Abstract
Aim:
Edaravone (3-methyl-1-phenyl-2-pyrazolin-5-one) is a free radical scavenger that has shown potent antioxidant, anti-inflammatory and neuroprotective effects in variety of disease models. In this study, we investigated whether edaravone produced neuroprotective actions in an infant mouse model of pneumococcal meningitis.
Methods:
C57BL/6 mice were infected on postnatal d 11 by intracisternal injection of a certain inoculum of Streptococcus pneumoniae. The mice received intracisternal injection of 10 μL of saline containing edaravone (3 mg/kg) once a day for 7 d. The severity of pneumococcal meningitis was assessed with a clinical score. In mice with severe meningitis, the survival rate from the time of infection to d 8 after infection was analyzed using Kaplan-Meier curves. In mice with mild meningitis, the CSF inflammation and cytokine levels in the hippocampus were analyzed d 7 after infection, and the clinical neurological deficit score was evaluated using a neurological scoring system d 14 after infection. The nuclear factor (erythroid-derived 2)-like 2 knockout (Nrf2 KO) mice and heme oxygenase-1 knockout (HO-1 KO) mice were used to confirm the involvement of Nrf2/HO-1 pathway in the neuroprotective actions of edaravone.
Results:
In mice with severe meningitis, edaravone treatment significantly increased the survival rate (76.4%) compared with the meningitis model group (32.2%). In mice with mild meningitis, edaravone treatment significantly decreased the number of leukocytes and TNF- levels in CSF, as well as the neuronal apoptosis and protein levels of HMGB1 and iNOS in the hippocampus, but did not affect the high levels of IL-10 and IL-6 in the hippocampus. Moreover, edaravone treatment significantly improved the neurological function of mice with mild meningitis. In Nrf2 KO or HO-1 KO mice with the meningitis, edaravone treatment was no longer effective in improving the survival rate of the mice with severe meningitis (20.2% and 53.6%, respectively), nor it affected the protein levels of HMGB1 and iNOS in the hippocampus of the mice with mild meningitis.
Conclusion:
Edaravone produces neuroprotective actions in a mouse model of pneumococcal meningitis by reducing neuronal apoptosis and HMGB1 and iNOS expression in the hippocampus via the Nrf2/HO-1 pathway. Thus, edaravone may be a promising agent for the treatment of bacterial meningitis.
Similar content being viewed by others
Introduction
Bacterial meningitis (BM) is a severe infection of the central nervous system (CNS) associated with a high mortality rate and primarily occurs in infants1,2. Streptococcus pneumoniae is the most common pathogen that causes BM3. Despite the advances in antimicrobial therapy against BM, up to 50% of BM survivors develop long-term neurofunctional sequelae due to neuronal injury, such as mental retardation, hearing loss, learning and memory impairment and seizures4,5,6. Some neurofunctional sequelae, such as learning and memory impairment, are correlated with neuronal apoptosis in the hippocampus7,8. Hippocampal apoptosis and cortical necrosis are prominently observed in experimental BM9,10.
Inflammation in the meninges and subarachnoid space is typical of BM and substantially drives the pathologic development of BM11. During BM, an excessive inflammatory reaction, including the release of pro-inflammatory cytokines [tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and IL-6] and matrix metalloproteinases (MMPs), is largely responsible for brain damage12. Damaged cells can send alarm signals, called danger-associated molecular patterns, to activate the immune response; these signals include heat shock proteins, IL-33, and high mobility group box 1 protein (HMGB1)13,14. HMGB1 is a ubiquitous nuclear protein that modulates the activation of the innate immune response15. Accumulating knowledge on the contribution of HMGB1 to the pathogenesis of pneumococcal meningitis suggests that HMGB1 acts as a central propagator of inflammation16. Moreover, nitric oxide (NO), generated via the conversion of L-arginine to L-citrulline catalyzed by a cluster of isoenzymes named nitric oxide synthases (NOSs), is also a substantial concern during meningitis. Excess production of NO is intimately linked to the interference with cerebrovascular permeability, brain edema, and meningeal inflammation in experimental meningitis17,18.
In addition to the inflammatory response, oxidative stress also plays a critical role in the pathophysiologic response in some inflammatory diseases, such as sepsis19 and pneumococcal meningitis20. Currently, many antioxidants have been employed as adjuvant therapies in experimental pneumococcal meningitis because the oxidative damage in the hippocampus and cortex associated with cognitive impairment after CNS infection with S pneumoniae results from the large amount of reactive oxygen species (ROS) produced during pneumococcal meningitis21,22. Edaravone (3-methyl-1-phenyl-2-pyrazolin-5-one), an antioxidant, exhibits strong antioxidant activity by scavenging oxygen free radicals23,24,25. Several studies have shown that edaravone exhibits neuroprotective effects by attenuating the oxidative damage of vascular endothelial cells and nerve cells through NOS inhibition26,27. In a rat model of acute intracerebral hemorrhage (ICH), edaravone attenuated brain edema and neurological deficits when the treatment was started immediately or 2 h after ICH28. Additionally, edaravone noticeably reduced the expression of inflammatory mediators, including TNF-α, IL-1β, and inducible NOS (iNOS), as well as one isoform of NOS, in activated microglia in rats with middle cerebral artery occlusion (MCAO) and in activated BV-2 cells29. This result strongly suggests that edaravone has an anti-inflammatory effect on activated microglia29. In this current study, we aimed to investigate the effects of edaravone in an infant mouse model of pneumococcal meningitis. We hypothesize that edaravone will protect infant mice from brain damage during BM by reducing the inflammatory reaction in the CNS.
Materials and methods
Infecting organism
S pneumoniae ATCC6303 (serotype 3) obtained from the American Type Culture Collection (ATCC, Rockville, MD, USA) was cultured as previously described30. Briefly, the bacteria were cultured overnight in 10 mL of brain heart infusion medium, then diluted in fresh medium, and grown for 6–8 h (35 °C, CO2 5%) to the logarithmic phase. The culture was centrifuged for 10 min at 5000×g and resuspended in sterile saline to the expected concentration for injection. The accuracy of the inoculum size was confirmed by quantitative cultures.
Infant mouse model of pneumococcal meningitis
A total of 106 nursing C57BL/6 mice were used throughout the experiments. Nursing C57BL/6 mice purchased from the Shanghai Laboratory Animal Center (Shanghai, China) were infected on postnatal d 11 by a direct intracisternal injection of 10 μL of saline containing a certain inoculum of S pneumoniae, as previously described30. Ten C57BL/6 mice were first use to determine the desired concentration of S pneumoniae to induce a mouse model of severe meningitis or mild meningitis. The severity of pneumococcal meningitis was assessed by a clinical score (5=normal activity; 4=reduced ambulation; 3=slow righting (>5 s/<30 s); 2=unable to right; and 1=coma). At 16 h after infection, severe meningitis was quantified as a clinical score ≤2, and eventually caused death within 1 week after S pneumoniae infection; mild meningitis was quantified as a clinical score >3 and did not cause death within 2 weeks after S pneumoniae infection. For the different experiments, the mice were divided into four groups (n=8/group): Sham; Sham+Edaravone; Meningitis; and Meningitis+Edaravone. The Sham group was injected with 10 μL of saline. The Sham+Edaravone group received an intraperitoneal injection of edaravone (Mitsubishi Pharma Corporation, Tokyo, Japan) at a dose of 3 mg/kg body weight once a day for 7 d; edaravone was diluted with saline to a concentration of 3 mg/mL. The Meningitis group received a direct intracisternal injection of 10 μL of saline containing a certain inoculum of S pneumoniae, and the Meningitis+Edaravone group received a direct intracisternal injection of 10 μL of saline containing a certain inoculum of S pneumoniae combined with edaravone for 7 d. The animal protocol was approved by the Committee on the Ethics of Animal Experiments of Southern Medical University.
White blood cell (WBC) count
Leukocyte counts in the cerebrospinal fluid (CSF) were examined after the animals were infected with S pneumoniae. One microliter of CSF was diluted 1:10 in phosphate-buffered saline (PBS) and then diluted 1:2 in Türk's solution. Leukocyte numbers were recorded in a Neubauer chamber (Poly Labo Paul Block & Cie, Strasbourg, France) using a light microscope.
Measurement of TNF-α, IL-6, and IL-10 concentrations
TNF-α levels in the CSF samples were detected using an ELISA kit according to the manufacturer's instructions (Biosource International, Camarillo, CA, USA). Then, the hippocampus was isolated to analyze the levels of IL-6 and IL-10 in each group. The cytokine concentrations in the hippocampus were determined using commercially available enzyme-linked immunosorbent assays as previously described31, according to the manufacturer's instructions (Biosource International, Camarillo, CA, USA).
Quantification of apoptosis
To investigate the effect of edaravone on hippocampal apoptosis, terminal deoxyribonucleotidyl transferase (TdT)-mediated biotin-16-dUTP nick-end labeling (TUNEL assay) was performed as previously described32. Hippocampal neuron injury was observed by bright-field microscopy. Apoptotic cell numbers were counted in three high-visual fields for the quantitative assessment of apoptosis as previously described33.
Western blotting
Western blotting was performed as previously described. Hippocampal tissues collected from the mice were lysed in buffer containing 25 mmol/L Tris (pH 7.5), 50 mmol/L NaCl, 10 mmol/L EDTA, and protease inhibitors (Roche). Twenty-five micrograms of proteins was subjected to 15% SDS-PAGE, transferred to nitrocellulose membranes (Whatman, Inc, Florham Park, NJ, USA) for 60 min at 100 V and then probed with a chicken anti-HMGB1 antibody (Shino-Test Corp). After incubation with a peroxidase-conjugated secondary antibody, the immunoreactive bands were visualized using an enhanced chemiluminescence kit (GE Lifesciences). After incubation in blocking buffer (Tris-buffered saline containing 150 mmol/L NaCl, 50 mmol/L Tris, and 0.05% Tween-20, pH 7.5) for 1 h at room temperature, the membrane was incubated with specific primary antibodies against Cathepsin K, Bcl-2, Bax, Caspase 3, Caspase 9, and β-actin (Santa Cruz, USA) in blocking buffer overnight at 4 °C and then incubated with secondary antibodies labeled with horseradish peroxidase (HRP), followed by the detection with chemiluminescence (ECL) reagent (Amersham, Buckinghamshire, UK). β-Actin was used as a protein loading control.
Statistical analysis
Statistical analysis was performed using GraphPad Prism software (Prism 6 for Windows, GraphPad Software Inc, San Diego, CA, USA). Comparisons between more than two groups were performed by one-way ANOVA, followed by Tukey's multiple comparison test. Data are presented as the mean±standard deviations (SDs); P<0.05 was considered statistically significant. All experiments were performed three times.
Results
Effects of edaravone on mortality in experimental mice with severe meningitis
To assess the effects of edaravone on severe meningitis, Kaplan-Meier curves were used to analyze the survival of mice with severe meningitis from the time of infection to 8 d after infection (Figure 1). The mice were divided into 4 groups: Sham, Sham+Edaravone, Meningitis, and Meningitis+Edaravone. There was a significant difference in the survival rate between the sham group (100%) and the meningitis group (32.2%) (P<0.05), as well as between the control meningitis group (32.2%) and the edaravone-treated meningitis group (76.4%)(P<0.05).
Kaplan-Meier survival curves of mice with severe pneumococcal meningitis. The results are expressed as the percentage of animals surviving over time. &Indicates a significant difference between the sham group and the meningitis group (P<0.05). *Indicates a significant difference between the meningitis group and the edaravone-treated meningitis group (P<0.05).
Effects of edaravone on the clinical parameters of the experimental mice with mild meningitis
As shown in Figure 1, edaravone induced a dramatic improvement in the survival rate in mice with severe meningitis. We next investigated the effects of edaravone in mice with mild meningitis, which survived for 2 weeks after the S pneumoniae infection. Considering that the mice with mild meningitis slowly exhibited neurological signs of BM within several days after the induction of pneumococcal meningitis, we assessed the clinical neurological deficit score in mice with mild meningitis 14 d after the S pneumoniae infection using a neurological scoring system34. The neurological function of mice with mild meningitis was significantly improved after edaravone treatment (Figure 2A, P<0.05). In addition, a significant difference in body weights was observed between the control meningitis group and the edaravone-treated meningitis group (Figure 2B, P<0.05).
Clinical neurological deficit scores (A) and body weight changes (B) in the experimental animals 14 d after the induction of pneumococcal meningitis. &Indicates a significant difference between the sham group and the meningitis group (P<0.05). *Indicates a significant difference between the control meningitis group and the edaravone-treated meningitis group (P<0.05).
Effects of edaravone on CSF inflammation and cytokine levels in the hippocampus
Figure 3A illustrates the effect of edaravone on the number of leukocytes in the CSF 7 d after the induction of mild pneumococcal meningitis. Compared with the control meningitis group, the edaravone-treated meningitis group exhibited a significant decrease in WBCs. Meanwhile, the edaravone-treated meningitis group exhibited a significantly lower level of TNF-α than the control meningitis group (Figure 3B, P<0.05). However, there was no significant difference in the IL-10 and IL-6 levels between the control meningitis group and the edaravone-treated meningitis group (Figure 3C and 3D).
Leukocyte counts (A) and TNF-α (B) in the CSF, IL-10 (C) and IL-6 (D) concentrations in the hippocampus of the experimental mice 7 d after the induction of mild pneumococcal meningitis. &Indicates a significant difference between the sham group and the meningitis group (P<0.05). *Indicates a significant difference between the control meningitis group and the edaravone-treated meningitis group (P<0.05).
Moreover, we investigated the effect of edaravone on the hippocampus tissue in mice suffering from meningitis. The images of neuronal apoptosis in the hippocampus from each group are shown in Figure 4A. Compared with the control meningitis group, a significant decrease in the number of apoptotic neurons was observed in the edaravone-treated meningitis group (Figure 4B, P<0.05).
Images of neuronal apoptosis in the hippocampus of each group (A): a: Sham group; b: sham+edaravone group; c: Meningitis group; and d: Edaravone+meningitis group. TUNEL assay (B) was used for the quantitative assessment of the number of apoptotic cells in the experimental mice 7 d after the induction of mild pneumococcal meningitis. &Indicates a significant difference between the sham group and the meningitis group (P<0.05). *Indicates a significant difference between the control meningitis group and the edaravone-treated meningitis group (P<0.05).
Effects of edaravone on important proteins involved in hippocampal damage
The HMGB1 level in the hippocampus was examined 7 d after the induction of mild pneumococcal meningitis. Compared with the control meningitis group, the edaravone-treated meningitis group exhibited a significant decrease in HMGB1 (Figure 5A, P<0.05). Moreover, the hippocampal levels of three NOS isoforms, neuronal NOS (nNOS), inducible NOS (iNOS), and endothelial NOS (eNOS), were examined. The edaravone-treated meningitis group exhibited an obvious and significant decrease in iNOS compared with the control meningitis group (Figure 5B, P<0.05), but no significant changes in eNOS and nNOS were observed among the four groups (Figure 5C and 5D).
HMGB1 (A), iNOS (B), eNOS (C), and nNOS (D) levels in the hippocampus of the experimental mice 7 d after the induction of mild pneumococcal meningitis. Representative immunoblots are shown in the top panel, and the quantitative results are shown in the bottom panel. &Indicates a significant difference between the sham group and the meningitis group (P<0.05). *Indicates a significant difference between the control meningitis group and the edaravone-treated meningitis group (P<0.05).
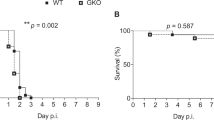
Considering that HMGB1 and iNOS secretion were associated with the nuclear factor (erythroid-derived 2)-like 2 (Nrf2) and heme oxygenase-1 (HO-1) genes35,36, we further investigated the effects of edaravone on HMGB1 and iNOS using Nrf2 KO and HO-1 KO mice models. Eight days after S pneumoniae infection, a significant difference in the survival rate between the meningitis+edaravone group (76.4%) and the meningitis+edaravone+Nrf2 KO group (20.2%), as well as between the meningitis+edaravone group (76.4%) and the meningitis+edaravone+HO-1 KO group (53.6%) was observed (Figure 6A). In addition, both the Nrf2 and HO-1 gene-deficient mice with meningitis exhibited a significant increase in the HMGB1 and iNOS levels after edaravone treatment (Figure 6B and 6C, P<0.05).
Kaplan-Meier survival curves of KO mice subjected to pneumococcal meningitis (A). HMGB1 (B) and iNOS (C) levels in the experimental mice. &Indicates a significant difference between the edaravone-treated meningitis group and the experimental Nrf2 KO or HO-1 KO mice (P<0.05).
Discussion
The antioxidant/oxidant status of the CSF in human meningitis has been studied previously37,38. In the present study, we showed the effects of edaravone, an antioxidant, on the survival rate, clinical parameters, leukocyte counts, cytokine levels, and several proteins involved in hippocampal damage in an infant mouse model of pneumococcal meningitis. The terrible survival rate in the severe meningitis group was significantly improved following edaravone treatment, suggesting that edaravone can serve as a new agent for the treatment of meningitis. A previous study has reported that edaravone is effective in ameliorating neurological function and secondary ischemia after ICH39. Our data showed that edaravone produced an obvious improvement in the neurological function deficits in a mouse model of meningitis. In addition, a significant beneficial effect of edaravone on weight loss in the mouse model of meningitis was observed in this study.
During pneumococcal meningitis, S pneumoniae regulates CSF homeostasis, the initiation of the host inflammatory response following pneumococcal infection, and the accompanying cytokine production and leukocyte migration into the subarachnoidal space40,41. A significant increase in TNF-α, IL-8 and IL-6 levels has been observed in CSF samples from children with meningitis compared with controls42. The cytokines TNF-α, IL-6, and IL-10 are generated after pneumococcal infection, leading to the upregulation of several adhesion factors on the vascular endothelium, which mediate leukocyte flux43. The anti-inflammatory cytokine IL-10 also participates in regulating the immune response in pneumococcal meningitis44. In our study, edaravone treatment markedly reduced the increased WBC and TNF-α levels observed in the CSF samples of the control meningitis group, but the IL-6 and IL-10 levels did not differ significantly between the hippocampus from the edaravone-treated meningitis group and the control meningitis group, indicating that edaravone had no beneficial effect on the regulation of inflammatory cytokines in the hippocampus after the induction of meningitis.
However, it is well established that hippocampal cells are damaged in the brain during BM33,45. A recent study in a mouse model of acute cerebral infarction revealed that edaravone is capable of promoting neurogenesis following neuronal damage in the hippocampal dentate gyrus46. Interestingly, in the present study, neuronal apoptosis in the hippocampus during pneumococcal meningitis was also attenuated by treatment with edaravone, indicating a neuroprotective effect of edaravone on the BM-induced neuronal damage in the hippocampus. Accumulating knowledge regarding the contribution of HMGB1 to the pathogenesis of pneumococcal meningitis suggests that HMGB1 can serve as a central propagator of inflammation16. Moreover, two studies have reported the release of HMGB1 into the CSF during acute bacterial meningitis in children47,48. Our results showed that the elevation of HMGB1 in the hippocampus of an infant mouse with pneumococcal meningitis was substantially reduced by edaravone treatment, consistent with a previous report showing that edaravone attenuated the release of HMGB1 in neuronal cells from rats with cerebral infarction49. More importantly, a significant increase in iNOS was observed in the hippocampus of the meningitis group, whereas the edaravone treatment significantly reduced the iNOS level, but few changes in eNOS and nNOS levels were detected in the hippocampus of the four groups. iNOS-derived NO not only exhibits antimicrobial effects on some pathogens but also contributes to tissue damage in some cases of inflammation or infection50. Increased NO has been observed in animal models of BM, as well as in children with this disease51,52. Moreover, emerging evidence has shown that edaravone has a protective effect on cerebral infarction by reducing the serum NOS levels53. Here, our data showed a significant decrease in iNOS after edaravone treatment, indicating that edaravone can protect infant mice against hippocampal damage during meningitis by inhibiting iNOS-derived NO production.
Currently, the use of KO mice has provided new insights into the role of some cytokines involved in the inflammatory cascade during BM. Enhanced defense and reduced inflammation in IL-18 gene-deficient mice with pneumococcal meningitis suggested that endogenous IL-18 contributes to a disadvantageous inflammatory response54. Nrf2 is a critical regulator of the inducible antioxidant response, which has been shown to mediate the expression of some enzymes that provide protection against oxidative stress, thus attenuating cellular injury from oxidative stress induced by some redox insults55. Nrf2 also contributes to protection from oxidative stress in sepsis, which represents a disordered innate immune response to pathogens, suggesting a possible link between the cellular redox state and innate immunity in some inflammatory diseases19. HO-1, the inducible HO isoform, is a cytoprotective enzyme that catalyzes the conversion of the pro-oxidant heme to carbon monoxide (CO) and biliverdin/bilirubin. Biliverdin can be converted to bilirubin, a powerful endogenous antioxidant56, and biliverdin also has proven anti-inflammatory properties57. In an HO-1-deficient mouse model of endotoxemia, Wiesel et al58 found that the loss of HO-1 resulted in enhanced oxidative stress, further contributing to end-organ injury and death in mice. HO-1 also exhibits anti-inflammatory effects in response to different stimuli, such as nephrotoxic, ischemic, and inflammatory reactions59,60. More importantly, recent studies have shown that HMGB1 and iNOS release are closely related to the Nrf2 and HO-1 genes35,36,61; thus, in this study, the use of Nrf2 KO and HO-1 KO mice models has further increased our understanding of the related pathways by which edaravone exerts its effects on an infant mouse model of pneumococcal meningitis. We found that Nrf2 or HO-1 gene-deficient mice with pneumococcal meningitis showed significantly higher levels of HMGB1 and iNOS after edaravone treatment, in contrast to the lower levels of HMGB1 and iNOS in the edaravone-treated meningitis group, suggesting that the elimination of the Nrf2 or HO-1 genes can cause detrimental outcomes in this disease. These results indicated a crucial role of Nrf2/HO-1 in the regulation of HMGB1 and iNOS during pneumococcal meningitis.
In summary, our results show that edaravone, a free radical scavenger, provides a protective effect against hippocampal damage in an infant mouse model of pneumococcal meningitis by reducing the levels of HMGB1 and iNOS through the Nrf/HO-1 pathway. Our study suggests that edaravone may serve as a new agent for therapeutic interventions in BM.
Author contribution
Zheng LI designed the study; Qian-qian MA and Yan YAN performed the experiments; Wei-qin ZHOU contributed new reagents or analytical tools; Feng-dan XU and Xiao-ying ZHANG analyzed the data; and Zhi-chun FENG wrote the paper.
References
Kim KS . Pathogenesis of bacterial meningitis: from bacteraemia to neuronal injury. Nat Rev Neurosci 2003; 4: 376–85.
Mook-Kanamori BB, Madelijn G, Tom VDP, Diederik VDB . Pathogenesis and pathophysiology of pneumococcal meningitis. Clin Microbiol Rev 2011; 24: 721–36.
Thigpen MC, Whitney CG, Messonnier NE, Zell ER, Ruth L, Hadler JL, et al. Bacterial meningitis in the United States, 1998-2007. New Engl J Med 2011; 364: 2016–25.
Aruna C, Hadley H, Derek M, Mathuram S . Long-term sequelae of childhood bacterial meningitis: an underappreciated problem. Pediatr Infect Dis J 2011; 30: 3–6.
Grimwood K, Anderson P, Anderson V, Tan L, Nolan T . Twelve year outcomes following bacterial meningitis: further evidence for persisting effects. Arch Dis Child 2000; 83: 111–6.
Richard . Meningitis in infancy in England and Wales: follow up at age 5 years. BMJ 2001; 323: 533–6.
Wellmer A, Noeske C, Gerber J, Munzel U, Nau R . Spatial memory and learning deficits after experimental pneumococcal meningitis in mice. Neurosci Lett 2000; 296: 137–40.
Loeffler JM, Ringer R, Hablützel M, Täuber MG, Leib SL . The free radical scavenger alpha-phenyl-tert-butyl nitrone aggravates hippocampal apoptosis and learning deficits in experimental pneumococcal meningitis. J Infect Dis 2001; 183: 247–52.
Zysk G, Brück W, Gerber J, Brück Y, Prange HW, Nau R . Anti-inflammatory treatment influences neuronal apoptotic cell death in the dentate gyrus in experimental pneumococcal meningitis. J Neuropathol Exp Neurol 1996; 55: 722–8.
Christian S, Christian B, Helle Bossen K, Susanne S . Differences in survival, brain damage, and cerebrospinal fluid cytokine kinetics due to meningitis caused by 3 different Streptococcus pneumoniae serotypes: evaluation in humans and in 2 experimental models. J Infect Dis 2004; 190: 1212–20.
Coutinho LG, Christen S, Bellac CL, Fontes FL, Souza FR, Grandgirard D, et al. The kynurenine pathway is involved in bacterial meningitis. J Neuroinflammation 2014; 11: 169.
Tunkel AR, Scheld WM . Pathogenesis and pathophysiology of bacterial meningitis. Clin Microbiol Rev 1993; 6: 118–36.
Hajime K, Rock KL . How dying cells alert the immune system to danger. Nat Rev Immunol 2008; 8: 279–89.
Bianchi ME . DAMPs, PAMPs and alarmins: all we need to know about danger. J Leukoc Biol 2007; 81: 1–5.
Andersson U, Tracey KJ . HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol 2011; 29: 139–62.
Christopher HH, Michael W, Barbara A, Sven H, Hans HC, Matthias K, et al. High mobility group box 1 prolongs inflammation and worsens disease in pneumococcal meningitis. Brain 2013; 136: 1746–59.
Boje KM . Inhibition of nitric oxide synthase attenuates blood-brain barrier disruption during experimental meningitis. Brain Res 1996; 720: 75–83.
Uwe K, Andrea B, Robert P, Karl F, Adriano F, Pfister HW . Experimental pneumococcal meningitis: Cerebrovascular alterations, brain edema, and meningeal inflammation are linked to the production of nitric oxide. Ann Neurol 1995; 37: 313–23.
Kolls JK . Oxidative stress in sepsis: a redox redux. J Clin Invest 2006; 116: 860–3.
Barichello T, Petronilho FC, Silva GZ, Souza B, Savi GD, Feier G, et al. Oxidative damage in the rat hippocampus and cortex after meningitis induced by Streptococcus pneumoniae. BMC Proceed 2008; 2: P6.
Tatiana B, Santos ALB, Savi GD, Generoso JS, Paola O, Michelon CM, et al. Antioxidant treatment prevents cognitive impairment and oxidative damage in pneumococcal meningitis survivor rats. Metab Brain Dis 2012; 27: 587–93.
Matthias K, Uwe K, Hans-Walter P . Oxidative stress in pneumococcal meningitis: a future target for adjunctive therapy? Prog Neurobiol 2006; 80: 269–80.
Watanabe T, Tahara M, Todo S . The novel antioxidant edaravone: from bench to bedside. Cardiovasc Ther 2008; 26: 101–14.
Arumugam S, Thandavarayan RA, Veeraveedu PT, Nakamura T, Arozal W, Sari FR, et al. Beneficial effects of edaravone, a novel antioxidant, in rats with dilated cardiomyopathy. J Cell Mol Med 2012; 16: 2176–85.
Zhang N, Kominekobayashi M, Tanaka R, Liu M, Mizuno Y, Urabe T . Edaravone reduces early accumulation of oxidative products and sequential inflammatory responses after transient focal ischemia in mice brain. Stroke 2005; 36: 2220–5.
Group EAIS . Effect of a novel free radical scavenger, edaravone (MCI-186), on acute brain infarction. Randomized, placebo-controlled, double-blind study at multicenters. Cerebrovasc Dis 2003; 15: 222–9.
Hiroshi Y, Hidekatsu Y, Yoshihisa N, Kayoko FS, Nobuyuki F, Norio T . Neuroprotective effects of edaravone: a novel free radical scavenger in cerebrovascular injury. CNS Drug Rev 2006; 12: 9–20.
Nakamura T, Kuroda Y, Yamashita S, Zhang X, Miyamoto O, Tamiya T, et al. Edaravone attenuates brain edema and neurologic deficits in a rat model of acute intracerebral hemorrhage. Stroke 2008; 39: 463–9.
Yun Y, Hao Z, Rangarajan P, Ling EA, Wu C . Anti-inflammatory effects of Edaravone and Scutellarin in activated microglia in experimentally induced ischemia injury in rats and in BV-2 microglia. BMC Neurosci 2014; 15: 125.
Grandgirard D, Steiner O, Täuber MG, Leib SL . An infant mouse model of brain damage in pneumococcal meningitis. Acta Neuropathol 2007; 114: 609–17.
Barichello T, Generoso JS, Simões LR, Elias SG, Tashiro MH, Dominguini D, et al. Inhibition of indoleamine 2,3-dioxygenase prevented cognitive impairment in adult Wistar rats subjected to pneumococcal meningitis. Transl Res 2013; 162: 390–7.
Wijsman JH, Jonker RR, Keijzer R, van de Velde CJ, Cornelisse CJ, van Dierendonck JH . A new method to detect apoptosis in paraffin sections: in situ end-labeling of fragmented DNA. J Histochem Cytochem 1993; 41: 7–12.
Bifrare YD, Gianinazzi C, Imboden H, Leib SL, Täuber MG . Bacterial meningitis causes two distinct forms of cellular damage in the hippocampal dentate gyrus in infant rats. Hippocampus 2003; 13: 481–8.
Spranger M, Schwab S, Krempien S, Winterholler M, Steiner T, Hacke W . Excess glutamate levels in the cerebrospinal fluid predict clinical outcome of bacterial meningitis. Arch Neurol 1996; 53: 992–6.
Park EJ, Jang HJ, Tsoyi K, Kim YM, Park SW, Kim HJ, et al. The heme oxygenase-1 inducer THI-56 negatively regulates iNOS expression and HMGB1 release in LPS-activated RAW 264.7 cells and CLP-induced septic mice. PLoS One 2013; 8: e76293.
Kim YM, Kim HJ, Chang KC . Glycyrrhizin reduces HMGB1 secretion in lipopolysaccharide-activated RAW 264.7 cells and endotoxemic mice by p38/Nrf2-dependent induction of HO-1. Int Immunopharmacol 2015; 26: 112–8.
Barichello T, Savi GD, Panatto AP, Generoso JS, Cipriano AL, Rezin GT, et al. Effect of new compound with antioxidant potential in the energy metabolism of adults rats after pneumococcal meningitis. Am J Pharmacol Toxicol 2012; 7: 49–61.
Aycicek A, Iscan A, Erel O, Akcali M, Selek S . Total antioxidant/oxidant status in meningism and meningitis. Pediatr Neurol 2006; 35: 382–6.
Gu XL, Gao Y, Sun T, Zhu DY . Effects of edaravone on score of neurological behavior,cerebral ischemia areas and amount of bleeding after cerebral hemorrhage in rats. Chin J New Drugs Clin Remedies 2006; 25: 358–61.
Ostergaard C, Yieng-Kow RV, Benfield T, Frimodt-Møller N, Espersen F, Lundgren JD . Inhibition of leukocyte entry into the brain by the selectin blocker fucoidin decreases interleukin-1 (IL-1) levels but increases IL-8 levels in cerebrospinal fluid during experimental pneumococcal meningitis in rabbits. Infect Immun 2000; 68: 3153–7.
Mook-Kanamori BB, Geldhoff M, van der Poll T, van de Beek D . Pathogenesis and pathophysiology of pneumococcal meningitis. Clin Microbiol Rev 2011; 24: 557–91.
Prasad R, Kapoor R, Srivastava R, Mishra OP, Singh TB . Cerebrospinal fluid TNF-α, IL-6, and IL-8 in children with bacterial meningitis. Pediatr Neurol 2014; 50: 60–5.
Fassbender K, Schminke U, Ries S, Ragoschke A, Kischka U, Fatar M, et al. Endothelial-derived adhesion molecules in bacterial meningitis: association to cytokine release and intrathecal leukocyte-recruitment. J Neuroimmunol 1997; 74: 130–4.
Zwijnenburg PJ, van der Poll T, Florquin S, Roord JJ, van Furth AM . Interleukin-10 negatively regulates local cytokine and chemokine production but does not influence antibacterial host defense during murine pneumococcal meningitis. Infect Immun 2003; 71: 2276–9.
Leib SL, Leppert D, Clements J, Täuber MG . Matrix metalloproteinases contribute to brain damage in experimental pneumococcal meningitis. Infect Immun 2000; 68: 615–20.
Kikuta M, Shiba T, Yoneyama M, Kawada K, Yamaguchi T, Hinoi E, et al. In vivo and in vitro treatment with edaravone promotes proliferation of neural progenitor cells generated following neuronal loss in the mouse dentate gyrus. J Pharmacol Sci 2013; 121: 74–83.
Asano T, Ichiki K, Koizumi S, Kaizu K, Hatori T, Mashiko K, et al. High mobility group box 1 in cerebrospinal fluid from several neurological diseases at early time points. Int J Neurosci 2011; 121: 480–4.
Tang D, Kang R, Cao L, Zhang G, Yu Y, Xiao W, et al. A pilot study to detect high mobility group box 1 and heat shock protein 72 in cerebrospinal fluid of pediatric patients with meningitis. Crit Care Med 2008; 36: 291–5.
Kikuchi K, Kawahara K, Tancharoen S, Matsuda F, Morimoto Y, Ito T, et al. The free radical scavenger edaravone rescues rats from cerebral infarction by attenuating the release of high-mobility group box-1 in neuronal cells. J Pharmacol Exp Ther 2009; 329: 865–74.
Licinio J, Prolo P, Mccann SM, Wong ML . Brain iNOS: current understanding and clinical implications. Mol Med Today 1999; 5: 225–32.
Suzuki Y, Fujii S, Tominaga T, Yoshimoto T, Fujii S, Akaike T, et al. Direct evidence of in vivo nitric oxide production and inducible nitric oxide synthase mRNA expression in the brain of living rat during experimental meningitis. J Cereb Blood Flow Metab 1999; 19: 1175–8.
Kornelisse RF, Hoekman K, Visser JJ, Hop WC, Huijmans JG, van der Straaten PJ, et al. The role of nitric oxide in bacterial meningitis in children. J Infect Dis 1996; 174: 120–6.
Li B . The effect of edaravone on serum NO, NOS, MDA and SOD in patients with acute cerebral infarction. Chin J Arteriosclerosis 2010.
Zwijnenburg PJ, van der Poll T, Florquin S, Akira S, Takeda K, Roord JJ, et al. Interleukin-18 gene-deficient mice show enhanced defense and reduced inflammation during pneumococcal meningitis. J Neuroimmunol 2003; 138: 31–7.
Gupte AA, Lyon CJ, Hsueh WA . Nuclear factor (erythroid-derived 2)-like-2 factor (Nrf2), a key regulator of the antioxidant response to protect against atherosclerosis and nonalcoholic steatohepatitis. Curr Diab Rep 2013; 13: 362–71.
Stocker R, Yamamoto Y, Mcdonagh AF, Glazer AN, Ames BN . Bilirubin is an antioxidant of possible physiological importance. Science 1987; 235: 1043–6.
Sarady-Andrews JK, Liu F, Gallo D, Nakao A, Overhaus M, Ollinger R, et al. Biliverdin administration protects against endotoxin-induced acute lung injury in rats. Am J Physiol Lung Cell Mol Physiol 2005; 289: L1131–7.
Wiesel P, Patel AP, Difonzo N, Marria PB, Sim CU, Pellacani A, et al. Endotoxin-induced mortality is related to increased oxidative stress and end-organ dysfunction, not refractory hypotension, in heme oxygenase-1-deficient mice. Circulation 2000; 102: 3015–22.
Kanwar YS . Heme oxygenase-1 in renal injury: conclusions of studies in humans and animal models. Kidney Int 2001; 59: 378–9.
Nath KA, Balla G, Vercellotti GM, Balla J, Jacob HS, Levitt MD, et al. Induction of heme oxygenase is a rapid, protective response in rhabdomyolysis in the rat. J Clin Invest 1992; 90: 267–70.
Kim HS, Park EJ, Sang WP, Kim HJ, Chang KC . A tetrahydroisoquinoline alkaloid THI-28 reduces LPS-induced HMGB1 and diminishes organ injury in septic mice through p38 and PI3K/Nrf2/HO-1 signals. Int Immunopharmacol 2013; 17: 684–92.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Z., Ma, Qq., Yan, Y. et al. Edaravone attenuates hippocampal damage in an infant mouse model of pneumococcal meningitis by reducing HMGB1 and iNOS expression via the Nrf2/HO-1 pathway. Acta Pharmacol Sin 37, 1298–1306 (2016). https://doi.org/10.1038/aps.2016.71
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2016.71
Keywords
This article is cited by
-
Edaravone Confers Neuroprotective, Anti-inflammatory, and Antioxidant Effects on the Fetal Brain of a Placental-ischemia Mouse Model
Journal of Neuroimmune Pharmacology (2023)
-
Ulinastatin Attenuates LPS-Induced Inflammation and Inhibits Endoplasmic Reticulum Stress–Induced Apoptosis in Renal Tubular Epithelial Cells via Regulation of the TLR4/NF-κB and Nrf2/HO-1 Pathways
Inflammation (2021)
-
Ulinastatin attenuates LPS-induced inflammation in mouse macrophage RAW264.7 cells by inhibiting the JNK/NF-κB signaling pathway and activating the PI3K/Akt/Nrf2 pathway
Acta Pharmacologica Sinica (2018)
-
Diterpene ginkgolides protect against cerebral ischemia/reperfusion damage in rats by activating Nrf2 and CREB through PI3K/Akt signaling
Acta Pharmacologica Sinica (2018)