Abstract
Aim:
To evaluate the effects of an Al3+- and Mg2+-containing antacid, ferrous sulfate, and calcium carbonate on the absorption of nemonoxacin in healthy humans.
Methods:
Two single-dose, open-label, randomized, crossover studies were conducted in 24 healthy male Chinese volunteers (12 per study). In Study 1, the subjects orally received nemonoxacin (500 mg) alone, or an antacid (containing 318 mg of Al3+ and 496 mg of Mg2+) plus nemonoxacin administered 2 h before, concomitantly or 4 h after the antacid. In Study 2, the subjects orally received nemonoxacin (500 mg) alone, or nemonoxacin concomitantly with ferrous sulfate (containing 60 mg of Fe2+) or calcium carbonate (containing 600 mg of Ca2+).
Results:
Concomitant administration of nemonoxacin with the antacid significantly decreased the area under the concentration-time curve from time 0 to infinity (AUC0–∞) for nemonoxacin by 80.5%, the maximum concentration (Cmax) by 77.8%, and urine recovery (Ae) by 76.3%. Administration of nemonoxacin 4 h after the antacid decreased the AUC0–∞ for nemonoxacin by 58.0%, Cmax by 52.7%, and Ae by 57.7%. Administration of nemonoxacin 2 h before the antacid did not affect the absorption of nemonoxacin. Administration of nemonoxacin concomitantly with ferrous sulfate markedly decreased AUC0–∞ by 63.7%, Cmax by 57.0%, and Ae by 59.7%, while concomitant administration of nemonoxacin with calcium carbonate mildly decreased AUC0–∞ by 17.8%, Cmax by 14.3%, and Ae by 18.4%.
Conclusion:
Metal ions, Al3+, Mg2+, and Fe2+ markedly decreased the absorption of nemonoxacin in healthy Chinese males, whereas Ca2+ had much weaker effects. To avoid the effects of Al3+ and Mg2+-containing drugs, nemonoxacin should be administered ≥2 h before them.
Similar content being viewed by others
Introduction
Nemonoxacin (TG-873870) is a novel non-fluorinated quinolone developed from a series of 8-methoxy non-fluorinated quinolones1 as a malate salt (Figure 1). It shows a broad spectrum of activity2,3 against Gram-positive, Gram-negative, and atypical pathogens. Furthermore, it appears to be more potent than other fluoroquinolones, including ciprofloxacin, levofloxacin, and moxifloxacin4. Phase I clinical studies have shown that nemonoxacin is well tolerated up to a maximum dose of 1500 mg after a single oral dose and 1000 mg when administered once daily for 10 d5,6,7. Phase II studies have shown that once daily administration of 500 or 750 mg nemonoxacin was as effective and safe as once daily administration of 500 mg levofloxacin for the treatment of community-acquired pneumonia8. Nemonoxacin also achieved high clinical and bacteriological success rates compared with levofloxacin in patients with community-acquired pneumonia8.
Chemical structure of nemonoxacin as a malate salt (C20H25N3O4·C4H6O5·½H2O).
Nemonoxacin is completely absorbed after oral administration, with an oral bioavailability of approximately 100% in humans ((X Wu and J Zhang, unpublished data). No major or minor metabolites of nemonoxacin were found in in vitro or in vivo studies, while 50%–70% of nemonoxacin was detected unchanged in urine after an oral dose in humans6,7. In vitro studies showed that nemonoxacin did not induce or inhibit human hepatic CYP3A4 activity (CY Tsai and CP Chow, unpublished data), which suggests there is a low risk of metabolism-related drug-drug interactions. However, it is well known that drugs containing metal ions decrease the absorption of many quinolones. For example, calcium carbonate or ferrous sulfate affected ciprofloxacin absorption9,10, ferrous sulfate affected levofloxacin and moxifloxacin absorption11,12, and Mg2+- or Al3+-containing antacids affected the absorption of most fluoroquinolones13,14,15. This interaction is mainly due to chelation and the formation of a complex between the 3-carboxyl- and 4-oxo-substituents of quinolones and the metal ions16.
Here, we performed two studies to determine the effects of an Al3+- and Mg2+-containing antacid, ferrous sulfate, and calcium carbonate on the absorption of nemonoxacin in healthy volunteers.
Materials and methods
Study drugs
Nemonoxacin Malate Capsules, 500 mg of nemonoxacin per capsule, were provided by TaiGen Biotechnology Co Ltd (Taipei, Taiwan, China). Alumina, Magnesia and Dimethicone Chewable Tablets, 153 mg of aluminum hydroxide, 200 mg of magnesium hydroxide, and 18.9 mg of dimethicone per tablet, were manufactured by Yung Shin Pharm Ind (Kunshan) Co, Ltd (Kunshan, China). Ferrous Sulfate Tablets, 300 mg of ferrous sulfate per tablet, were manufactured by Ji'nan Yongning Pharmaceutical Co, Ltd (Ji-nan, China), and Calcium Carbonate Tablets, 750 mg of calcium carbonate per tablet, were manufactured by Biochemical Pharmaceutical Factory of Zhuhai SEZ (Zhuhai, China).
Volunteers
A total of 25 healthy male Chinese volunteers were enrolled in the studies, with 12 volunteers in Study 1 and 13 volunteers in Study 2. In Study 1, all 12 volunteers completed the study and were included in the pharmacokinetic (PK) analysis. Their mean age was 22.3 years (range 19–29 years) and the mean body weight was 62.8 kg (range 58–67 kg). In Study 2, one volunteer withdrew for personal reasons after the collection of the blood sample 4 h post-dose in period 1, and a replacement volunteer was enrolled. Therefore, 12 volunteers completed the study and were included in the PK analysis. Their mean age was 23.0 years (range 21–24 years) and their mean body weight was 67.6 kg (range 63–73 kg). The volunteers were in good health in terms of their medical history, physical examination, electrocardiography, and routine clinical laboratory tests. None of the subjects used any drugs for ≥2 weeks before the study and alcohol was forbidden from 72 h before administration of the study drugs. All volunteers provided written informed consent before enrollment.
Study design
The clinical studies were conducted at the First Hospital Affiliated to Lanzhou University (Lanzhou, China). All protocols were approved by the hospital's Independent Ethics Committee.
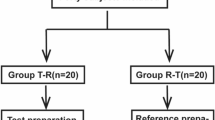
Study 1 was an open, randomized, four-way crossover study designed to investigate the time-dependent interactions between nemonoxacin and an Al3+- and Mg2+-containing antacid. Study 2 was an open, randomized, three-way crossover study designed to assess the effects of ferrous sulfate and calcium carbonate on the absorption of nemonoxacin. Both studies included a washout period of 7 d between each study period. In Study 1, each volunteer received the following treatments in a random order: 500 mg nemonoxacin alone (Treatment A); 500 mg nemonoxacin administered 4 h after an Al3+- and Mg2+-containing antacid (318 mg of Al3+ and 496 mg of Mg2+, Treatment B); 500 mg nemonoxacin administered at the same time as the Al3+- and Mg2+-containing antacid (Treatment C); and 500 mg nemonoxacin administered 2 h before the Al3+- and Mg2+-containing antacid (Treatment D). The dosage of Al3+ and Mg2+ was the same in treatment B, C, and D. In Study 2, each volunteer received the following treatments in a random order: 500 mg nemonoxacin alone (Treatment E); 500 mg nemonoxacin administered together with ferrous sulfate containing 60 mg of Fe2+ (Treatment F); and 500 mg nemonoxacin administered together with calcium carbonate containing 600 mg of Ca2+ (Treatment G). In both studies, nemonoxacin was orally administered to subjects after fasted for ≥10 h. Fasting was continued for ≥3 h after administering nemonoxacin. A snack was provided at 3 h and standard meals were provided at 5 and 10 h after administering nemonoxacin.
Safety evaluation
All of the volunteers who participated in either study were included in the safety analysis. Safety was evaluated based on assessments of physical examinations, vital signs (blood pressure, pulse, respiratory rate, and body temperature), 12-lead electrocardiography (ECG), laboratory tests (clinical chemistry, hematology, urinalysis, and serology), and adverse events (AEs). Vital signs and 12-lead ECGs were assessed before administration and at 2, 4, 24, 48, and 72 h after the administration of nemonoxacin. Clinical chemistry, hematology, and urinalysis were conducted 1 d before dosing and at 24 h after dosing. Additional laboratory tests were performed at 72 h after dosing if abnormal, clinical significant values were obtained at 24 h. AEs were recorded throughout the study period and at follow-up.
Sample collection
In both studies, blood samples (4 mL) were collected from a forearm vein and were placed in heparinized tubes. Samples were obtained before, and at 0.33, 0.67, 1, 1.5, 2, 2.5, 3, 4, 6, 8, 12, 14, 24, 36, 48, and 72 h after administration of nemonoxacin. The samples were centrifuged at 1500×g for 10 min. Plasma was separated and frozen at approximately −70 °C until further analysis. Urine samples were collected before and during the following periods after administration of nemonoxacin: 0–4, 4–8, 8–12, 12–24, 24–48, and 48–72 h. The volume of urine obtained in each collection interval was recorded, and 10 mL of well-mixed urine was frozen at approximately −70 °C until further analysis.
Measurement of plasma and urine nemonoxacin concentrations
The concentrations of nemonoxacin in plasma and urine were determined using validated liquid chromatography–tandem mass spectrometry (LC/MS/MS) assay methods. Both plasma and urine samples were pre-treated with acetonitrile before LC/MS/MS analysis. Chromatography was performed on an Ecilipse Plus C18 column (particle size 3.5 μm, 100×4.6 mm; Agilent, Wilmington, DE, USA) using a mobile phase of 1% formic acid in 5 mmol/L ammonium acetate-acetonitrile (70:30, v/v) at a flow rate of 0.70 mL/min. The column temperature was 40 °C. An API 4000 triple quadrupole mass spectrometer equipped with a TurboIonSpray source (Applied Biosystems, Concord, Ontario, Canada) was used for mass analysis and detection. Quantification was performed using multiple reaction monitoring of the transitions m/z 372→m/z 311 for nemonoxacin and m/z 402→m/z 364 for moxifloxacin, which was used an the internal standard. The nemonoxacin response was linear (r>0.998) over the concentration range of 0.005–5.00 mg/L in plasma and 0.2–200 mg/L in urine. The intra- and inter-batch precision values were <4.3% and 6.1%, respectively, for plasma and were <5.5% and 7.1%, respectively, for urine. The accuracy ranged from 96.4% to 102.1% of the nominal value for plasma and from 96.1% to 98.9% of the nominal value for urine.
PK analysis
The PK parameters were calculated using standard non-compartmental methods. The maximum concentration (Cmax) and the time to reach Cmax (Tmax) were directly taken from the plasma concentration–time curves. The elimination rate constant (λz) was calculated by liner regression of the terminal linear portion of the ln-concentration-time curve, and the apparent elimination half-life (T1/2) was calculated as 0.693/λz. The area under the plasma concentration–time curve (AUC) from time 0 to the last time point (AUC0–t) was calculated using the linear trapezoidal method. The AUC from 0 to infinity (AUC0–∞) was calculated as AUC0–t+Ct/λz, where Ct is the last measurable concentration. Oral clearance (CL/F) was calculated as the nemonoxacin dose/AUC0–∞, and the terminal volume of distribution without correction for bioavailability (Vz/F) was calculated as oral clearance/λz. Renal clearance (CLr) was determined based on the cumulative amount of nemonoxacin excreted in urine divided by the AUC for the collection interval. The percentage of the administered dose recovered in urine (Ae) was also determined. Phoenix WinNonlin software version 6.1 (Pharsight, Mountain View, CA, USA) was used for all PK analysis.
Statistical analysis
In both studies, the AUCs and Cmax were natural logarithm (ln)-transformed and compared by analysis of variance (ANOVA) with the following factors: treatment sequence, volunteer-nested with treatment sequence, period, and treatment. The point estimates and associated 90% confidence intervals (CIs) for the difference between each treatment (Study 1: B–A, C–A, D–A; Study 2: F–E, G–E) were determined using the residual variances taken from the model. The point estimate and CIs on the log scale were then back-transformed to give point estimates and CIs for the ratios (Study 1, B:A, C:A, D:A; Study 2, F:E, G:E). In all analyses, P values of <0.05 were considered statistically significant.
Results
Effects of the Al3+- and Mg2+-containing antacid on nemonoxacin PK
Figure 2 shows the plasma concentration–time curves after administration of a single dose of 500 mg nemonoxacin either alone or at various times relative to Al3+- and Mg2+-containing antacid. The calculated parameters are summarized in Table 1, and the statistical results are presented in Table 2.
Plasma concentration–time curves of nemonoxacin after single oral dose of 500 mg nemonoxacin alone (A), 4 h after an Al3+- and Mg2+-containing antacid (B), at the same time as the antacid (C), or 2 h before the antacid (D) in 12 Chinese healthy male volunteers. Data are presented as the arithmetic mean±SD.
After a single oral dose of 500 mg nemonoxacin, the mean Cmax was 5.54 mg/L, which occurred at 1 h. The mean AUC0–∞ was 40.7 mg·h·L–1 and Ae was 65.3% of the administered dose. Administration of nemonoxacin concomitantly with the Al3+- and Mg2+-containing antacid significantly reduced the absorption of nemonoxacin because Cmax decreased by 77.8%, AUC0–∞ by 80.5%, and Ae by 76.3%. However, these parameters were unaffected when nemonoxacin was administered 2 h before the Al3+- and Mg2+-containing antacid, indicating that this sequence did not affect the absorption of nemonoxacin. We also observed a reduction in the PK parameters when nemonoxacin was administered 4 h after the Al3+- and Mg2+-containing antacid, with a mean decrease in Cmax by 52.7%, AUC0–∞ by 58.0%, and Ae by 57.7%, although the decreases were smaller than when nemonoxacin was administered at the same time as the antacid. However, the inter-individual variance was very large when nemonoxacin was administered 4 h after the Al3+- and Mg2+-containing antacid because, in this treatment, the AUC for nemonoxacin decreased by >80% in seven volunteers but did not change or the change was very small in the other five volunteers, as compared with nemonoxacin administered alone (Figure 3).
Plasma concentration–time curves of nemonoxacin after a single oral dose of 500 mg nemonoxacin alone (A) or 4 h after an Al3+- and Mg2+-containing antacid (B) in 12 Chinese healthy male volunteers. Data for treatment B are shown separately for five volunteers who did not experience a decrease in nemonoxacin absorption and in seven volunteers with a decrease by >80%. Data are presented as the mean±SD.
Effects of ferrous sulfate and calcium carbonate on nemonoxacin PK
Figure 4 shows the plasma concentration–time curves for nemonoxacin administered alone or together with ferrous sulfate or calcium carbonate. The PK parameters for nemonoxacin in these conditions are summarized in Table 1 and the statistical results are presented in Table 2. Concomitant administration of nemonoxacin with ferrous sulfate significantly reduced the absorption of nemonoxacin because Cmax decreased by 57.0%, AUC0–∞ by 63.7%, and Ae by 59.7%. Concomitant administration of nemonoxacin with calcium carbonate had much weaker effects because the AUC0–∞ decreased by 17.8%, Cmax by 14.3%, and Ae by 18.4%.
Plasma concentration-time curves of nemonoxacin after a single oral dose of 500 mg nemonoxacin alone (E) or at the same time as ferrous sulfate (F) or calcium carbonate (G) in 12 Chinese healthy male volunteers. Data are presented as the arithmetic mean±SD.
Safety
The AE profile did not differ between volunteers who received nemonoxacin only or those who received nemonoxacin and metal-ion-containing drugs (Table 3 and 4). The most common reported AEs were blood uric acid increased and WBC count increased. For Study 1, a total of 13 AEs were reported by 7 volunteers. Two episodes of creatine phosphokinase increased (1 following administration of nemonoxacin only, 1 following administration of nemonoxacin 2 h before antacid) reported by the same subject were considered possibly related to the study drug. For Study 2, a total of 17 AEs were reported by 6 volunteers. Six episodes of blood uric acid increased reported by 3 volunteers (2 following administration of nemonoxacin only, 1 following administration of nemonoxacin with ferrous sulfate, and 1 following administration of nemonoxacin with calcium carbonate) and 1 episode of ALT increased reported by 1 volunteer following administration of nemonoxacin only were considered possibly related to study drug. One volunteer experienced bacterial arthritis 13 d after nemonoxacin administration, and underwent open drainage of the knee joint and anti-rheumatic therapy. This event was classified as a serious AE, but was considered not related to the study drug. Except for this event, most AEs in both studies were classified as mild to moderate in severity, and recovered without treatment. There were no clinically important changes in vital signs nor were there any ECG abnormalities. None of the volunteers withdrew from the study because of an AE. Therefore, nemonoxacin was tolerated well when administered alone or in combination with drugs containing metal ions.
Discussion
The chelation of polyvalent metal ions by quinolones is a well-known interaction, and may result in lower plasma concentrations of quinolones, and could lead to therapeutic failure17. The extent of this interaction varies between quinolones and metal ions. Al3+ was reported to have the greatest chelation potential, and aluminum hydroxide markedly reduced the absorption of norfloxacin by 97.3%, ciprofloxacin by 85%, enoxacin by 84%, and ofloxacin by 53%, respectively9,14. The relative bioavailability of gatifloxacin was decreased by 64% when it was concomitantly administered with Maalox, a formulation of aluminum hydroxide and magnesium hydroxide13. In Study 1, we used Alumina, Magnesia and Dimethicone Chewable Tablets, which contained similar amounts of Al3+ and Mg2+ to Maalox, a drug that is not available in China. Like the quinolone antibiotics mentioned above, the absorption of nemonoxacin was significantly decreased when it was concomitantly administered with the metal ions Al3+ and Mg2+. Fortunately, this interaction was absent when it was administered 2 h before the Al3+- and Mg2+-containing antacid. This lack of effect may be due to the relatively rapid absorption of nemonoxacin (Tmax=1 h), which ensures that its absorption was complete before the antacid was administered. However, it is less clear why administration of the Al3+- and Mg2+-containing antacid 4 h before nemonoxacin significantly reduced nemonoxacin exposure but was accompanied by very large inter-individual variability. Of note, the absorption of nemonoxacin was hardly affected in five volunteers, but was decreased by >80% in seven volunteers. There were no protocol violations or important deviations during the study, and no procedural errors were found in a retrospective analysis. Considering that the principle mechanism for the interaction involves chelation of metal ions by quinolones, the persistence of these metal ions in the gastrointestinal tract appears to be a decisive factor when they are administered before the quinolone. The main ingredient of the antacid used in this study was dried aluminum hydroxide, which neutralizes gastric acid and protects the gastrointestinal mucosa. Its pharmacologic properties are dependent on the gastric emptying time. In our study, to ensure that nemonoxacin was administered to each volunteer at the same time (approximately 07:00 h), the antacid was administered at approximately 03:00 h in treatment B, after which the volunteers stayed in bed until 06:30 h. It is possible that the physiological condition (ie awake or asleep) during this period might affect gastric emptying time18,19, and hence retain the metal ions in the stomach for longer. This mechanism might explain the variability in the effects of administering the antacid 4 h before nemonoxacin. Based on the results in this study, we do not recommend that nemonoxacin is administered after an Al3+- and Mg2+-containing antacid.
The effects of ferrous sulfate and calcium carbonate on the absorption of nemonoxacin were evaluated in Study 2. Compared with the Al3+- and Mg2+-containing antacid, ferrous sulfate caused a less reduction in the absorption of nemonoxacin because Cmax and AUC0–∞ decreased by 57.0% and 63.7%, respectively. By contrast, calcium carbonate had much weaker effects because Cmax and AUC0–∞ decreased by 14.3% and 17.8%, respectively, and these decreases may not be clinically meaningful. It has been reported that for many quinolone drugs, the effects of metal ions are reduced markedly by their administration 2 h after quinolones intake12,13,20. In Study 1, the decreases in AUC0–∞ and Ae of nemonoxacin were less than 10%, when Al3+- and Mg2+-containing antacid was administered 2 h after nemonoxacin. Although we did not examine the time-dependent effects of ferrous sulfate, based on the mechanism of interaction, the results in Study 1, and the reports mentioned above, the influence of ferrous sulfate might not be larger than Al3+- and Mg2+-containing antacid when it was administered 2 h after nemonoxacin. There was no change in parameters T1/2 and CLr of nemonoxacin when administered with Al3+- and Mg2+-containing antacid, ferrous sulfate or calcium carbonate, which indicates that these metal ions have no influences on the elimination of nemonoxacin.
In conclusion, the results of the present studies indicate that Al3+, Mg2+, and Fe2+ significantly decreased the absorption of nemonoxacin when they were co-administered with nemonoxacin. To avoid the effects of Al3+ and Mg2+ containing drugs, nemonoxacin should be administered ≥2 h before them. Ca2+ had much weaker effects on the absorption of nemonoxacin that may not be clinically meaningful.
Author contribution
Yi-fan ZHANG designed research, analyzed data, and wrote the paper. Da-fang ZHONG, Xiao-yan CHEN, Ting WANG, Cheng-yuan TSAI, and Li-wen CHANG designed research. Xiao-jian DAI, Li LIANG, Hua QIAO, Ping-ting HUANG, Chiung-yuan HSU, Yu-ting CHANG, and Chen-en TSAI performed research.
References
Roychoudhury S, Ledoussal B . Non-fluorinated quinolones (NFQs): new antibacterials with unique properties against quinolone-resistant gram-positive pathogens. Curr Drug Targets Infect Disord 2002; 2: 51–65.
Adam HJ, Laing NM, King CR, Lulashnyk B, Hoban DJ, Zhanel GG . In vitro activity of nemonoxacin, a novel nonfluorinated quinolone, against 2,440 clinical isolates. Antimicrob Agents Chemother 2009; 53: 4915–20.
Chen YH, Liu CY, Lu JJ, King CH, Hsueh PR . In vitro activity of nemonoxacin (TG-873870), a novel non-fluorinated quinolone, against clinical isolates of Staphylococcus aureus, enterococci and Streptococcus pneumoniae with various resistance phenotypes in Taiwan. J Antimicrob Chemother 2009; 64: 1226–9.
Lauderdale TL, Shiau YR, Lai JF, Chen HC, King CH . Comparative in vitro activities of nemonoxacin (TG-873870), a novel nonfluorinated quinolone, and other quinolones against clinical isolates. Antimicrob Agents Chemother 2010; 54: 1338–42.
Chung DT, Tsai CY, Chen SJ, Chang LW, King CH, Hsu CH, et al. Multiple-dose safety, tolerability, and pharmacokinetics of oral nemonoxacin (TG-873870) in healthy volunteers. Antimicrob Agents Chemother 2010; 54: 411–7.
Guo B, Wu X, Zhang Y, Shi Y, Yu J, Cao G, et al. Safety and clinical pharmacokinetics of nemonoxacin, a novel non-fluorinated quinolone, in healthy Chinese volunteers following single and multiple oral doses. Clin Drug Investig 2012; 32: 475–86.
Lin L, Chang LW, Tsai CY, Hsu CH, Chung DT, Aronstein WS, et al. Dose escalation study of the safety, tolerability, and pharmacokinetics of nemonoxacin (TG-873870), a novel potent broad-spectrum nonfluorinated quinolone, in healthy volunteers. Antimicrob Agents Chemother 2009; 54: 405–10.
van Rensburg DJ, Perng RP, Mitha IH, Bester AJ, Kasumba J, Wu RG, et al. Efficacy and safety of nemonoxacin versus levofloxacin for community-acquired pneumonia. Antimicrob Agents Chemother 2010; 54: 4098–106.
Frost RW, Lasseter KC, Noe AJ, Shamblen EC, Lettieri JT . Effects of aluminum hydroxide and calcium carbonate antacids on the bioavailability of ciprofloxacin. Antimicrob Agents Chemother 1992; 36: 830–2.
Polk RE, Healy DP, Sahai J, Drwal L, Racht E . Effect of ferrous sulfate and multivitamins with zinc on absorption of ciprofloxacin in normal volunteers. Antimicrob Agents Chemother 1989; 33: 1841–84.
Shiba K, Sakai O, Shimada J, Okazaki O, Aoki H, Hakusui H . Effects of antacids, ferrous sulfate, and ranitidine on absorption of DR-3355 in humans. Antimicrob Agents Chemother 1992; 36: 2270–4.
Stass H, Böttcher MF, Ochmann K . Evaluation of the influence of antacids and H2 antagonists on the absorption of moxifloxacin after oral administration of a 400 mg dose to healthy volunteers. Clin Pharmacokinet 2001; 40 (Suppl 1): 39–48.
Lober S, Ziege S, Rau M, Schreiber G, Mignot A, Koeppe P, et al. Pharmacokinetics of gatifloxacin and interaction with an antacid containing aluminum and magnesium. Antimicrob Agents Chemother 1999; 43: 1067–71.
Mizuki Y, Fujiwara I, Yamaguchi T . Pharmacokinetic interactions related to the chemical structures of fluoroquinolones. J Antimicrob Chemother 1996; 37 (Suppl A): 41–55.
Miyata K, Ohtani H, Tsujimoto M, Sawada Y . Antacid interaction with new quinolones: dose regimen recommendations based on pharmacokinetic modeling of clinical data for ciprofloxacin, gatifloxacin and norfloxacin and metal cations. Int J Clin Pharmacol Ther 2007; 45: 63–70.
Uivarosi V . Metal complexes of quinolone antibiotics and their applications: an update. Molecules 2013; 18: 11153–97.
Mallet L, Huang A . Coadministration of gatifloxacin and multivitamin preparation containing minerals: potential treatment failure in an elderly patient. Ann Pharmacother 2005; 39: 150–2.
Pasricha PJ . Effect of sleep on gastroesophageal physiology and airway protective mechanisms. Am J Med 2003; 115 Suppl 3A: 114S–8S.
Orr WC, Heading R, Johnson LF, Kryger M . Review article: sleep and its relationship to gastro-oesophageal reflux. Aliment Pharmacol Ther 2004; 20 Suppl 9: 39–46.
Allen A, Bygate E, Faessel H, Isaac L, Lewis A . The effect of ferrous sulphate and sucralfate on the bioavailability of oral gemifloxacin in healthy volunteers. Int J Antimicrob Agents 2000; 15: 283–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Yf., Dai, Xj., Wang, T. et al. Effects of an Al3+- and Mg2+-containing antacid, ferrous sulfate, and calcium carbonate on the absorption of nemonoxacin (TG-873870) in healthy Chinese volunteers. Acta Pharmacol Sin 35, 1586–1592 (2014). https://doi.org/10.1038/aps.2014.95
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2014.95