dl or higher that is unexplainable by any other etiology.25 However, this cutoff may fall short in identifying all NDMM patients with RI since the serum creatinine can be influenced by factors such as muscle mass. Conversely, a cutoff of CrCl <60 ml/min may inappropriately consider older NDMM patients with age-related decline in their CrCl as having MM-related RI. In this study, we used a CrCl cutoff of <40 ml/min as it has appeared to be optimal in identifying NDMM patients with RI when compared to the previously mentioned cutoffs.26
By using our CrCl cutoff of 40 ml/ml, RI at diagnosis was present in almost 20% of the patients. Of these patients, more than half of them (54%) had reversal of their RI upon institution of anti-myeloma induction therapy. This study demonstrated an improvement in survival among NDMM patients with RI as a result of novel agent therapy as seen in Figure 2. Furthermore this study suggests that though RI in NDMM patients is associated with a worse OS as well as higher rates of early mortality, it is not an independent predictor of worse OS as seen in the multivariable model (Table 2). However, this study demonstrates that even if NDMM patients with RI experience a resolution of their RI upon receiving myeloma directed therapy (group 2), they do not have equivalent survival outcomes to those NDMM patients without RI (group 1) as seen in Figure 3a. Furthermore, even after accounting for early mortality by performing a landmark analysis at 6 months, patients in group 2 still do not have equivalent survival outcomes as those patients in group 1 (Figure 2). However, reversal of RI is still important to achieve in NDMM patients. This is because patients in group 3 who have RI at diagnosis but never recover their renal function have a worse median OS to patients in group 2 (33 vs 56 months, P=0.006). This survival benefit of reversal of RI seen in group 2 is observed likely due to their significantly lower rate of early mortality in comparison to group 3 (8 vs 17%; P=0.004). When a landmark analysis was performed at 6 months, the median OS for patients in group 2 compared to group 3 was 67 vs 51 months (P=0.175).
Our study also evaluated the renal function of all the patients at their last follow-up. We observed that even though patients in group 2 had a reversal of their RI, they were more likely to eventually re-worsen their renal function and experience RI again compared to the patients in group 1 (34 vs 9%; P<0.001); this suggests that NDMM patients with RI at diagnosis likely have a higher propensity for RI during their disease course compared to their NDMM counterparts who do not have RI at diagnosis.
Several studies have confirmed the beneficial effect of novel agent induction therapy in NDMM patients with RI in comparison to conventional chemotherapy.27, 28 This is likely because novel agents have been associated with improved depth of paraprotein response in myeloma and this likely translates to higher rates of improvement in renal function.29, 30, 31, 32 RI at diagnoses has not been found to weaken the responses provided by novel agent induction therapy.33 Furthermore, unlike most conventional chemotherapeutic agents, novel agents such as bortezomib and thalidomide have safe pharmacokinetic and pharmacodynamic properties in the setting of severe RI;34 lenalidomide, even though it is mainly renally excreted, can also be safely used if appropriate dose modifications are implemented and close evaluation for toxicities are undertaken in patients with mild to moderate RI.35 Novel agents such as bortezomib have also been reported to have protective effects in the renal tubular cells36 and inhibitory effects on the pro-inflammatory and fibrotic pathways within the renal microenvironment37 in addition to its previously described anti-myeloma activity.
However, despite the survival gains experienced with the emergence of novel agents in the upfront management of MM patients with RI at diagnosis, there is still room for improvement. Acute renal failure has been a major cause of early mortality in previous observational studies involving NDMM patients.9, 38 Even in this study, we observed a 16% early mortality rate in NDMM patients with CrCl<40 ml/min treated with a novel agent induction regimen; this signifies the need for earlier and more effective interventions in this subgroup of patients.
Our study also indicated that certain patient and disease-related characteristics predicted for the presence of RI at diagnosis in NDMM patients. Age >70 years was the only patient characteristic associated with RI at diagnosis. However, higher disease burden as suggested by an international staging system 3, high-risk cytogenetics by FISH, light-chain-secreting-only disease, higher bone marrow plasma cell percentage and higher LDH were all determinants of plasma cell biology that were associated with RI at diagnosis. In contrast, only NDMM patients who did not have light-chain-secreting-only disease were most likely to recover their renal function. In this study, older age, high-risk FISH, elevated LDH, high plasma cell labeling index and lack of novel agent use during induction were independent predictors of worse OS. This suggests that RI at diagnosis may not be an adverse prognostic marker in NDMM patients. In a study by Eleftherakis-Papapiakovou et al.,19 RI was also not found to be independently associated with inferior survival likely as a result of novel agent use during induction therapy.
There are several limitations to this study. First, the etiology of RI in each patient was not included in the analyses. Given the advanced age of the average NDMM patient, it is possible that their RI can also be associated with a decline in renal function as a result of other medical comorbidities such as diabetes, hypertension, vascular disease, drug-induced issues and so on. unrelated to the MM. Furthermore, a renal biopsy is not necessarily required or performed in every NDMM patient with RI11 and we do not have that information on all of our patients making it difficult to know the true etiology of RI in our patient population. Second, we are unable to determine with certainty whether certain novel agents used during induction such as bortezomib is superior to immunomodulators like thalidomide or lenalidomide in this subpopulation with RI due to the potential bias in patient selection for certain therapies and the high likelihood of most patients receiving bortezomib in the salvage setting. Third, the retrospective nature of this study prevents us from truly understanding the etiology of early mortality in these patients, that is, disease-related morbidity vs therapy-related toxicity leading to early mortality. Also in patients with acute renal impairment, the traditional equations to calculate glomerular filtration rate such as the MDRD formula do not provide accurate assessments of their true CrCl.39 Nevertheless, the MDRD equation has been adopted by the IMWG in monitoring renal function and response in patients with newly diagnosed MM. 11
Data from randomized control trials comparing different induction therapy regimens in NDMM patients with RI are sparse. Nevertheless, our data confirm the improvement in renal response that novel agents have had on NDMM patients with RI. They have also decreased early mortality in these patients as well as improved OS. However, reversal of RI alone does not appear to elevate the expected OS of such NDMM patients with RI at diagnosis to that of patients without RI at diagnosis. The findings from this study imply the need for instituting early treatment strategies in order to prevent patients from developing RI. For example, redefining the existing CRAB criteria required to diagnose MM by including criteria such as free light chain ratio >100 (ref. 40) or a bone marrow plasma cell percentage of 60 or higher41 may identify NDMM patients requiring therapy prior to them developing RI. In addition, for those NDMM patients already with RI, further work is required to determine the optimal management so as to continue to reduce associated morbidity and mortality.
References
Siegel R, Ma J, Zou Z, Jemal A . Cancer statistics, 2014. CA Cancer J Clin 2014; 64: 9–29.
Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003; 78: 21–33.
Knudsen LM, Hippe E, Hjorth M, Holmberg E, Westin J . Renal function in newly diagnosed multiple myeloma—a demographic study of 1353 patients. The Nordic Myeloma Study Group. Eur J Haematol 1994; 53: 207–212.
Kyle RA, Rajkumar SV . Multiple myeloma. N Engl J Med 2004; 351: 1860–1873.
Alexanian R, Barlogie B, Dixon D . Renal failure in multiple myeloma. Pathogenesis and prognostic implications. Arch Intern Med 1990; 150: 1693–1695.
Hutchison CA, Batuman V, Behrens J, Bridoux F, Sirac C, Dispenzieri A et al. The pathogenesis and diagnosis of acute kidney injury in multiple myeloma. Nat Rev Nephrol 2012; 8: 43–51.
Blade J, Fernandez-Llama P, Bosch F, Montoliu J, Lens XM, Montoto S et al. Renal failure in multiple myeloma: presenting features and predictors of outcome in 94 patients from a single institution. Arch Intern Med 1998; 158: 1889–1893.
Torra R, Blade J, Cases A, Lopez-Pedret J, Montserrat E, Rozman C et al. Patients with multiple myeloma requiring long-term dialysis: presenting features, response to therapy, and outcome in a series of 20 cases. Br J Haematol 1995; 91: 854–859.
Augustson BM, Begum G, Dunn JA, Barth NJ, Davies F, Morgan G et al. Early mortality after diagnosis of multiple myeloma: analysis of patients entered onto the United kingdom Medical Research Council trials between 1980 and 2002—Medical Research Council Adult Leukaemia Working Party. J Clin Oncol 2005; 23: 9219–9226.
Kleber M, Ihorst G, Terhorst M, Koch B, Deschler B, Wasch R et al. Comorbidity as a prognostic variable in multiple myeloma: comparative evaluation of common comorbidity scores and use of a novel MM-comorbidity score. Blood Cancer J 2011; 1: e35.
Dimopoulos MA, Terpos E, Chanan-Khan A, Leung N, Ludwig H, Jagannath S et al. Renal impairment in patients with multiple myeloma: a consensus statement on behalf of the International Myeloma Working Group. J Clin Oncol 2010; 28: 4976–4984.
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Kumar SK, Dispenzieri A, Lacy MQ, Gertz MA, Buadi FK, Pandey S et al. Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Leukemia 2014; 28: 1122–1128.
Brenner H, Gondos A, Pulte D . Recent major improvement in long-term survival of younger patients with multiple myeloma. Blood 2008; 111: 2521–2526.
Chanan-Khan AA, Swaika A, Paulus A, Kumar SK, Mikhael JR, Rajkumar SV et al. Pomalidomide: the new immunomodulatory agent for the treatment of multiple myeloma. Blood Cancer J 2013; 3: e143.
Dimopoulos MA, Swern AS, Li JS, Hussein M, Weiss L, Nagarwala Y et al. Efficacy and safety of long-term treatment with lenalidomide and dexamethasone in patients with relapsed/refractory multiple myeloma. Blood Cancer J 2014; 4: e257.
Dimopoulos MA, Delimpasi S, Katodritou E, Vassou A, Kyrtsonis MC, Repousis P et al. Significant improvement in the survival of patients with multiple myeloma presenting with severe renal impairment after the introduction of novel agents. Ann Oncol 2014; 25: 195–200.
Dimopoulos MA, Roussou M, Gkotzamanidou M, Nikitas N, Psimenou E, Mparmparoussi D et al. The role of novel agents on the reversibility of renal impairment in newly diagnosed symptomatic patients with multiple myeloma. Leukemia 2013; 27: 423–429.
Eleftherakis-Papapiakovou E, Kastritis E, Roussou M, Gkotzamanidou M, Grapsa I, Psimenou E et al. Renal impairment is not an independent adverse prognostic factor in patients with multiple myeloma treated upfront with novel agent-based regimens. Leuk Lymphoma 2011; 52: 2299–2303.
Knudsen LM, Hjorth M, Hippe E . Renal failure in multiple myeloma: reversibility and impact on the prognosis. Nordic Myeloma Study Group. Eur J Haematol 2000; 65: 175–181.
Greipp PR, San Miguel J, Durie BG, Crowley JJ, Barlogie B, Blade J et al. International staging system for multiple myeloma. J Clin Oncol 2005; 23: 3412–3420.
Kapoor P, Fonseca R, Rajkumar SV, Sinha S, Gertz MA, Stewart AK et al. Evidence for cytogenetic and fluorescence in situ hybridization risk stratification of newly diagnosed multiple myeloma in the era of novel therapie. Mayo Clin Proc 2010; 85: 532–537.
Kalff A, Spencer A . The t(4;14) translocation and FGFR3 overexpression in multiple myeloma: prognostic implications and current clinical strategies. Blood Cancer J 2012; 2: e89.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999; 130: 461–470.
Kyle RA, Rajkumar SV . Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia 2009; 23: 3–9.
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 2014; 15: e538–e548.
Roussou M, Kastritis E, Christoulas D, Migkou M, Gavriatopoulou M, Grapsa I et al. Reversibility of renal failure in newly diagnosed patients with multiple myeloma and the role of novel agents. Leuk Res 2010; 34: 1395–1397.
Kastritis E, Anagnostopoulos A, Roussou M, Gika D, Matsouka C, Barmparousi D et al. Reversibility of renal failure in newly diagnosed multiple myeloma patients treated with high dose dexamethasone-containing regimens and the impact of novel agents. Haematologica 2007; 92: 546–549.
Tosi P, Zamagni E, Cellini C, Cangini D, Tacchetti P, Tura S et al. Thalidomide alone or in combination with dexamethasone in patients with advanced, relapsed or refractory multiple myeloma and renal failure. Eur J Haematol 2004; 73: 98–103.
Tosi P, Zamagni E, Tacchetti P, Ceccolini M, Perrone G, Brioli A et al. Thalidomide-dexamethasone as induction therapy before autologous stem cell transplantation in patients with newly diagnosed multiple myeloma and renal insufficiency. Biol Blood Marrow Transplant 2010; 16: 1115–1121.
Dimopoulos MA, Richardson PG, Schlag R, Khuageva NK, Shpilberg O, Kastritis E et al. VMP (bortezomib, melphalan, and Prednisone) is active and well tolerated in newly diagnosed patients with multiple myeloma with moderately impaired renal function, and results in reversal of renal impairment: cohort analysis of the phase III VISTA study. J Clin Oncol 2009; 27: 6086–6093.
Ludwig H, Adam Z, Hajek R, Greil R, Tothova E, Keil F et al. Light chain-induced acute renal failure can be reversed by bortezomib-doxorubicin-dexamethasone in multiple myeloma: results of a phase II study. J Clin Oncol 2010; 28: 4635–4641.
Dimopoulos M, Alegre A, Stadtmauer EA, Goldschmidt H, Zonder JA, de Castro CM et al. The efficacy and safety of lenalidomide plus dexamethasone in relapsed and/or refractory multiple myeloma patients with impaired renal function. Cancer 2010; 116: 3807–3814.
Eriksson T, Hoglund P, Turesson I, Waage A, Don BR, Vu J et al. Pharmacokinetics of thalidomide in patients with impaired renal function and while on and off dialysis. J Pharm Pharmacol 2003; 55: 1701–1706.
Dimopoulos MA, Christoulas D, Roussou M, Kastritis E, Migkou M, Gavriatopoulou M et al. Lenalidomide and dexamethasone for the treatment of refractory/relapsed multiple myeloma: dosing of lenalidomide according to renal function and effect on renal impairment. Eur J Haematol 2010; 85: 1–5.
Sarkozi R, Perco P, Hochegger K, Enrich J, Wiesinger M, Pirklbauer M et al. Bortezomib-induced survival signals and genes in human proximal tubular cells. J Pharmacol Exp Ther 2008; 327: 645–656.
Ying WZ, Wang PX, Aaron KJ, Basnayake K, Sanders PW . Immunoglobulin light chains activate nuclear factor-kappaB in renal epithelial cells through a Src-dependent mechanism. Blood 2011; 117: 1301–1307.
Kastritis E, Terpos E, Roussou M, Eleutherakis-Papaiakovou E, Gavriatopoulou M, Kalapanida D et al. Very early death (<2 months) in myeloma is associated with advanced age, poor performance status and reduced use of novel agents, while early death within 12 months is associated with high risk features of both the disease and the patient. ASH 2013 Annual Meeting 2013, Abstract 3195.
Pickering JW, Endre ZH . Back-calculating baseline creatinine with MDRD misclassifies acute kidney injury in the intensive care unit. Clin J Am Soc Nephrol 2010; 5: 1165–1173.
Larsen JT, Kumar SK, Dispenzieri A, Kyle RA, Katzmann JA, Rajkumar SV . Serum free light chain ratio as a biomarker for high-risk smoldering multiple myeloma. Leukemia 2013; 27: 941–946.
Rajkumar SV, Larson D, Kyle RA . Diagnosis of smoldering multiple myeloma. N Engl J Med 2011; 365: 474–475.
Acknowledgements
This work was supported in part by Mayo Clinic Hematological Malignancies Program, Paul Calabresi K12 Award (CA96028). This study was also supported in part by grants CA 107476, CA 62242, CA100707 and CA 83724 from the National Cancer Institute, Rockville, MD, USA. This publication was also made possible by the CTSA Grant UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH).
Author Contributions
SKK designed the study. SKK and WIG collected and analyzed the data and wrote the manuscript. NL, SVR, MAG, AD, MQL, FKB, RSG, DD, SRH, JAL, YL, SJR, SZ, RAK and PK contributed to writing and reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Gonsalves, W., Leung, N., Rajkumar, S. et al. Improvement in renal function and its impact on survival in patients with newly diagnosed multiple myeloma. Blood Cancer Journal 5, e296 (2015). https://doi.org/10.1038/bcj.2015.20
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2015.20
This article is cited by
-
Multiple myeloma with acute light chain cast nephropathy
Blood Cancer Journal (2023)
-
Autologous stem cell transplantation for multiple myeloma patients with chronic kidney disease: a safe and effective option
Bone Marrow Transplantation (2022)
-
Procollagen C-proteinase enhancer-1 and renal failure in multiple myeloma
International Urology and Nephrology (2022)
-
Kidney injury and disease in patients with haematological malignancies
Nature Reviews Nephrology (2021)
-
Use of bisphosphonates in multiple myeloma patients in Denmark, 2005–2015
Supportive Care in Cancer (2021)