Abstract
Recent studies have reported an increased risk of second primary malignancies (SPM) following multiple myeloma (MM) diagnosis associated with novel anti-myeloma treatments. We evaluated the risk of SPM among 36 491 MM cases reported to the Surveillance, Epidemiology, and End Results program (SEER) between 1973 and 2008. We calculated overall and site-specific standardized incidence ratio (SIR) and 95% confidence intervals (CI) for 2012 SPM cases diagnosed within the 35-year follow-up. There was no significant overall risk of SPM (SIR=0.98; 95% CI=0.94–1.02); however, there were multiple site-specific risk patterns. The risk of breast and prostate cancer was significantly decreased overall and across age, latency and the year of diagnosis strata. There was an ∼50% increased risk of colorectal cancer 5 years after MM diagnosis (Ptrend<0.001). The risk of hematological malignancies was significantly increased, notably for acute myeloid leukemia (AML; SIR=6.51; 95% CI=5.42–7.83). There was a significant decreasing trend for AML over time, particularly for patients ⩾65. However, no significant change in risk was noted after the introduction of autologous stem cell transplant among younger patients (<65 years). On the basis of observed trends for overall SPM as well as AML, no association between the introduction of novel therapies and SPM following MM has emerged in this large population-based study.
Similar content being viewed by others
Introduction
Major advancements in the treatment of multiple myeloma (MM) have included the introduction of combination high-dose melphalan and autologous stem cell transplant (ASCT) in the 1980s,1 and the introduction of novel anti-myeloma agents such as thalidomide,2 bortezomib3 and lenalidomide4 over the past decade. These have led to improved patient outcomes, resulting in increased survival when compared with a dismal prognosis just 10 years ago.5 However, an emerging challenge has been to manage other medical conditions that may arise in patients with a longer survival, including second primary malignancies (SPM). Previous clinical studies have reported an occurrence of SPM in 1–12% of MM patients.6, 7, 8, 9, 10, 11 Studies based on the cancer registry data, more generalizable to the entire population, conducted before the introduction of novel anti-myeloma treatments, reported no overall increased risk of SPM among MM patients; however, these studies noted an increased incidence of hematological malignancies and significant heterogeneity in the risk of solid tumor SPM subtypes.12, 13 The development of SPM is multicausal; risk factors may include MM-related factors including treatment and tumor microenvironment, as well as host-related processes including genetic and environmental factors.14 Reports from ongoing randomized clinical trials have suggested a possible higher incidence of SPM in MM patients treated with certain novel anti-myeloma treatments, particularly immunomodulatory drugs (IMiDs).15, 16, 17 A recent study of 8740 MM patients from Sweden reported an overall 20% increased risk of SPM, but no significant change in the risk of acute myeloid leukemia (AML) after the introduction of novel therapeutic agents and ASCT.18
We conducted a large population-based study of SPM in MM patients using data from a 35-year follow-up period (1973–2008) to examine the risk patterns of SPM following MM, to provide information on the public health burden of SPM following MM and to further characterize the population at risk.
Materials and methods
Patients
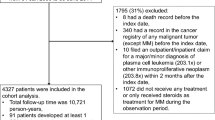
We utilized data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program’s original nine registries (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle and Utah) with incidence data contributed over a 35-year interval (1973–2008).19 MM patients were defined using the third edition of the International Classification of Diseases for Oncology codes 9732 and 9734. We excluded cases whose reporting sources were coded as autopsy- or death-certificate-only (n=775), cases where MM was not the first primary cancer diagnosis (n=3545) and cases with SPM diagnosed within the first 2 months of MM diagnosis (n=365).
Statistical analysis
To estimate SPM risk, we defined a cohort of MM patients with no previous history of malignancy. Person-years for age strata (5-year age-groups), sex, race (white, black, other) and the year of diagnosis were calculated from 2 months after diagnosis of MM to the date of death, date of diagnosis of SPM, date of loss to follow-up or the end of study (31 December 2008), whichever came first. General population incidence rates for each stratum were multiplied by their respective accumulated person-years-at-risk to estimate the overall expected cancer cases in that cohort of MM patients. We calculated the standardized incidence ratio (SIR) by dividing the observed number of SPM cases by the expected number based on the general population rates. The 95% confidence intervals (CI) were calculated using Fisher’s exact test. We used likelihood ratio tests based on Poisson regression models that included SEER registries general population rates to evaluate linear trends and heterogeneity across different SPM sites, with at least five observed occurrences in each stratum. We further performed multivariate Poisson regression analysis adjusted for age, sex and latency to compare the SIRs across different year categories. All analyses were completed using SEER*Stat Version 7.0.5 statistical software (Surveillance Research Program, NCI, http://www.seer.cancer.gov/seerstat) and Stata version 11.2 (StataCorp LP, College Station, TX, USA).
Detailed treatment information is not available from the SEER database. To generate hypotheses regarding the effect of anti-myeloma therapy on SPM, we used diagnosis periods corresponding to the introduction of new treatments, similar to previously published population-based analyses without treatment data.5, 18 Categories include: 1973–1984, representing the use of alkylating agents and steroids; 1985–1999, representing the introduction of high-dose melphalan and ASCT; and 2000–2008, representing the introduction of novel treatments (IMiDs and proteasome inhibitors).20 We further stratified by latency period, under the assumption that treatment-related SPM are more likely to increase with latency. On the basis of the likely MM treatments used for different age groups, we categorized age into three main age categories (<65, 65–75 and ⩾75). To evaluate the effect of ASCT on risk of AML, we further stratified the analysis by 5-year time periods and two age categories (<65 and ⩾65), with the assumption that ASCT was most commonly offered to patients <65 years.
Results
Overall, 36 491 cases of adult MM were recorded as the first primary malignancy in the SEER registries between 1973 and 2008, and of these 2021 cases had a diagnosed SPM. The MM patients were at risk for a mean time of 3.1 years and contributed 113 275 person-years in total. The mean age at MM diagnosis for patients with SPM was similar to the overall mean age of all MM patients (68.2 years vs 68.7 years, respectively). Patient characteristics are summarized in Table 1.
Overall and sex-specific risk
There was no significant difference in the overall risk of SPM among MM patients compared with the US general population (SIR=0.98; 95% CI=0.94–1.02; Figure 1). We observed a modest statistically significant decreased risk of SPM for solid tumors (n=1707, SIR=0.92; 95% CI=0.88–0.97) among MM patients, with heterogeneity by SPM type. There was a lower risk of esophagus (SIR=0.49; 95% CI=0.28–0.87), lung/bronchus (SIR=0.88; 95% CI=0.78–0.99), breast (SIR=0.81; 95% CI=0.69–0.94) and prostate (SIR=0.69; 95% CI=0.61–0.77) cancers, but a higher risk of melanoma (SIR=1.36; 95% CI=1.07–1.74), urinary bladder (SIR=1.22; 95% CI=1.03–1.44), kidney/renal pelvis (SIR=1.30; 95% CI=1.01–1.66) and thyroid (SIR=1.63; 95% CI=1.05–2.52) SPM. There was no statistically significant difference in sex-specific risks of solid tumor SPM.
A statistically significant increased risk was observed for all hematological malignancies (n=263, SIR=1.63; 95% CI=1.45–1.84; Figure 1). There was a statistically significant increased risk of leukemias (SIR=2.94; 95% CI=2.52–3.43), with the highest risk observed for AML (SIR=6.51; 95% CI=5.42–7.83), the most common hematological SPM (n=114). Chronic lymphocytic leukemia was the only leukemia subtype that MM patients were less likely to develop (SIR=0.34; 95% CI=0.17–0.68). Overall, there was a 27% increase in the risk of lymphomas, mostly non-Hodgkin subtype (SIR=1.28; 95% CI=1.04–1.57). Among the hematological malignancies, women had a significantly higher risk of leukemias (female: SIR=3.85; 95% CI=3.07–4.83, male: SIR=2.44; 95% CI=1.97–3.01; Pheterogeneity=0.004).
Latency and risk
The mean latency time to develop SPM among MM patients was 5.21 years (95% CI=4.98–5.45). Overall, there was a statistically significant increase in the risk of SPM by latency period (Ptrend<0.001), with the most significant increase observed in hematological malignancies (Figure 2). The strongest association was observed for AML, with a 78% increase in risk within the first 2 years (SIR=1.78; 95% CI=1.03–3.06) and over a 10-fold increased risk after 5 years of MM diagnosis (SIR=10.77; 95% CI=8.09–14.33). An increased risk of non-Hodgkin lymphoma was present only after 5 years of MM diagnosis (SIR=1.79; 95% CI=1.27–2.52).
We observed no change in risk associated with the latency period for most solid tumors (Figure 2). The risk of breast and prostate cancers remained significantly decreased after MM diagnosis (Ptrend=0.65, Ptrend=0.51, respectively). A significant increasing trend in the risk of colorectal cancer was associated with latency (Ptrend<0.001), with an almost 50% increased risk 5 years after MM diagnosis (SIR=1.46; 95% CI=1.20–1.78). An increased risk of the central nervous system, thyroid, small intestine and kidney cancers was observed within the first 2 years of MM diagnosis only.
Age-specific risk
SIRs for SPM decreased with increasing age, (<65 years: SIR=1.09; 95% CI=1.01–1.18, ⩾75 years: SIR=0.87; 95% CI=0.80–0.94; Ptrend<0.001; Figure 3). This pattern was most prominent in hematological malignancies (<65 years: SIR=2.18; 95% CI=1.78–2.67, ⩾75 years: SIR=1.01; 95% CI=0.78–1.30; Ptrend<0.001), notably for AML (<65 years: SIR=11.92; 95% CI=8.95–15.86, ⩾75 years: SIR=2.28; 95% CI=1.40–3.72). Among solid tumors, change in risk across age strata was more heterogeneous. The risk of prostate and breast cancer remained lower than the general population among all age categories. There was a significant decrease in the urinary bladder and lung/bronchus cancer risk with increasing age (Ptrend=0.015 and 0.003, respectively).
Secular trend
There was no change in the overall and site-specific risk of solid tumor SPM over time (Figure 4). In contrast, we observed a significant decreased risk of hematological malignancies by time, mostly attributable to a significantly decreasing trend in AML risk. The 12-fold excess risk of AML among MM patients diagnosed in 1973–1977 decreased to a fourfold excess risk in 2000–2008 (Ptrend<0.001). To further investigate this finding, we stratified by 5-year MM diagnosis period and age at MM diagnosis (Figure 5). The decreasing trend by year of diagnosis was observed across age categories and was most prominent among patients ⩾65 years (Ptrend<0.001). Younger patients had a consistently higher risk of AML across all time periods.
Novel anti-myeloma therapeutics and ASCT
There was no significant change in the risk of SPM when risks were compared before and after the introduction of novel therapies (1985–1999: SIR=0.95; 95% CI=0.90–1.02, 2000–2008: SIR=0.96; 95% CI=0.88–1.06). This was true for both solid tumors (1985–1999: SIR=0.92; 95% CI=0.86–0.98, 2000–2008: SIR=0.91; 95% CI=0.82–1.00) and hematological malignancies (1985–1999: SIR=1.45; 95% CI=1.21–1.73, 2000–2008: SIR=1.43; 95% CI=1.10–1.85). In an analysis stratified by age categories to further evaluate the effect of ASCT and novel therapies on AML risk, we did not observe an increase in the risk of AML in either age group since the introduction of novel anti-myeloma therapies (Figure 5). We also observed no change in risk in patients <65 years after the introduction of ASCT (Pheterogeneity=0.43). We performed a multivariate analysis adjusted for age, sex and latency, and did not observe any differences in SPM risk before and after novel therapies were introduced (P=0.42).
Discussion
To our knowledge, this is the largest and most current population-based study to evaluate the risk of SPM following MM diagnosis. Our results demonstrate significant heterogeneity in risk by SPM site by age, sex, latency and secular trends, with the most significant risks noted for AML.
We observed an overall sevenfold increased risk of AML following MM diagnosis, similar to increased risks reported in previous clinical and population-based studies.7, 8, 9, 18, 21 Although the etiology is unclear, this increased risk has previously been attributed to treatment-related factors including the use of alkylators such as melphalan.7, 8, 9 In our study, AML risk significantly increased with increasing latency, consistent with the hypothesis that large numbers of AML cases can be attributed to treatment. Overall, younger patients had a significantly higher risk of AML compared with older patients, which may be associated with a more aggressive use of alkylators in the younger age group. To further evaluate the effect of ASCT on AML risk, we analyzed risk by age and time period under the assumption that ASCT was introduced in the United States in the mid-1980s and was widely used by the late 1990s.20 Although there are differences in practice across centers, overall ASCT is more likely be offered to patients <65 years.22, 23 There was a decreasing trend in the risk of AML by time, but no significant change in risk after the introduction of ASCT. Although SEER does not provide individual-level treatment data, the general patterns we observed in risk trends are consistent with the findings of a recent smaller Swedish study, which reported no significant change in the risk of AML following the introduction of ASCT.18 The common practice before ASCT was the use of prolonged low-dose alkylator-based therapies. The fact that AML risk has not changed with the introduction of high-dose short-term alkylators suggests that the cumulative dose of alkylators may be more important than the duration of treatment.7, 8, 21 We found a significant 80% increased risk of AML within the first 2 years of MM diagnosis, which cannot be explained by treatment-related factors but rather similar pathogenic/etiological mechanisms, as yet unknown.
We observed a statistically significant decreased risk in breast and prostate cancer, which was consistent across time period, latency and age strata. Previous studies have reported a reduced risk of breast cancer and no effect on the risk of prostate cancer following MM diagnosis. As our analyses were conducted in a much larger population, they are more likely to reflect true population trends.10, 21 Although biological mechanisms for SPM after MM are not well defined, Thomas et al.14 described a model of SPM involving treatment, behavioral factors, MM-related factors, host genetic factors and environmental factors. Within this model, genetic variation or environmental exposures that increase the risk of MM could be protective for breast and prostate cancers. For example, polymorphisms in MTHFR, a gene involved in the folate metabolizing pathway, have been associated with the risk of MM,24 while a meta-analysis found a polymorphism in the MTHFR gene to be protective in prostate cancer risk.25 In addition, both of these cancers are hormone related, and it is possible that MM pathogenesis modifies the levels of sex hormones or host-related factors with subsequent sustained decreased risk of these cancers throughout the survival time. A decrease in screening after MM diagnosis is another possible explanation for the decreased risk observed in both breast and prostate cancer. Further research is needed to explore these potential hypotheses.
In our study, there was a significant increased risk of colorectal cancer associated with latency. The fact that the risk of colorectal cancer was elevated after 5 years of MM diagnosis and was more prominent in the earlier time periods (1973–1984 and 1985–1999) is suggestive of MM treatment-related factors. A retrospective study in Japan also reported a significantly increased risk of colorectal cancer following MM diagnosis between 1984 and 1994.26 The increased risk of colorectal cancer after 5 years following MM diagnosis warrants attention to screening for colorectal cancer among the long-term MM survivors.
We found a 50% increased risk of urinary bladder cancer following MM in earlier time periods (1973–1984), among younger patients (age <65) and after 5 years of MM diagnosis. Although this pattern of risk is heterogeneous, it may suggest an association with MM-related factors, including MM therapy through chemotherapy-induced cystitis. Previous studies have also reported an increased risk of bladder cancer following MM diagnosis.18, 27
The increased risk of both melanoma and non-melanoma skin cancers after MM has been reported.18, 21 In our analysis, the increased risk of melanoma was not associated with the latency or year of diagnosis, suggesting that risk may be attributable to common etiological factors such as immune dysfunction, which is a major feature of MM28 and has also been implicated in the excessive risk of various skin cancers, specifically among organ transplant recipients.29
Results from three recent randomized clinical trials of maintenance therapy in MM patients after first induction therapy in the transplant and non-transplant setting suggest an increased risk of SPM among patients who received the maintenance therapy with lenalidomide as compared with the placebo group.15, 16, 17 The rate of SPM was variable in these three trials with respect to the number as well as type of the SPM. On the basis of this data, the International Myeloma Working Group suggested weighing the potential benefit of maintenance therapy with IMiDs with the risk of SPM in these patients.30 It is important to note that all the patients enrolled in these trials had been previously exposed to alkylating agents as induction or pre-transplant conditioning. Furthermore, the fact that the incidence and distribution of SPM across the three trials were variable and the sample size was relatively small, it precludes definitive conclusions, especially on a population-wide basis. Our findings suggest no change in SPM risk since the introduction of IMiDs. To further investigate these findings, we performed a sensitivity analysis using the SEER 13 data set, which includes information from the nine original SEER registries as well as four additional registries between 1992 and 2008. We similarly found no change in risk of AML as well as other SPMs since the introduction of novel therapies (data not shown). Other factors such as the combination of IMiDs with alkylators, sequence of therapy and the duration of continuous therapy may contribute to the findings in these clinical trials and should be better defined.
A major strength of our study is the large number of population-based MM cases identified in the time period, representing the novel therapeutic agent era. SEER ascertainment is >98%, which eliminates selection bias that is potentially introduced when using hospital-based populations and also expands the generalizability of the findings to patients who are not enrolled in clinical trials.
This study also has limitations. The SEER database does not include individual-level treatment information; thus, we were unable to test the hypothesis that secular trends were causally associated with treatment. Instead, we examined SPM incidence with dates of new treatment introductions as period cut-points and patient-age as proxies to generate hypotheses about the relationship between new treatments and SPM. This approach has previously been used to study the effect of changes in trends of therapeutic modalities.5, 18
MM is a relatively rare cancer and the survival time is shorter compared with other hematological malignancies, making SPM case ascertainment a challenge. Therefore, we chose to exclude cases diagnosed with a second cancer within the first 2 months of MM diagnosis. To address the issue of surveillance bias within the first year of a primary cancer diagnosis, we performed a sensitivity analysis excluding SPM cases diagnosed within the first year, and the results were similar.
In summary, there was no overall increased risk of SPM among MM patients, but several significant SPM patterns were described. In addition, our results provide epidemiological evidence that there has been no increase in population-based risk of SPM after the introduction of novel therapeutic agents. Follow-up studies with individual-level treatment data will be necessary to test this hypothesis conclusively.
References
McElwain TJ, Powles RL . High-dose intravenous melphalan for plasma-cell leukaemia and myeloma. Lancet 1983; 2: 822–824.
Singhal S, Mehta J, Desikan R, Ayers D, Roberson P, Eddlemon P et al. Antitumor activity of thalidomide in refractory multiple myeloma. N Engl J Med 1999; 341: 1565–1571.
Richardson PG, Barlogie B, Berenson J, Singhal S, Jagannath S, Irwin D et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med 2003; 348: 2609–2617.
Rajkumar SV, Hayman SR, Lacy MQ, Dispenzieri A, Geyer SM, Kabat B et al. Combination therapy with lenalidomide plus dexamethasone (Rev/Dex) for newly diagnosed myeloma. Blood 2005; 106: 4050–4053.
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Law IP, Blom J . Second malignancies in patients with multiple myeloma. Oncology 1977; 34: 20–24.
Bergsagel DE, Bailey AJ, Langley GR, MacDonald RN, White DF, Miller AB . The chemotherapy on plasma-cell myeloma and the incidence of acute leukemia. N Engl J Med 1979; 301: 743–748.
Cuzick J, Erskine S, Edelman D, Galton DA . A comparison of the incidence of the myelodysplastic syndrome and acute myeloid leukaemia following melphalan and cyclophosphamide treatment for myelomatosis. A report to the Medical Research Council’s working party on leukaemia in adults. Br J Cancer 1987; 55: 523–529.
Govindarajan R, Jagannath S, Flick JT, Vesole DH, Sawyer J, Barlogie B et al. Preceding standard therapy is the likely cause of MDS after autotransplants for multiple myeloma. Br J Haematol 1996; 95: 349–353.
Acute leukaemia and other secondary neoplasms in patients treated with conventional chemotherapy for multiple myeloma: a Finnish Leukaemia Group study. Eur J Haematol 2000; 65: 123–127.
Przepiorka D, Buadi F, McClune B, Franz G, Walsh W, White F . Myelodysplastic syndrome after autologous peripheral blood stem cell transplantation for multiple myeloma. Bone Marrow Transplant 2007; 40: 759–764.
Dong C, Hemminki K . Second primary neoplasms among 53 159 haematolymphoproliferative malignancy patients in Sweden, 1958-1996: a search for common mechanisms. Br J Cancer 2001; 85: 997–1005.
Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK et al(eds) New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1973-2000. National Cancer Institute, NIH: Bethesda, 2006.
Thomas A, Mailankody S, Korde N, Kristinsson SY, Turesson I, Landgren O . Second malignancies after multiple myeloma: from 1960s to 2010s. Blood 2012; 119: 2731–2737.
Palumbo A, Hajek R, Delforge M, Kropff M, Petrucci MT, Catalano J et al. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. N Engl J Med 2012; 366: 1759–1769.
Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1782–1791.
McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1770–1781.
Mailankody S, Pfeiffer RM, Kristinsson SY, Korde N, Bjorkholm M, Goldin LR et al. Risk of acute myeloid leukemia and myelodysplastic syndromes after multiple myeloma and its precursor disease (MGUS). Blood 2011; 118: 4086–4092.
Surveillance Epidemiology and End Results (SEER) ProgramSEER*Stat Database: Incidence - SEER 9 Regs Research Data, November 2010 Sub (1973-2008) (Katrina/Rita Population Adjustment) - Linked To County Attributes - Total U.S., 1969-2009 Counties. In: National Cancer Institute D, Surveillance Research Program, Cancer Statistics Branch (ed.); April 2011.
Kyle RA, Rajkumar SV . Multiple myeloma. Blood 2008; 111: 2962–2972.
Hasskarl J, Ihorst G, De Pasquale D, Schrottner P, Zerweck A, Wasch R et al. Association of multiple myeloma with different neoplasms: systematic analysis in consecutive patients with myeloma. Leuk Lymphoma 2011; 52: 247–259.
Attal M, Harousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Francais du Myelome. N Engl J Med 1996; 335: 91–97.
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K et al. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med 2003; 348: 1875–1883.
Zintzaras E, Giannouli S, Rodopoulou P, Voulgarelis M . The role of MTHFR gene in multiple myeloma. J Hum Genet 2008; 53: 499–507.
Li XL, Xu JH . MTHFR polymorphism and the risk of prostate cancer: a meta-analysis of case-control studies. Prostate Cancer Prostatic Dis 2012; 15: 244–249.
Kishida T, Yonezawa M, Shibata Y, Tanaka S, Shinozawa I, Hoshino T et al. Risk of colorectal cancer in patients with hematologic disease. J Gastroenterol Hepatol 2000; 15: 1272–1276.
Cannon MJ, Flanders WD, Pellett PE . Occurrence of primary cancers in association with multiple myeloma and Kaposi’s sarcoma in the United States, 1973-1995. Int J Cancer 2000; 85: 453–456.
Pratt G, Goodyear O, Moss P . Immunodeficiency and immunotherapy in multiple myeloma. Br J Haematol 2007; 138: 563–579.
Engels EA, Pfeiffer RM, Fraumeni JF Jr., Kasiske BL, Israni AK, Snyder JJ et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA 2011; 306: 1891–1901.
Ludwig H, Durie BG, McCarthy P, Palumbo A, San Miguel J, Barlogie B et al. IMWG consensus on maintenance therapy in multiple myeloma. Blood 2012; 119: 3003–3015.
Acknowledgements
This work was presented in part as an oral presentation at the 2011 Annual Meeting of the American Society of Hematology, San Diego, CA, USA. We thank Susan Groshen, PhD (Division of Biostatics, Department of Preventive Medicine, USC) for her insightful comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author Contributions
PR contributed to the study design, data analysis, interpretation and manuscript preparation; KR and WC contributed in interpretation and manuscript preparation; SU and AC contributed to manuscript preparation; and SA performed study design, interpretation and manuscript preparation.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Razavi, P., Rand, K., Cozen, W. et al. Patterns of second primary malignancy risk in multiple myeloma patients before and after the introduction of novel therapeutics. Blood Cancer Journal 3, e121 (2013). https://doi.org/10.1038/bcj.2013.19
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2013.19
Keywords
This article is cited by
-
Increased mortality risk in multiple-myeloma patients with subsequent malignancies: a population-based study in the Netherlands
Blood Cancer Journal (2022)
-
The mutagenic impact of melphalan in multiple myeloma
Leukemia (2021)
-
Effect of autologous hematopoietic stem cell transplant on the development of second primary malignancies in multiple myeloma patients
Blood Cancer Journal (2021)
-
Is the risk of second primary malignancy increased in multiple myeloma in the novel therapy era? A population-based, retrospective cohort study in Taiwan
Scientific Reports (2020)
-
Clinical outcomes and prognostic factors in patients with multiple myeloma in South Tyrol: a retrospective single-center analysis
Annals of Hematology (2020)