Abstract
Natural killer (NK) cells are potential effector cells in cell-based cancer immunotherapy, particularly in the control of hematological malignancies. The chimeric antigen receptor (CAR) is an artificially modified fusion protein that consists of an extracellular antigen recognition domain fused to an intracellular signaling domain. T cells genetically modified with a CAR have demonstrated remarkable success in the treatment of hematological cancers. Compared to T cells, CAR-transduced NK cells (CAR-NK) exhibit several advantages, such as safety in clinical use, the mechanisms by which they recognize cancer cells, and their abundance in clinical samples. Human primary NK cells and the NK-92 cell line have been successfully transduced to express CARs against both hematological cancers and solid tumors in pre-clinical and clinical trials. However, many challenges and obstacles remain, such as the ex vivo expansion of CAR-modified primary NK cells and the low transduction efficiency of NK cells. Many strategies and technologies have been developed to improve the safety and therapeutic efficacy in CAR-based immunotherapy. Moreover, NK cells express a variety of activating receptors (NKRs), such as CD16, NKG2D, CD226 and NKp30, which might specifically recognize the ligands expressed on tumor cells. Based on the principle of NKR recognition, a strategy that targets NKRs is rapidly emerging. Given the promising clinical progress described in this review, CAR- and NKR-NK cell-based immunotherapy are likely promising new strategies for cancer therapy.
Similar content being viewed by others
Introduction
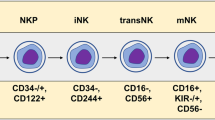
Natural killer (NK) cells are potential effector cells in cell-based cancer immunotherapy, particularly in the control of hematological malignancies1. Initial studies of NK cell immunotherapy employed autologous NK cells activated by interleukin-2 (IL-2). However, this approach resulted in poor clinical outcomes, mainly due to the suppression of autologous NK cells because ligands presented by self-human leukocyte antigen (HLA) molecules on tumor cells bound to killer inhibitory receptors (KIR) on NK cells. The transfer of allogeneic or haploidentical NK cells with KIR ligand-mismatch avoids this suppression due to the “missing self” recognition of tumor cells2. Thus, allogeneic NK cell infusions are safe and can eliminate leukemia relapse without leading to graft-versus-host disease (GVHD). However, therapy with adoptively transferred NK cells purified from peripheral blood (PB) has been limited due to the short life span of these cells in vivo (usually a few days up to a few weeks)3,4. Recent studies have shown that cytokines can induce NK cells to become memory-like NK cells, which have a longer life span in vivo5. By briefly pre-activating cells with IL-12, IL-15, and IL-18, memory-like NK cells differentiate and exhibit enhanced IFN-γ production and cytotoxicity against leukemia cells both in vitro and in vivo. In a phase I clinical trial, clinical responses were observed in five of nine evaluable patients with acute myeloid leukemia, including four with complete remissions6. Importantly, IL-15-stimulated NK cell infusions show promising therapeutic efficacy in the treatment of solid tumors. Specifically, four of six pediatric patients with refractory solid tumors showed a clinical response, particularly one patient with very good partial remission and two patients with partial remission, after receiving haploidentical stem cell transplants7.
The chimeric antigen receptor (CAR) is an artificially modified fusion protein based on the T cell receptor, which consists of an extracellular antigen recognition domain fused to a variety of intracellular signaling domains. The extracellular domain of CARs is usually an antibody single-chain variable fragment (scFv) that recognizes the specific antigen (usually overexpressed on or unique to tumor cells) without presentation by major histocompatibility complex (MHC) molecules, similar to an antibody. The intracellular domains usually contain CD3ζ, CD28, 4-1BB, or OX40 and are designed to increase T cell activation. T cells genetically modified to express a CAR can directly recognize the CAR-targeted antigen and then trigger T cell activation, proliferation, cytokine secretion and cytotoxicity against tumor cells that express the CAR-specific antigen. Thus, CAR-modified T cell therapy has demonstrated remarkable success in the treatment of hematological cancers, including lymphoma, chronic lymphocytic leukemia, and acute lymphoblastic leukemia (ALL). Specifically, CD19-targeting CAR-T cells have been reported to result in complete response rates of 70% to 90% in patients with ALL8. However, CAR-modified T cells exhibit poor therapeutic efficacy for solid tumors9,10,11. In addition, the preparation of CAR-T cells usually requires patient autologous cells because of GVHD caused by allogeneic T cells12,13, which limits their broader clinical application. Moreover, the expansion and persistence of CAR-T cells in vivo may induce the release of pro-inflammatory cytokines, referred to as cytokine storms or cytokine release syndrome (CRS).
Similar to CAR-expressing T cells, CAR-modified NK cells exhibit improved tumor-specific targeting and cytotoxicity against cancer cells both in vitro and in vivo14,15. Importantly, NK cells have many advantages compared to T cells in CAR-targeted immunotherapy. For example, allogeneic NK cell can be used as effector cells since they are not responsible for GVHD because they do not require HLA matching. Furthermore, CAR-NK cells may be safer than CAR-T cells because they usually do not induce cytokine storms. Additionally, NK cells can be generated from different sources, such as PB, umbilical cord blood (UCB), human embryonic stem cells (hESCs), induced pluripotent stem cells (iPCSs), and even NK-92 cell lines. In this review, we will focus on recent advances in CAR-modified NK cell immunotherapy, including the advantages and current progress made in the use of CAR-engineered NK cells for tumor therapy in pre-clinical and clinical settings, the major obstacles to the translation of CAR-engineered NK cells to clinical practice, and novel strategies to enhance the safety and efficacy of CAR-expressing NK cells.
Advantages of CAR-NK cells for tumor immunotherapy
Despite the early success of CAR-T cell therapy, particularly in hematological malignancies, the large-scale clinical applications of CAR-T cell therapy may be limited by individualized preparation and various side effects, such as CRS, neurologic toxicities and on-target/off-tumor effects. Given these problems, NK cells have been proposed to be superior CAR drivers for T cells16. Specifically, NK cells have several advantages in CAR-based immunotherapy compared to T cells.
First, CAR-expressing NK cells might be safer than CAR-T cells in clinical use, and the safety of NK cell immunotherapy has been verified in several clinical fields. For example, several phase I/II trials showed that allogeneic NK cell infusions are tolerated well and do not lead to GVHD and serious toxicities17,18,19; therefore, NK cells are universal CAR drivers that are not limited to autologous cells. One of the main side effects in CAR-T cell therapy are on-target/off-tumor effects due to the persistence of CAR-T cells. For instance, CD19-targeting CAR-T cells can cause profound and long-lasting B-cell deficiency due to the cellular memory response of T cells and the attack of normal mature or progenitor B cells20. Fortunately, CAR-NK cells have a limited lifespan in the circulation, leading to few on-target/off-tumor effects. Furthermore, the types of cytokines produced by NK cells differ from those produced by T cells; activated NK cells usually produce IFN-γ and GM-CSF, whereas the cytokine storm induced by CAR-T cells is mainly mediated by pro-inflammatory cytokines, such as TNF-α, IL-1 and IL-6.
Second, in addition to killing target cells via a CAR-specific mechanism (recognizing the tumor-associated antigen via scFv), NK cells can spontaneously kill tumors cells by recognizing diverse ligands via a variety of activating receptors21,22, including natural cytotoxicity receptors (NKp46, NKp44, and NKp30), NKG2D and DNAM-1 (CD226). These activating NK cell receptors usually recognize stress-induced ligands expressed on tumor cells under the pressure of immune cells or long-term treatment during tumor evolution. Furthermore, NK cells mediate the antibody-dependent cell-mediated cytotoxicity (ADCC) via FcγRIII (CD16). Therefore, CAR-expressing NK cells can kill target cells via both CAR-dependent and NK cell receptor-dependent mechanisms to eradicate either tumor-associated antigen-positive tumor cells or tumor cells expressing ligands for NK cell receptors. Indeed, clinical trials have shown that CAR-T cells cannot eradicate tumor cells that are highly heterogeneous23, whereas CAR-modified NK cells may be able to efficiently eradicate residual tumor cells that may change their phenotypes after long-term treatment.
Finally, NK cells are abundant in clinical specimens and can be generated from PB, UCB, hESCs, iPCSs, and even NK-92 cell lines. NK-92 cells provide a homogeneous cell population and can be easily expanded under good manufacturing practice standards for broader clinical applications24, enabling the “off-the-shelf” production of CAR-modified NK-92 cells. However, they must be irradiated prior to infusion due to their tumor cell line origin. Activated PB-NK cells express a wider range of activating receptors and can be administered without irradiation, which allows them to expand in vivo. NK cells derived from iPSCs or hESCs combine the advantages of PB-NK and NK-92 cells since they exhibit a phenotype similar to that of PB-NK cells and are a homogeneous population. Importantly, CARs are easily expressed in hESC- and/or iPSC-derived NK cells using nonviral gene transfer methods25.
Current progress in the use of CAR-NK cells, from investigation to clinical trials
A suitable CAR structure is important for activating CAR-transduced cells. The majority of CAR-NK cells used the first generation of CAR constructs that contain CD3ζ as an intracellular signaling domain or the second generation of CAR constructs that express a second signaling domain (eg, CD28, 4-1BB) in conjunction with CD3ζ (Figure 1). In general, the second generation of CARs in NK cells is more active than first-generation CARs. Some studies have designed CAR constructs based on the activating features of NK cells. For example, DNAX-activation protein 12 (DAP12) and DAP10 have been selected as intracellular signaling domains, and CD3ζ appears to be a better signaling domain than DAP1015, whereas DAP12 may better activate signaling than CD3ζ for NK cells26. For second-generation CARs, the important co-stimulatory molecule 4-1-BB combines with CD3ζ as an intracellular domain, which significantly enhances the targeted lysis of CAR-NK cells27,28,29. However, the combination of CAR constructs for optimal NK cell activation may depend on the tumor type or target antigen27. Based on the importance of the NK cell-activating receptor NKG2D for NK cell activity and the common overexpression of NKG2D ligands on various tumors, a unique CAR construct that contains NKG2D as the ectodomain and links DAP10 and CD3ζ as key signaling molecules has been developed. These CAR-expressing NK cells exhibited enhanced cytotoxicity against a wide spectrum of tumor subtypes, with the best responses observed in ALL, osteosarcoma, prostate carcinoma, and rhabdomyosarcoma30.
Basic principle of CAR-NK cells. Chimeric antigen receptors contain an antigen-recognition domain (eg, ScFv or NKG2D), a transmembrane domain and a signaling domain that provides a signal to activate NK cells. First-generation CARs only contain CD3ζ or DAP12 as the signaling domain, and CD3ζ appears to be a better signaling domain than DAP10, whereas DAP12 may activate NK cells better than CD3ζ. In contrast, second-generation CARs express a second signaling domain (eg, CD28 or 4-1BB) in conjunction with CD3ζ. Third-generation CARs contain two co-stimulatory signaling domains. Based on the mechanisms by which NKG2D activates NK cells, a unique CAR construct containing NKG2D as the ectodomain that links DAP10 and CD3ζ as key signaling molecules was developed. The clustering of CARs induced by antigen binding or NKG2D and its ligand ligation initiates signal transduction that leads to NK cell activation, cytotoxicity against cancer cells, cytokine production, survival and proliferation.
The safety and efficacy of CAR-NK cells are usually evaluated in NSG or NOG (NOD/scid/IL-2Rγnull) mice, which lack nearly all types of immune cells. To this end, tumor cell line- or patient-derived tumor xenografts (PDX) are engrafted into NSG or NOG mice to establish the human tumor model31. The cell line-derived tumor xenografts models are simple to handle but cannot capture the heterogeneity of the original tumor. The PDX model, which is established by transferring of primary tumors directly from the patient into an immunodeficient mouse, can retain the heterogeneity of primary tumor samples and more closely resembles the original clinical cancer than long-established cell lines and standard xenografts; thus, this model has emerged as a powerful tool for studying tumor xenografts32. Most CAR-NK cells are transferred to the PDX model to evaluate their safety and efficacy in pre-clinical trials, including CAR-targeting antigens from hematological cancers (eg, CD19, CD20, CD138, and CS-1)33,34,35,36,37,38 and solid tumors (eg, HER2, EpCam, GD2, GPA7, PSCA, EGFR and EGFRvIII)14,26,39,40,41,42,43,44,45,46 (Table 1).
However, the deficient immune systems of NSG and NOG mice preclude observing changes in the immune system49, the interaction of immune cells and tumor cells, and, importantly, the influences of CAR-NK or CAR-T therapy on host immune cells in the tumor microenvironment. Humanized mice, which develop a functional human immune system due to the transplantation of human hematopoietic stem cells into immunodeficient mice, are used to narrow the gap of the tumor microenvironment50. To date, humanized mice have been used to evaluate the safety and efficacy of some CAR-T cell therapies. For example, a CD44v6-targeted CAR-T cells were transferred into hematopoietic reconstituted NSG xenograft mice to evaluate the on-target/off-tumor toxicities on normal hematopoietic stem cells51. A new combination immunotherapy that consists of human anti-carbonic anhydrase IX (CAIX)-targeted CAR-T cells engineered to secrete human anti-programmed death ligand 1 (PD-L1) antibodies was evaluated with a humanized mouse model to observe the effect on the reversal of T cell exhaustion and the promotion of NK cell recruitment to tumor sites52. Overall, humanized mice are a more precise model for preclinical trials of CAR-based immunotherapy.
Despite numerous clinical trials on CAR-T cells, only a few clinical trials that examine CAR-transduced NK cells are ongoing, including CAR-modified NK-92 and primary NK cells (Table 1). Four clinical studies sponsored by PersonGen BioTherapeutics (Suzhou, China) aim to evaluate the safety and efficacy of CAR-modified NK-92 cells for patients with relapsed or refractory malignancies, including leukemia, lymphoma and solid tumors. The targets for lymphoma and leukemia include CD19, CD7 and CD33, whereas MUC1 is targeted for relapsed or refractory solid tumors, including hepatocellular carcinoma, non-small cell lung cancer, pancreatic carcinoma, triple-negative invasive breast carcinoma, malignant glioma of brain, colorectal carcinoma, and gastric carcinoma. Although the NK-92 cell line has successfully entered into clinical trials, its clinical application is limited by a poor safety profile and poor in vivo expansion and persistence because this cell line must be irradiated prior to infusion and expresses fewer natural NK cell receptors.
Three clinical trials focus on human primary NK cells that express CD19-specific CAR for the treatment of B-lineage ALL. The first trial (NCT00995137) was conducted at St Jude Children's Research Hospital, and phase I has been completed. In this trial, irradiated K562 cells line to express membrane-bound IL-15 and 4-1BB ligand (K562-mb15-41BBL) were used as feeder cells to promote the expansion of donor NK cells prior to the transduction of a CD19-targeted CAR (anti-CD19-BB-zeta). The second clinical trial (NCT01974479) used a similar method to expand NK cells. Specifically, primary NK cells were transfected with anti-CD19-BB-zeta mRNA to construct CD19-targeted CAR-NK cells. The third trial (NCT03056339) employed iC9/CAR.19/IL15-transduced UCB-derived NK cells and was sponsored by the MD Anderson Cancer Center. CAR containing CD28/CD3ζ as a signaling domain, inducible caspase-9 (iCasp9) as a suicide gene, and IL-15 as an activating cytokine was transduced into UCB-derived NK cells. This phase I/II trial was recently approved for B-lymphoid malignancies in 2017.
Challenges to the clinical applications of CAR-NK cells
Ex vivo expansion of primary CAR-NK cells
The foremost challenge to the clinical application of CAR-NK cells is the ex vivo expansion of CAR-modified primary NK cells. In recent years, the purification/expansion of clinical-grade NK cells has mainly focused on their generation from PB, cord blood and embryonic stem cells53. Although the expansion of clinical-grade primary NK cells by coculture with irradiated K562-mb15-4-1BBL cells as feeder cells is practical54, reservations regarding residual feeder cells in the final NK product persist. In a clinical trial of adoptive transferring donor-derived IL-15/4-1BBL-activated NK cells (aNK-DLI), which were cocultured with recombinant human IL-15 plus 4-1BBL+IL-15Rα+ K562 cells as feeder cells, grade 4 GVHD was observed in three patients55. Because aNK-DLI were HLA-matched and T cells were depleted, which poses a low risk of severe GVHD, the utilization of feeder cells may be responsible for the observed GVHD.
The expansion of human NK cells in feeder-free conditions, such as the expansion of primary NK cells from PBMCs with cytokines (IL-2 or in combination with IL-15 or anti-CD3 mAb)56, is currently feasible and safer than expansion with feeders. Because PBMCs contain low levels of NK cells ranging from 5%–20%, Koehl et al expanded NK cells from purified CD56 cells using immunomagnetic beads, and these cells were subsequently activated in vitro by IL-2 for 12 d. This approach resulted in a median number of 7.59×108 CD56+CD3− cells that exhibited both a purity and viability of 94%57. However, the amount of NK cells expanded from purified CD56+ cells is limited and not sufficient for CAR-NK cell therapy. Thus, Sutlu et al expanded NK cells directly from PBMCs without any separation strategies, which resulted in a mean of 9.8×109 NK cells are obtained after 21 d, but the purity of these cells was only 38%58. Recently, Masuyama et al reported a new method to obtain high-purity NK cells59. Specifically, PBMCs are co-stimulated with anti-CD3 and anti-CD52 monoclonal antibodies and cultured for 14 d in NKGM-1 medium with autologous plasma and IL-2. Using this approach, purity of NK cells is approximately 60% after 7 d of culture, and this purity is much higher in continued culture. A median of 5.7×109 NK cells are generated from 20 mL of PB (approximately 646-fold increase) after 14 d of culture. Recent studies have shown that a brief pre-activation with IL-12, IL-15, and IL-18 followed by successive stimulation and expansion with these cytokines induces memory-like NK cells that display a longer life span in vivo5. These memory-like NK cells exhibited enhanced IFN-γ production and cytotoxicity as well as good clinical responses after adoptively transfer6; thus, this approach shows great promise for NK cell expansion. In the future, the choice of expanding naïve NK cells or memory-like NK cells needs to be based on clinical responses.
Spanholtz et al developed a cytokine-based method without supportive feeders for the expansion of human NK cells from UCB60. Specifically, they used a two-step in vitro differentiation scheme using a novel clinical grade medium that contained different cytokine combinations (including SCF, IL-7, Flt3L, TPO, IL-15, G-CSF, GM-CSF, IL-6, IL-2, etc) to generate a high purity of expanded CD56+NK cells from CD34+ UCB cells ex vivo. The mean expansion was greater than 15 000-fold, and the purity was nearly 100%. Importantly, UCB-derived NK cells generated with this method exhibit a powerful function; they can efficiently target myeloid leukemia and melanoma cell lines. Thus, this method is ideal and practical if the restrictions in using UCB as a source could be overcome. A UCB-derived CAR-NK cell therapy for B lymphoid malignancies (sponsored by MD Anderson Cancer Center) has recently been approved for clinical trial (NCT03056339).
The clinical-scale derivation of NK cells from hESCs or iPSCs is based on a two-stage culture system that utilizes a recombinant protein-based, animal product-free medium in a xenogeneic stromal cells-free manner61. Briefly, the undifferentiated hESCs and iPSCs are first supported to produce hematopoietic progenitor cells using a “spin embryoid bodies (EBs)” method for 11 d62; without dissociation of sorting, the spin EBs are then directly transferred into defined conditions containing cytokines (IL-3, IL-7, IL-15, SCF and Flt3L) without exogenous stromal cells and cultured for 28–35 d. The utilization of hESCs or iPSCs may avoid restrictions associated with using UCB as a source, but problems persist, such as the selection of an optimal cell line (hESCs or iPSCs) for the expansion of NK cells and the development of self-tolerance in NK cells from UCB, hESCs or iPSCs63.
Methods for CAR transduction into NK cells
Another pressing obstacle is the selection of a suitable transduction method for NK cells that express CARs. Two types of transduction methods have been applied to introduce CARs: viral vectors and non-viral vectors.
For viral vectors, retrovirus- or lentivirus-based vectors have been mostly applied to genetically engineer primary CAR-NK cells due to their stable integration into the genome. The transduction efficacy of retroviral vectors is very high in expanded primary NK cells, ie, a median of 69% (43%–93%)15, but this method is associated with a risk for insertional mutagenesis, oncogenesis, or sustained and uncontrolled adverse events due to stable transgene expression. For example, a report shows that four of nine patients who received retrovirus-mediated gene therapy developed T cell leukemia64. Lentiviral vectors have moderate levels of insertion mutations, but their lentiviral transduction efficiency is very low for PB-derived NK cells (between 8%–16%). However, the transduction efficiency of cord blood-derived NK cells reaches 73%65, which is sufficient to introduce CARs into cord blood-derived NK cells. Nevertheless, the lentiviral transduction efficiency of PB-derived NK cells requires improvement.
Due to the high-risk of insertion mutations and the high cost of viral vectors for clinical therapy, non-viral vectors have garnered increasing attention. Non-viral vectors, such as naked DNA, have some advantages, eg, they are inexpensive and low immunogenicity, but cannot they integrate transgenes into the genome. The non-viral Sleeping Beauty (SB) transposon system is an alternative gene transfer system that combines the advantages of viral and non-viral vectors since they mediate stable transgene expression. The SB transposon system transfers genes via a bi-component vector system that consists of a transposon containing a gene of interest (eg, CAR) flanked by inverted terminal repeats and a transposase (eg, SB100X) that binds to the inverted terminal repeats and “cuts-and-pastes” the transposon for integration into the genome. Several groups have successfully applied the SB transposon system to CAR transgenes in T cells using electroporation66,67,68. Phase I trials have been sponsored that use SB to generate CD19-specific CAR-T cells for the treatment of patients with advanced non-Hodgkin's lymphoma and acute lymphoblastic leukemia who underwent HSCT and CAR-T cell infusion as adjuvant therapy in the autologous or allogeneic settings. The results identified 84% CAR expression without integration hotspots68. Importantly, the respective 30-month progression-free and overall survival rates were 83% and 100% following autologous HSCT, and the respective 12-month rates were 53% and 63% after allogeneic HSCT. However, due to the low transfection efficiency and severe cytotoxicity of electroporation DNA vectors to primary NK cells, the applicability of the SB transposon system to transduce CAR transgenes into primary NK cells remains unknown. Nevertheless, the SB transposon system has been proven to mediate gene transfer in cord blood-derived hematopoietic stem and progenitor cells69, and the SB-based anti-CD19 CAR transgene has been successfully tested in a follow-up study70. Therefore, it may be feasible to expand CAR-NK cells from UCB hematopoietic stem and progenitor cells and then genetically transfer CARs using the SB transposon system.
The transfection of mRNA that encodes a CAR using electroporation has been tested in human primary NK cells. The electroporation of mRNA is a safe, cost-effective and efficient to transiently express CARs. Shimasaki et al showed that 61.3% of cells expressed anti-CD19 CAR, and the viability of expanded NK cells reached 90% 24 h after the electroporation of mRNA71. Remarkably, mRNA electroporation is associated with transfection efficiencies of 80%–90% not only in ex vivo-expanded cells but also in primary resting (non-cytokine activated) human NK cells72. However, due to the transient expression of CARs transferred by mRNA electroporation (up to 3 d), anti-tumor effects may also be transient72, and CAR-NK cells prepared by electroporation mRNA might be more suitable as an adjuvant therapy to rapidly reduce tumor cell burden.
Strategies to improve the safety and efficacy of CAR-NK cells
Improvements in safety
In recent years, many technologies have been studied to improve the safety and therapeutic efficacy of CAR-targeted cell therapy. Most technologies have been proven efficacious in T cells but can be easily transferred to CAR-NK cells, including the selection of safer antigens, masked CAR, oxygen-sensitive CAR and synthetic Notch (synNotch) receptors.
Many CAR-targeted antigens are expressed not only on the surface of tumor cells but also in healthy tissues. In 2010, a patient with HER2-positive metastatic colon cancer died after a high dose of HER2-specific CAR-T cell therapy due to the release of cytokines by lung epithelial cells that expressed low levels of HER273. Therefore, tumor-specific CAR targets need to be selected. Posey et al reported a CAR that targets an abnormal glycoform of MUC1, Tn-MUC1, which is specifically expressed by multiple types of tumors but not on the cellular surface of normal human tissues74. Thus, this approach allowed the selection of aberrantly glycosylated antigens and constitutes a safer alternative to tumor-associated antigens for CAR-based therapy.
Several technologies have been explored to ensure that CARs are active only at local tumor sites. For example, a masked CAR consists of a masking peptide that blocks the antigen-binding site and a protease-sensitive linker75. Proteases that are commonly active in the tumor microenvironment can cleave the linker and disengage the masking peptide, thereby enabling CARs to be functional at the local tumor sites. An oxygen-sensitive CAR designed by fusing an oxygen-sensitive subdomain of HIF1α to a CAR scaffold generated CAR-T cells that are responsive to a hypoxic environment, a hallmark of certain tumors, which allows the CAR-T cells to only be effective at local tumor sites76. Indeed, in vitro models showed that the CAR surface expression and cytolysis of CAR-T cells were controlled by the oxygen concentration.
Two recent papers reported taking advantage of the synNotch system to spatially control CAR-T cell activation via combinatorial antigen recognition77,78. In other words, a T cell would only be activated when both the synNotch ligand and the CAR ligand were simultaneously expressed on a target cell. This strategy provides precise therapeutic discrimination single antigen "bystander" cells while efficiently clearing combinatorial antigen-positive tumors78. It is a powerful platform to engineer T or NK cells and provide customized therapy at local tumor sites to obtain more effective and safer CAR-T or CAR-NK cell therapies for a wider range of tumor types. Nevertheless, many problems persist for the use of this system in clinical therapy. For instance, a dose/response relationship between the ligand concentration and receptor activation has not yet been reported. Moreover, the strength, duration, and specificity of the synNotch system as well as the kinetics of CAR expression and function need to be clarified.
Improvements in the anti-tumor effects of CAR-NK cells
The production of inhibitory cytokines, high expression of ligands for co-inhibitory receptors (eg, PD-1, NKG2A, and TIM-3) on tumor cells, and high frequency of regulatory T cells or MDSCs in the tumor microenvironment are important immune-escape mechanisms79,80,81,82,83 that limit CAR-T or NK cell persistence and function. Thus, the introduction of a CAR while simultaneously silencing NK cell inhibitory receptors (such as NKG2A or TIM-3) may improve the efficacy of CAR-NK cells. To protect CAR-T cells from impairment by the immunosuppressive cytokine IL-4 in the tumor environment, an inverted cytokine receptor (ICR) in which the IL-4 receptor exodomain is fused to the IL-7 receptor endodomain (4/7 ICR) has been transgenically expressed in PSCA-targeted CAR-T cells84. This 4/7 ICR attenuated inhibition by tumor-derived IL-4 and instead promoted T cell proliferation. Moreover, in vivo experiments showed that CAR/ICR-transduced cells induced potent and sustained anti-tumor effects in an IL-4-rich tumor microenvironment. A similar modification strategy may also apply to CAR-NK cells, although the endodomain of ICR, such as the IL-15, IL-18 or IL-21 receptor, that is more suitable for NK cells remains to be identified.
Recently, the CRISPR/Cas9 system has rapidly become a popular tool for targeted gene integration. Due to its advantages in inducing permanent modifications at specific sites of the genome via double-strand breaks, the CRISPR/Cas9 system can be used to integrate CAR genes at specific sites via homology-directed recombination instead of random integration. A recent study has shown that knocking-in a CAR at the T cell receptor α constant locus with CRISPR/Cas9 increased tumor rejection85. Notably, targeting the CAR to the TRAC locus averts tonic CAR signaling and establishes the effective internalization and re-expression of the CAR following a single or repeated exposure to antigen, which delays effector T cell differentiation and exhaustion. Similarly, the CRISPR/Cas9 system could be used to produce stably transduced NK cells via the gene editing of primary NK cells, which might efficiently improve both the efficacy and safety of CAR-NK cells.
Conclusion and perspectives
In addition to the numerous clinical studies of CAR-T cells, various CAR-NK cell clinical trials have recently been carried out in 2016 and 2017. The advantages of CAR-expressing NK cells compared to CAR-T cells hold great promise for application in cellular immunotherapy against refractory malignancies. However, questions remain to be answered. For example, although many strategies and technologies have been presented to improve therapeutic efficacy, the outcomes of CAR-NK cell immunotherapy remain unpredictable, especially in solid tumors. Due to the heterogeneity of NK cells, which contain different NK subsets with different functional features86,87,88,89, the need to select suitable NK cell subsets (eg, killer subpopulation) to selectively expand and construct specific CAR-NK cells is yet to be explored. Are naïve or memory-like NK cells better for expansion and transduction? Due to their short in vivo lifespan, NK cells likely cannot induce cytokine storms or on-target/off-tumor effects, but their short persistence in vivo likely limits their cytolytic efficacy against tumors. Furthermore, the best structure of CARs to improve the proliferation, activation, cytokine secretion and cytolytic activity of NK cells has not yet been identified. Nevertheless, given the recent advances and rapid developments in clinically compliant techniques to expand and genetically manipulate NK cells, CAR-NK cell-based immunotherapy likely constitutes a promising prospect for cancer therapy.
References
Rey J, Veuillen C, Vey N, Bouabdallah R, Olive D . Natural killer and gammadelta T cells in haematological malignancies: enhancing the immune effectors. Trends Mol Med 2009; 15: 275–84.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 2002; 295: 2097–100.
Brehm C, Huenecke S, Esser R, Kloess S, Quaiser A, Betz S, et al. Interleukin-2-stimulated natural killer cells are less susceptible to mycophenolate mofetil than non-activated NK cells: possible consequences for immunotherapy. Cancer Immunol Immunother 2014; 63: 821–33.
Brehm C, Huenecke S, Quaiser A, Esser R, Bremm M, Kloess S, et al. IL-2 stimulated but not unstimulated NK cells induce selective disappearance of peripheral blood cells: concomitant results to a phase I/II study. PLoS One 2011; 6: e27351.
Romee R, Schneider SE, Leong JW, Chase JM, Keppel CR, Sullivan RP, et al. Cytokine activation induces human memory-like NK cells. Blood 2012; 120: 4751–60.
Romee R, Rosario M, Berrien-Elliott MM, Wagner JA, Jewell BA, Schappe T, et al. Cytokine-induced memory-like natural killer cells exhibit enhanced responses against myeloid leukemia. Sci Transl Med 2016; 8: 357ra123.
Perez-Martinez A, Fernandez L, Valentin J, Martinez-Romera I, Corral MD, Ramirez M, et al. A phase I/II trial of interleukin-15–stimulated natural killer cell infusion after haplo-identical stem cell transplantation for pediatric refractory solid tumors. Cytotherapy 2015; 17: 1594–603.
Maude SL, Teachey DT, Porter DL, Grupp SA . CD19-targeted chimeric antigen receptor T-cell therapy for acute lymphoblastic leukemia. Blood 2015; 125: 4017–23.
Ahmed N, Brawley VS, Hegde M, Robertson C, Ghazi A, Gerken C, et al. Human epidermal growth factor receptor 2 (HER2)–specific chimeric antigen receptor-modified T cells for the immunotherapy of HER2-positive sarcoma. J Clin Oncol 2015; 33: 1688–96.
Katz SC, Burga RA, McCormack E, Wang LJ, Mooring W, Point GR, et al. Phase I hepatic immunotherapy for metastases study of intra-arterial chimeric antigen receptor-modified T-cell therapy for CEA+ liver metastases. Clin Cancer Res 2015; 21: 3149–59.
Feng K, Guo Y, Dai H, Wang Y, Li X, Jia H, et al. Chimeric antigen receptor-modified T cells for the immunotherapy of patients with EGFR-expressing advanced relapsed/refractory non-small cell lung cancer. Sci China Life Sci 2016; 59: 468–79.
Kalaitsidou M, Kueberuwa G, Schutt A, Gilham DE . CAR T-cell therapy: toxicity and the relevance of preclinical models. Immunotherapy 2015; 7: 487–97.
Cheng Q, Ma S, Lin D, Mei Y, Gong H, Lei L, et al. The S1P1 receptor-selective agonist CYM-5442 reduces the severity of acute GVHD by inhibiting macrophage recruitment. Cell Mol Immunol 2015; 12: 681–91.
Uherek C, Tonn T, Uherek B, Becker S, Schnierle B, Klingemann HG, et al. Retargeting of natural killer-cell cytolytic activity to ErbB2-expressing cancer cells results in efficient and selective tumor cell destruction. Blood 2002; 100: 1265–73.
Imai C, Iwamoto S, Campana D . Genetic modification of primary natural killer cells overcomes inhibitory signals and induces specific killing of leukemic cells. Blood 2005; 106: 376–83.
Klingemann H . Are natural killer cells superior CAR drivers? Oncoimmunology 2014; 3: e28147.
Miller JS, Soignier Y, Panoskaltsis-Mortari A, McNearney SA, Yun GH, Fautsch SK, et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood 2005; 105: 3051–7.
Rubnitz JE, Inaba H, Ribeiro RC, Pounds S, Rooney B, Bell T, et al. NKAML: a pilot study to determine the safety and feasibility of haploidentical natural killer cell transplantation in childhood acute myeloid leukemia. J Clin Oncol 2010; 28: 955–9.
Shaffer BC, Le Luduec JB, Forlenza C, Jakubowski AA, Perales MA, Young JW, et al. Phase II study of haploidentical natural killer cell infusion for treatment of relapsed or persistent myeloid malignancies following allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2016; 22: 705–9.
Kalos M, Levine BL, Porter DL, Katz S, Grupp SA, Bagg A, et al. T cells with chimeric antigen receptors have potent antitumor effects and can establish memory in patients with advanced leukemia. Sci Transl Med 2011; 3: 95ra73.
Sun C, Sun H, Zhang C, Tian Z . NK cell receptor imbalance and NK cell dysfunction in HBV infection and hepatocellular carcinoma. Cell Mol Immunol 2015; 12: 292–302.
Sun C, Sun HY, Xiao WH, Zhang C, Tian ZG . Natural killer cell dysfunction in hepatocellular carcinoma and NK cell-based immunotherapy. Acta Pharmacol Sin 2015; 36: 1191–9.
Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med 2014; 371: 1507–17.
Tam YK, Martinson JA, Doligosa K, Klingemann HG . Ex vivo expansion of the highly cytotoxic human natural killer-92 cell-line under current good manufacturing practice conditions for clinical adoptive cellular immunotherapy. Cytotherapy 2003; 5: 259–72.
Ni Z, Knorr DA, Bendzick L, Allred J, Kaufman DS . Expression of chimeric receptor CD4zeta by natural killer cells derived from human pluripotent stem cells improves in vitro activity but does not enhance suppression of HIV infection in vivo. Stem Cells 2014; 32: 1021–31.
Topfer K, Cartellieri M, Michen S, Wiedemuth R, Muller N, Lindemann D, et al. DAP12-based activating chimeric antigen receptor for NK cell tumor immunotherapy. J Immunol 2015; 194: 3201–12.
Hermanson DL, Kaufman DS . Utilizing chimeric antigen receptors to direct natural killer cell activity. Front Immunol 2015; 6: 195.
Wang R, Freywald A, Chen Y, Xu J, Tan X, Xiang J . Transgenic 4-1BBL-engineered vaccine stimulates potent Gag-specific therapeutic and long-term immunity via increased priming of CD44+CD62L(high) IL-7R+ CTLs with up- and downregulation of anti- and pro-apoptosis genes. Cell Mol Immunol 2015; 12: 456–65.
Rahman K, Iyer SS . Costimulatory molecules as vaccine adjuvants: to 4-1BB or not to 4-1BB? Cell Mol Immunol 2015; 12: 508–9.
Chang YH, Connolly J, Shimasaki N, Mimura K, Kono K, Campana D . A chimeric receptor with NKG2D specificity enhances natural killer cell activation and killing of tumor cells. Cancer Res 2013; 73: 1777–86.
Zhou Q, Facciponte J, Jin M, Shen Q, Lin Q . Humanized NOD-SCID IL2rg−/− mice as a preclinical model for cancer research and its potential use for individualized cancer therapies. Cancer Lett 2014; 344: 13–9.
Cassidy JW, Caldas C, Bruna A . Maintaining tumor heterogeneity in patient-derived tumor xenografts. Cancer Res 2015; 75: 2963–8.
Oelsner S, Friede ME, Zhang C, Wagner J, Badura S, Bader P, et al. Continuously expanding CAR NK-92 cells display selective cytotoxicity against B-cell leukemia and lymphoma. Cytotherapy 2017; 19: 235–49.
Romanski A, Uherek C, Bug G, Seifried E, Klingemann H, Wels WS, et al. CD19-CAR engineered NK-92 cells are sufficient to overcome NK cell resistance in B-cell malignancies. J Cell Mol Med 2016; 20: 1287–94.
Oelsner S, Wagner J, Friede ME, Pfirrmann V, Genssler S, Rettinger E, et al. Chimeric antigen receptor-engineered cytokine-induced killer cells overcome treatment resistance of pre-B-cell acute lymphoblastic leukemia and enhance survival. Int J Cancer 2016; 139: 1799–809.
Muller T, Uherek C, Maki G, Chow KU, Schimpf A, Klingemann HG, et al. Expression of a CD20-specific chimeric antigen receptor enhances cytotoxic activity of NK cells and overcomes NK-resistance of lymphoma and leukemia cells. Cancer Immunol Immunother 2008; 57: 411–23.
Jiang H, Zhang W, Shang P, Zhang H, Fu W, Ye F, et al. Transfection of chimeric anti-CD138 gene enhances natural killer cell activation and killing of multiple myeloma cells. Mol Oncol 2014; 8: 297–310.
Chu J, Deng Y, Benson DM, He S, Hughes T, Zhang J, et al. CS1-specific chimeric antigen receptor (CAR)-engineered natural killer cells enhance in vitro and in vivo antitumor activity against human multiple myeloma. Leukemia 2014; 28: 917–27.
Zhang C, Burger MC, Jennewein L, Genssler S, Schonfeld K, Zeiner P, et al. ErbB2/HER2-specific NK cells for targeted therapy of glioblastoma. J Natl Cancer Inst 2016; 108. doi:10.1093/jnci/djv375.
Liu H, Yang B, Sun T, Lin L, Hu Y, Deng M, et al. Specific growth inhibition of ErbB2-expressing human breast cancer cells by genetically modified NK92 cells. Oncol Rep 2015; 33: 95–102.
Sahm C, Schonfeld K, Wels WS . Expression of IL-15 in NK cells results in rapid enrichment and selective cytotoxicity of gene-modified effectors that carry a tumor-specific antigen receptor. Cancer Immunol Immunother 2012; 61: 1451–61.
Kailayangiri S, Altvater B, Spurny C, Jamitzky S, Schelhaas S, Jacobs AH, et al. Targeting Ewing sarcoma with activated and GD2-specific chimeric antigen receptor-engineered human NK cells induces upregulation of immune-inhibitory HLA-G. Oncoimmunology 2017; 6: e1250050.
Zhang G, Liu R, Zhu X, Wang L, Ma J, Han H, et al. Retargeting NK-92 for anti-melanoma activity by a TCR-like single-domain antibody. Immunol Cell Biol 2013; 91: 615–24.
Han J, Chu J, Keung Chan W, Zhang J, Wang Y, Cohen JB, et al. CAR-engineered NK cells targeting wild-type EGFR and EGFRvIII enhance killing of glioblastoma and patient-derived glioblastoma stem cells. Sci Rep 2015; 5: 11483.
Chen X, Han J, Chu J, Zhang L, Zhang J, Chen C, et al. A combinational therapy of EGFR-CAR NK cells and oncolytic herpes simplex virus 1 for breast cancer brain metastases. Oncotarget 2016; 7: 27764–77.
Muller N, Michen S, Tietze S, Topfer K, Schulte A, Lamszus K, et al. Engineering NK cells modified with an EGFRvIII-specific chimeric antigen receptor to overexpress CXCR4 improves immunotherapy of CXCL12/SDF-1alpha-secreting glioblastoma. J Immunother 2015; 38: 197–210.
Schirrmann T, Pecher G . Specific targeting of CD33+ leukemia cells by a natural killer cell line modified with a chimeric receptor. Leuk Res 2005; 29: 301–6.
Esser R, Muller T, Stefes D, Kloess S, Seidel D, Gillies SD, et al. NK cells engineered to express a GD2-specific antigen receptor display built-in ADCC-like activity against tumour cells of neuroectodermal origin. J Cell Mol Med 2012; 16: 569–81.
Diehl R, Ferrara F, Muller C, Dreyer AY, McLeod DD, Fricke S, et al. Immunosuppression for in vivo research: state-of-the-art protocols and experimental approaches. Cell Mol Immunol 2017; 14: 146–79.
Morton JJ, Bird G, Refaeli Y, Jimeno A . Humanized mouse xenograft models: narrowing the tumor-microenvironment gap. Cancer Res 2016; 76: 6153–8.
Casucci M, Nicolis di Robilant B, Falcone L, Camisa B, Norelli M, Genovese P, et al. CD44v6-targeted T cells mediate potent antitumor effects against acute myeloid leukemia and multiple myeloma. Blood 2013; 122: 3461–72.
Suarez ER, Chang de K, Sun J, Sui J, Freeman GJ, Signoretti S, et al. Chimeric antigen receptor T cells secreting anti-PD-L1 antibodies more effectively regress renal cell carcinoma in a humanized mouse model. Oncotarget 2016; 7: 34341–55.
Cheng M, Chen Y, Xiao W, Sun R, Tian Z . NK cell-based immuno-therapy for malignant diseases. Cell Mol Immunol 2013; 10: 230–52.
Lapteva N, Durett AG, Sun J, Rollins LA, Huye LL, Fang J, et al. Large-scale ex vivo expansion and characterization of natural killer cells for clinical applications. Cytotherapy 2012; 14: 1131–43.
Shah NN, Baird K, Delbrook CP, Fleisher TA, Kohler ME, Rampertaap S, et al. Acute GVHD in patients receiving IL-15/4-1BBL activated NK cells following T-cell-depleted stem cell transplantation. Blood 2015; 125: 784–92.
Shimasaki N, Coustan-Smith E, Kamiya T, Campana D . Expanded and armed natural killer cells for cancer treatment. Cytotherapy 2016; 18: 1422–34.
Koehl U, Brehm C, Huenecke S, Zimmermann SY, Kloess S, Bremm M, et al. Clinical grade purification and expansion of NK cell products for an optimized manufacturing protocol. Front Oncol 2013; 3: 118.
Sutlu T, Stellan B, Gilljam M, Quezada HC, Nahi H, Gahrton G, et al. Clinical-grade, large-scale, feeder-free expansion of highly active human natural killer cells for adoptive immunotherapy using an automated bioreactor. Cytotherapy 2010; 12: 1044–55.
Masuyama J, Murakami T, Iwamoto S, Fujita S . Ex vivo expansion of natural killer cells from human peripheral blood mononuclear cells co-stimulated with anti-CD3 and anti-CD52 monoclonal antibodies. Cytotherapy 2016; 18: 80–90.
Spanholtz J, Tordoir M, Eissens D, Preijers F, van der Meer A, Joosten I, et al. High log-scale expansion of functional human natural killer cells from umbilical cord blood CD34-positive cells for adoptive cancer immunotherapy. PLoS One 2010; 5: e9221.
Knorr DA, Ni Z, Hermanson D, Hexum MK, Bendzick L, Cooper LJ, et al. Clinical-scale derivation of natural killer cells from human pluripotent stem cells for cancer therapy. Stem Cells Transl Med 2013; 2: 274–83.
Ng ES, Davis R, Stanley EG, Elefanty AG . A protocol describing the use of a recombinant protein-based, animal product-free medium (APEL) for human embryonic stem cell differentiation as spin embryoid bodies. Nat Protoc 2008; 3: 768–76.
He Y, Tian Z . NK cell education via nonclassical MHC and non-MHC ligands. Cell Mol Immunol 2017; 14: 321–30.
Hacein-Bey-Abina S, Garrigue A, Wang GP, Soulier J, Lim A, Morillon E, et al. Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J Clin Invest 2008; 118: 3132–42.
Boissel L, Betancur M, Lu W, Wels WS, Marino T, Van Etten RA, et al. Comparison of mRNA and lentiviral based transfection of natural killer cells with chimeric antigen receptors recognizing lymphoid antigens. Leuk Lymphoma 2012; 53: 958–65.
Monjezi R, Miskey C, Gogishvili T, Schleef M, Schmeer M, Einsele H, et al. Enhanced CAR T-cell engineering using non-viral Sleeping Beauty transposition from minicircle vectors. Leukemia 2017; 31: 186–94.
Thokala R, Olivares S, Mi T, Maiti S, Deniger D, Huls H, et al. Redirecting specificity of T cells using the Sleeping Beauty system to express chimeric antigen receptors by mix-and-matching of VL and VH domains targeting CD123+ tumors. PLoS One 2016; 11: e0159477.
Kebriaei P, Singh H, Huls MH, Figliola MJ, Bassett R, Olivares S, et al. Phase I trials using Sleeping Beauty to generate CD19-specific CAR T cells. J Clin Invest 2016; 126: 3363–76.
Xue X, Huang X, Nodland SE, Mates L, Ma L, Izsvak Z, et al. Stable gene transfer and expression in cord blood-derived CD34+ hematopoietic stem and progenitor cells by a hyperactive Sleeping Beauty transposon system. Blood 2009; 114: 1319–30.
Huls MH, Figliola MJ, Dawson MJ, Olivares S, Kebriaei P, Shpall EJ, et al. Clinical application of Sleeping Beauty and artificial antigen presenting cells to genetically modify T cells from peripheral and umbilical cord blood. J Vis Exp 2013: (72): e50070.
Shimasaki N, Fujisaki H, Cho D, Masselli M, Lockey T, Eldridge P, et al. A clinically adaptable method to enhance the cytotoxicity of natural killer cells against B-cell malignancies. Cytotherapy 2012; 14: 830–40.
Li L, Liu LN, Feller S, Allen C, Shivakumar R, Fratantoni J, et al. Expression of chimeric antigen receptors in natural killer cells with a regulatory-compliant non-viral method. Cancer Gene Ther 2010; 17: 147–54.
Morgan RA, Yang JC, Kitano M, Dudley ME, Laurencot CM, Rosenberg SA . Case report of a serious adverse event following the administration of T cells transduced with a chimeric antigen receptor recognizing ERBB2. Mol Ther 2010; 18: 843–51.
Posey AD Jr, Schwab RD, Boesteanu AC, Steentoft C, Mandel U, Engels B, et al. Engineered CAR T cells targeting the cancer-associated Tn-glycoform of the membrane mucin MUC1 control adenocarcinoma. Immunity 2016; 44: 1444–54.
Han X, Bryson PD, Zhao Y, Cinay GE, Li S, Guo Y, et al. Masked chimeric antigen receptor for tumor-specific activation. Mol Ther 2017; 25: 274–84.
Juillerat A, Marechal A, Filhol JM, Valogne Y, Valton J, Duclert A, et al. An oxygen sensitive self-decision making engineered CAR T-cell. Sci Rep 2017; 7: 39833.
Morsut L, Roybal KT, Xiong X, Gordley RM, Coyle SM, Thomson M, et al. Engineering customized cell sensing and response behaviors using synthetic notch receptors. Cell 2016; 164: 780–91.
Roybal KT, Rupp LJ, Morsut L, Walker WJ, McNally KA, Park JS, et al. Precision tumor recognition by T cells with combinatorial antigen-sensing circuits. Cell 2016; 164: 770–9.
Speiser DE, Ho PC, Verdeil G . Regulatory circuits of T cell function in cancer. Nat Rev Immunol 2016; 16: 599–611.
Mao Y, Yin S, Zhang J, Hu Y, Huang B, Cui L, et al. A new effect of IL-4 on human gammadelta T cells: promoting regulatory Vdelta1 T cells via IL-10 production and inhibiting function of Vdelta2 T cells. Cell Mol Immunol 2016; 13: 217–28.
Krneta T, Gillgrass A, Chew M, Ashkar AA . The breast tumor microenvironment alters the phenotype and function of natural killer cells. Cell Mol Immunol 2016; 13: 628–39.
Rekik R, Belhadj Hmida N, Ben Hmid A, Zamali I, Kammoun N, Ben Ahmed M . PD-1 induction through TCR activation is partially regulated by endogenous TGF-beta. Cell Mol Immunol 2015; 12: 648–9.
Zhang S, Ke X, Zeng S, Wu M, Lou J, Wu L, et al. Analysis of CD8+ Treg cells in patients with ovarian cancer: a possible mechanism for immune impairment. Cell Mol Immunol 2015; 12: 580–91.
Mohammed S, Sukumaran S, Bajgain P, Watanabe N, Heslop HE, Rooney CM, et al. Improving chimeric antigen receptor-modified T cell function by reversing the immunosuppressive tumor microenvironment of pancreatic cancer. Mol Ther 2017; 25: 249–58.
Eyquem J, Mansilla-Soto J, Giavridis T, van der Stegen SJ, Hamieh M, Cunanan KM, et al. Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature 2017; 543: 113–7.
Zhang QF, Yin WW, Xia Y, Yi YY, He QF, Wang X, et al. Liver-infiltrating CD11b-CD27- NK subsets account for NK-cell dysfunction in patients with hepatocellular carcinoma and are associated with tumor progression. Cell Mol Immunol 2016. doi: 10.1038/cmi.2016.28.
Peng H, Wisse E, Tian Z . Liver natural killer cells: subsets and roles in liver immunity. Cell Mol Immunol 2016; 13: 328–36.
Fu B, Tian Z, Wei H . Subsets of human natural killer cells and their regulatory effects. Immunology 2014; 141: 483–9.
Zhang C, Tian Z . NK cell subsets in autoimmune diseases. J Autoimmun 2017; 83: 22–30.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (91429303, 31390433, 31670908, 81472646, 81771686 and 91542000), the Ministry of Science & Technology of China (973 Basic Science Project 2013CB944901 and 2013CB944902) and the Chinese Academy of Science (XDA12020344).
Author information
Authors and Affiliations
Corresponding authors
PowerPoint slides
Rights and permissions
About this article
Cite this article
Hu, Y., Tian, Zg. & Zhang, C. Chimeric antigen receptor (CAR)-transduced natural killer cells in tumor immunotherapy. Acta Pharmacol Sin 39, 167–176 (2018). https://doi.org/10.1038/aps.2017.125
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2017.125
Keywords
This article is cited by
-
Co-expression of IL-21-Enhanced NKG2D CAR-NK cell therapy for lung cancer
BMC Cancer (2024)
-
Chimeric antigen receptor engineered natural killer cells for cancer therapy
Experimental Hematology & Oncology (2023)
-
Chimeric antigen receptor-natural killer cells: a promising sword against insidious tumor cells
Human Cell (2023)
-
The Role of NK Cells and Their Exosomes in Graft Versus Host Disease and Graft Versus Leukemia
Stem Cell Reviews and Reports (2023)
-
CAR-modified immune cells as a rapidly evolving approach in the context of cancer immunotherapies
Medical Oncology (2023)