Abstract
Aim:
Sustained pulmonary vasoconstriction as experienced at high altitude can lead to pulmonary hypertension (PH). The main purpose of this study is to investigate the vasorelaxant effect of echinacoside (ECH), a phenylethanoid glycoside from the Tibetan herb Lagotis brevituba Maxim and Cistanche tubulosa, on the pulmonary artery and its potential mechanism.
Methods:
Pulmonary arterial rings obtained from male Wistar rats were suspended in organ chambers filled with Krebs-Henseleit solution, and isometric tension was measured using a force transducer. Intracellular Ca2+ levels were measured in cultured rat pulmonary arterial smooth muscle cells (PASMCs) using Fluo 4-AM.
Results:
ECH (30–300 μmol/L) relaxed rat pulmonary arteries precontracted by noradrenaline (NE) in a concentration-dependent manner, and this effect could be observed in both intact endothelium and endothelium-denuded rings, but with a significantly lower maximum response and a higher EC50 in endothelium-denuded rings. This effect was significantly blocked by L-NAME, TEA, and BaCl2. However, IMT, 4-AP, and Gli did not inhibit ECH-induced relaxation. Under extracellular Ca2+-free conditions, the maximum contraction was reduced to 24.54%±2.97% and 10.60%±2.07% in rings treated with 100 and 300 μmol/L of ECH, respectively. Under extracellular calcium influx conditions, the maximum contraction was reduced to 112.42%±7.30%, 100.29%±8.66%, and 74.74%±4.95% in rings treated with 30, 100, and 300 μmol/L of ECH, respectively. After cells were loaded with Fluo 4-AM, the mean fluorescence intensity was lower in cells treated with ECH (100 μmol/L) than with NE.
Conclusion:
ECH suppresses NE-induced contraction of rat pulmonary artery via reducing intracellular Ca2+ levels, and induces its relaxation through the NO-cGMP pathway and opening of K+ channels (BKCa and KIR).
Similar content being viewed by others
Introduction
Sustained pulmonary vasoconstriction as experienced at high altitude can lead to pulmonary hypertension (PH) and medial hypertrophy1, which have been identified as the main cause of right ventricular hypertrophy and heart failure2. Individuals living at high altitude, either temporarily or permanently, may present mild to moderate pulmonary hypertension, and those with greater susceptibility to hypoxia may have exaggerated pulmonary vasoconstriction, leading to various high-altitude diseases that are associated with significant morbidity and mortality, such as high-altitude pulmonary edema and heart diseases3. Echinacoside (ECH) (Figure 1) is a phenylethanoid glycoside found in a variety of Chinese herbs such as the Tibetan herb Lagotis brevituba Maxim and Cistanche tubulosa4,5. Lagotis brevituba Maxim is a species of Lagotis spp belonging to the Scrophulariaceae and grows widely at an altitude over 3000 meter in the Qinghai-Tibet Plateau. ECH has various desirable pharmacological characteristics, such as antioxidative, anti-inflammatory, neuroprotective, hepatoprotective, and nitric oxide (NO) radical-scavenging properties6. It can also elicit endothelium-dependent relaxation in rat thoracic aortic rings and cure cardiovascular diseases7. However, to the best of our knowledge, there has not been a study investigating its effects on the vascular tone in pulmonary arteries.
The chemical structure of echinacoside.
The purposes of this study are as follows: (1) to explore whether ECH induces in vitro vasorelaxation in rat pulmonary arteries precontracted with noradrenaline (NE), and whether this effect, if any, is endothelium-dependent or acts directly upon vascular smooth muscle; (2) to investigate the effect of ECH on the extracellular calcium influx and intracellular calcium release in rat pulmonary arterial smooth muscle cells (PASMCs); and (3) to identify possible pathways and K+ channels involved in ECH-induced relaxation.
Materials and methods
Reagents
ECH was kindly provided by Dr Peng-fei TU of Peking University (Beijing, China), with a purity of more than 98% as determined by high-performance liquid chromatography. Dimethyl sulfoxide (DMSO) was purchased from Solarbio Science & Technology Co, Ltd (Beijing, China); NE, acetylcholine (ACh, ≥99%), indomethacin (IMT), Nω-Nitro-L-arginine methyl ester hydrochloride (L-NAME), tetraethylammonium chloride (TEA), barium chloride (BaCl2), 4-aminopyridine (4-AP), and glibenclamide (Gli) from Sigma Chemical Co (St Louis, MO, USA); high-glucose Dulbecco's modified Eagle's medium (DMEM), fetal bovine serum (FBS), and trypsin from Gibco BRL Co, Ltd (Gaithersburg, MD, USA); mouse anti-rat primary α smooth muscle actin (α-SMA) antibody and goat anti-mouse secondary antibody from Boshide Biotech Co, Ltd (Wuhan, China); Fluo Calcium Indicators (Fluo 4-AM) from Invitrogen Corp (Carlsbad, CA, USA); and all inorganic salts from Beijing Chemical Reagent Co, Ltd (Beijing, China). IMT was dissolved in DMSO and 5% NaH2PO4, Gli, Fluo 4-AM, and ECH were dissolved in DMSO, and all other reagents were dissolved in Krebs-Henseleit (KH) or PBS solution. Preliminary experiments showed that DMSO at less than 0.1% (v /v) had no effect on the tension development of isolated pulmonary arterial rings.
Experimental animals
All procedures and protocols were approved by the Animal Care and Use Committee of the Medical College of Qinghai University. Male Wistar rats, 6–8 weeks old, 250–300 g body weight, were purchased from the Animal Center of Lanzhou University (Lanzhou, China) and maintained on a standard laboratory diet and tap water ad libitum at an ambient temperature of 22±2 °C and a relative humidity of 45%–55% throughout the experiments.
In vitro pulmonary artery perfusion
Preparation of rat pulmonary arterial rings
Rats weighing 250–300 g were anesthetized by intraperitoneal injection of sodium pentobarbital (40 mg/kg), and then their hearts and lungs were removed and immersed immediately in ice-cold KH solution containing (in mmol/L): 118 NaCl, 4.7 KCl, 2.5 CaCl2, 1.2 MgSO4·7H2O, 1.2 KH2PO4, 25 NaHCO3, and 11.1 glucose (pH 7.4). The intrapulmonary arteries (0.7–1.5 mm in diameter) were dissected free of surrounding connective tissue and adventitia and then cut into rings of approximately 2–3 mm in length. The rings were suspended in organ chambers filled with 10 mL of KH solution at 37 °C and gassed with 95% O2–5% CO28, and isometric tension was measured using a force transducer (JH-2, Space Medico-Engineering Institute, Beijing, China).
Vessel ring activity assessment and endothelial function assessment
Vessel rings were allowed to equilibrate for 2 h under a basal tension of 400 mg, during which time the KH solution was changed every 15 min; then 1 μmol/L of NE was added into the chamber to assess the activity of each ring by detecting contraction percentage. Before and after the experimental protocol, the contraction percentage was measured (Figure 2A and 2B). Endothelium was removed in some rings by gently rubbing the intimal surface with a fine steel wire, and the integrity was assessed qualitatively by the degree of relaxation caused by ACh (10 μmol/L) in the percentage of contractile tone induced by NE (1 μmol/L). If the relaxation with ACh was greater than 80%, the endothelium remained in good condition; if the relaxation was less than 30%, the endothelium was destroyed (Figure 2A and 2B)9.
The vasorelaxant effects of ECH on E+ and E− pulmonary arterial rings. Representative curve of echinacoside-induced (300 μmol/L) relaxant effects on E+ (A) and E− (B) rings (n=8); (C) ECH dilated the vessels in a concentration-dependent manner in both E+ and E− pulmonary arterial rings. However, the effect was significantly reduced in the E− group (cP<0.01 vs E+).


Isolation and culture of rat PASMCs10
Distal pulmonary arteries were isolated from pulmonary lobes of rats, and the endothelium and adventitia were removed carefully. After tissues were minced into 2-mm pieces, they were added to the flasks immediately, maintained at 37 °C and 5% CO2 in a humidified incubator for approximately four hours, and then cultured with high-glucose DMEM supplemented with 20% FBS, 100 U/mL of penicillin and 100 U/mL of streptomycin for approximately five days. Half of the culture media was replaced with fresh media when cells emerged. When cells reached 80% confluence, they were harvested with 0.125% trypsin and seeded into the flasks (1:2 ratio) containing high-glucose DMEM supplemented with 10% FBS, 100 U/mL of penicillin and 100 U/mL of streptomycin. Cells with three to eight passages were used for all experiments.
Identification of PASMCs by immunohistochemistry10
PASMCs were positive for immunochemical staining when typical “hill and valley” features were observed. Cells were seeded in 6-well plates with glass coverslips. When cells reached 80% confluence, they were fixed in 4% paraformaldehyde, blocked with 3% hydrogen peroxide for 15 min, and then incubated with mouse anti-rat primary α-SMA antibody overnight at 4 °C. After being washed three times in PBS for 10 min, cells were incubated with goat anti-mouse secondary antibody at room temperature for 45 min, washed again three times in PBS for 10 min, and visualized with diaminobenzidine.
Detection of the intracellular calcium concentration in rat PASMCs
PASMCs were seeded in 6-well plates with glass coverslips. When cells reached 80% confluence, the culture media were replaced with serum-free DMEM. Twenty-four hours later, cells were loaded with 7 μmol/L Fluo 4-AM at 37 °C for 30 min in a humidified atmosphere of 5% CO2. The residual dye was washed with Hanks' Balanced Salt Solution (HBSS) solution containing the following (in mmol/L): 1.26 CaCl2, 0.49 MgCl2·6H2O, 0.41 MgSO4·7H2O, 5.33 KCl, 0.44 KH2PO4, 4.17 NaHCO3, 137.93 NaCl, 0.34 Na2HPO4, and 5.56 D-Glucose, with no phenol red. Cells loaded with Fluo 4-AM were exposed to one of three treatment conditions: (1) the control group (con group), in which cells were incubated with serum-free DMEM; (2) the NE group, in which cells were incubated with serum-free DMEM supplemented with 1 μmol/L of NE for 10 min; and (3) the NE+ECH (100 μmol/L) group (NE+ECH100 group), in which cells were incubated with serum-free DMEM supplemented with 1 μmol/L of NE for 10 min and 100 μmol/L of ECH for 20 min. Fluorescence intensity was observed and photographed by fluorescence microscopy (IX71, Olympus, Tokyo, Japan)11. Six fields of vision (200×) were collected for each sample. Intracellular calcium concentration was quantified by measuring mean fluorescence intensity using Image Pro-Plus 6.0 software.
Statistical analysis
Data were expressed as the mean±SD. When appropriate, significant difference was assessed by Dunnett's test or the Student-Newman-Keuls test for multiple comparisons after one-way analysis of variance (ANOVA). A probability level of P<0.05 was considered significant.
Results
Vasorelaxant effects of ECH on isolated pulmonary artery
At the beginning of the experiment, the cumulative addition of ECH from 30 to 300 μmol/L had no significant effect on the basal tension of the pulmonary artery. After the NE-induced vasoconstriction reached a plateau, ECH was added cumulatively (30–300 μmol/L) to the intact endothelium (E+, Figure 2C) or endothelium-denuded rings (E−, Figure 2C). In intact endothelium rings, cumulative addition of ECH dilated the vessels in a concentration-dependent manner, with a maximum relaxation percentage of 89.22%±0.32% at 300 μmol/L and an EC50 of 51.60±0.57 μmol/L (Figure 2A and 2C). Similarly, in endothelium-denuded rings, ECH also dilated the vessels in a concentration-dependent manner, but with a significantly lower maximum response of 67.72%±1.69% (P<0.01 vs intact endothelium rings) and a higher EC50 of 108.51±2.8 μmol/L (P<0.01 vs intact endothelium rings, Figure 2B and 2C). The sustained plateau of the high-contraction percentage induced by NE (1 μmol/L) after the experimental protocol indicated that the rings pretreated with ECH (30–300 μmol/L) had good activity (Figure 2A and 2B).
Effects of ECH on intracellular calcium release and extracellular calcium influx
The endothelium-denuded rings were exposed to 1 μmol/L of NE until the maximum contraction was attained. Under extracellular Ca2+-free conditions, the rings were equilibrated in Ca2+-free KH solution containing 0.2 mmol/L of EGTA before the initiation of the experiments. Following three washes with Ca2+- and EGTA-free KH solution, the rings were pre-incubated with ECH (30, 100, and 300 μmol/L) for 20 min and then re-exposed to 1 μmol/L of NE. The rings produced unsustained contractions that rapidly returned to baseline, compared with the initial contractions induced by NE, which served as the reference. The maximum contraction of the control was 33.27%±2.94% (Figure 3A and 3E) but was significantly reduced to 24.54%±2.97% and 10.60%±2.07% in rings pretreated with 100 and 300 μmol/L of ECH, respectively (P<0.01 vs control group; Figure 3C–3E). Under extracellular calcium influx conditions, 2.5 mmol/L CaCl2 was added to the chamber when the curve reached a plateau. The control group produced sustained contractions, with a maximum contraction of 139.89%±7.38% (Figure 3A and 3E); but the maximum contraction was significantly reduced to 112.42%±7.30%, 100.29%±8.66%, and 74.74%±4.95% in rings pretreated with 30, 100, and 300 μmol/L of ECH, respectively (P<0.01 vs control group; Figure 3B–3E). Under these conditions, the maximal effect caused by ECH was more pronounced with 300 μmol/L than with 100 or 30 μmol/L (P<0.01 vs 30 or 100 μmol/L ECH group). Different concentrations of ECH all shortened the platform of sustained contraction, which was induced by extracellular calcium influx at different levels (Figure 3A–3D).
The effects of ECH on intracellular calcium release and extracellular calcium influx. (A) Under extracellular Ca2+-free conditions, 1 μmol/L of NE induced short and small contraction (intracellular calcium release), and the addition of 2.5 mmol/L CaCl2 resulted in extracellular calcium influx and sustained contraction (control, n=8); (B–D) The effects of ECH (30, 100, and 300 μmol/L) on intracellular calcium release and extracellular calcium (n=8). (E) Under extracellular Ca2+-free conditions, the maximum contraction was significantly reduced to 24.54%±2.97% and 10.60%±2.07% in rings treated with 100 and 300 μmol/L of ECH, respectively (P<0.01 vs control). Under extracellular calcium influx conditions, it was reduced to 112.42%±7.30%, 100.29%±8.66%, and 74.74%±4.95% in rings treated with 30, 100, and 300 μmol/L of ECH, respectively (P<0.01 vs control). Additionally, the effect was more pronounced with 300 μmol/L of ECH (cP<0.01 vs control, fP<0.01 vs 30 μmol/L ECH, iP<0.01 vs 100 μmol/L ECH).
Roles of different inhibitors in ECH-induced rat pulmonary artery vasorelaxation
ECH-induced rat pulmonary artery vasorelaxation was investigated in the presence or absence of the following inhibitors: L-NAME (eNOS inhibitor), IMT (cyclooxygenase inhibitor), TEA (large-conductance Ca2+-activated K+ channel inhibitor), BaCl2 (inward rectifier K+ channel inhibitor), 4-AP (voltage-dependent K+ channel inhibitor), and Gli (ATP-sensitive K+ channel inhibitor). The rings were maximally contracted with 1 μmol/L of NE, and then L-NAME (100 μmol/L), IMT (10 μmol/L), TEA (1 mmol/L), BaCl2 (1 mmol/L), 4-AP (1 mmol/L), or Gli (10 μmol/L) were added, respectively. Once a new plateau was reached, ECH was added in a cumulative manner from 30 to 300 μmol/L. The concentration–response curves in the presence of different inhibitors are shown in Figure 4. The vasorelaxant effect of ECH on pulmonary arterial rings contracted with 1 μmol/L of NE was significantly blocked by L-NAME (100 μmol/L), TEA (1 mmol/L), and BaCl2 (1 mmol/L), with maximum relaxations of 64.41%±3.20%, 84.38%±0.70%, and 75.27%±0.93%, respectively (P<0.01 vs the control group of 89.22%±0.32%), and the values of EC50 were increased to 197.32±2.75 μmol/L, 91.42±2.11 μmol/L, and 115.49±1.75 μmol/L, respectively (P<0.01 vs the control group of 51.60±0.57 μmol/L) (Table 1). However, IMT (10 μmol/L), 4-AP (1 mmol/L), and Gli (10 μmol/L) did not inhibit the ECH-induced relaxation (Figure 4 and Table 1).
The roles of different inhibitors in ECH-induced rat pulmonary artery vasorelaxation (n=8). The rings were maximally contracted with 1 μmol/L of NE, and then L-NAME (100 μmol/L), IMT (10 μmol/L), TEA (1 mmol/L), BaCl2 (1 mmol/L), 4-AP (1 mmol/L), or Gli (10 μmol/L) were added. Once a new plateau was reached, ECH was added in a cumulative manner from 30 to 300 μmol/L. The concentration-response curves in the absence or presence of different inhibitors are shown. The vasorelaxant effect of ECH was significantly blocked by L-NAME (100 μmol/L), TEA (1 mmol/L), and BaCl2 (1 mmol/L), with a maximum relaxation of 64.41%±3.20%, 84.38%±0.70%, and 75.27%±0.93%, respectively (cP<0.01 vs control group of 89.22%±0.32%), and the concentration-response curves all shifted up. However, IMT (10 μmol/L), 4-AP (1 mmol/L), and Gli (10 μmol/L) did not inhibit ECH-induced relaxation.
To validate the effects of these inhibitors on ECH-induced relaxation, the rings precontracted with 1 μmol/L of NE were treated with L-NAME (100 μmol/L), IMT (10 μmol/L), TEA (1 mmol/L), BaCl2 (1 mmol/L), 4-AP (1 mmol/L), and Gli (10 μmol/L). After a new plateau was reached, ECH was added to the chamber at a single concentration of 300 μmol/L rather than in a cumulative manner. The maximum relaxation was reduced to 56.33%±0.90%, 82.21%±0.92%, and 72.16%±0.76% following the addition of L-NAME, TEA, and BaCl2, respectively (P<0.01 vs the control group of 91.16%±0.55%) (Figure 5A, 5B, 5D, 5F, and 5H). However, IMT, 4-AP, and Gli did not inhibit the ECH-induced relaxation (Figure 5A, 5C, 5E, 5G, and 5H).
The effects of different inhibitors on ECH (300 μmol/L)-induced rat pulmonary artery vasorelaxation (n=8). (A) Control group ECH (300 μmol/L), (B) L-NAME (100 μmol/L), (C) IMT (10 μmol/L), (D) TEA (1 mmol/L), (E) Gli (10 μmol/L), (F) BaCl2 (1 mmol/L), or (G) 4-AP (1 mmol/L) was applied to the rings precontracted with 1 μmol/L of NE (control). (H) The maximum relaxation was reduced to 82.21%±0.92%, 56.33%±0.90%, and 72.16%±0.76% following the addition of TEA, L-NAME, and BaCl2, respectively (cP<0.01 vs the control). However, IMT, 4-AP, and Gli did not inhibit ECH-induced relaxation (P>0.05 vs control, cP<0.01 vs control).
Identification of rat PASMCs
At low magnification, spindle cells were densely packed, and almost all of cells were stained positively for PASMCs (the PASMC purity was >95%) (Figure 6A). Brown-stained myofilaments were clearly observed in the cytoplasm at high magnification (Figure 6B).
Identification of PASMCs by immunohistochemistry. (A) At low magnification, spindle cells were densely packed, almost all of cells were positive for PASMCs (the PASMC purity was >95%). (B) Brown-stained myofilaments were clearly observed in the cytoplasm at high magnification.
Effect of ECH on the intracellular calcium concentration in rat PASMCs
NE (1 μmol/L) significantly increased the intracellular calcium concentration (n=6, P<0.01 vs the control group) in rat PASMCs, and ECH could decrease the mean fluorescence intensity (n=6, P<0.01 vs the NE group) (Figure 7).
The effect of ECH on the intracellular calcium concentration in rat PASMCs. (A) The image of intracellular calcium fluorescence (200× and 400×). (B) NE (1 μmol/L) significantly increased the intracellular calcium concentration (n=6. cP<0.01 vs the control group) in rat PASMCs, and ECH could decrease the mean fluorescence intensity (n=6. fP<0.01 vs the NE group).
Discussion
To the best of our knowledge, this is the first study evaluating the effect of ECH on the vascular tone of the rat pulmonary artery. We found that ECH induced vasorelaxation of rat pulmonary artery precontracted with NE in a concentration-dependent manner, and such effects can be observed in both intact endothelium and endothelium-denuded rings. In the pulmonary artery, ECH attenuated both extracellular calcium influx and intracellular calcium release, and the NO-cGMP pathway and the opening of K+ channels (large conductance Ca2+-activated K+ channels and inward rectifier K+ channels) appeared to play a role in ECH-induced rat pulmonary artery vasorelaxation. In rat PASMCs, ECH could reduce intracellular calcium concentration directly. Previous studies have also suggested that ECH could mediate the endothelium-dependent vasodilator action in rat thoracic aortic rings through the NO-cGMP pathway7.
ECH-induced vasorelaxation can be observed in both intact endothelium and endothelium-denuded rings. However, removal of endothelium resulted in a significant reduction in maximum response and an increase in the EC50 relative to the intact endothelium rings. It has been suggested that NO-cGMP and PGI2-cAMP pathways play a key role in regulating endothelium-dependent vascular relaxation9. To explore this issue, we added 100 μmol/L of L-NAME, an inhibitor of NO synthesis into endothelial cells. The results showed that L-NAME significantly attenuated the vasodilation of ECH, suggesting that NO is likely to play a role in the vasorelaxation of ECH. We also found that IMT, an inhibitor of cyclooxygenase (a key PGI2 synthetase), had no such effect, indicating that PGI2 was unlikely to be involved in the vasorelaxation of ECH. Therefore, ECH may enhance NO production from L-arginine in vascular endothelium and activated guanylate cyclase, thus catalyzing the conversion of GTP to cGMP. After the experimental protocol, the rings showed the sustained plateau of high contraction percentage induced by NE (1 μmol/L), which indicated that the rings pretreated with ECH (30 to 300 μmol/L) displayed good activity (Figure 2A and 2B).
Vascular tone is regulated by intracellular Ca2+12. We found that ECH (100 and 300 μmol/L) significantly reduced the phasic contraction induced by NE in endothelium-denuded pulmonary arterial rings in Ca2+-free KH solution, and this effect was more pronounced with the higher concentration of ECH (300 μmol/L), indicating that the inhibitory effect of ECH on the NE-induced contraction of pulmonary arterial rings was mediated by interference in the ability of IP3 to promote the release of intracellular Ca2+. NE acts on the α-receptor to mediate vascular contraction, thus increasing intracellular Ca2+ levels ([Ca2+]i) through the G-protein coupled phosphatidylinositol signal transduction pathway13. Once being activated, this triggers the formation of the second messenger IP3 and diacylglycerol induced by phospholipase C14. IP3 can rapidly mobilize and release Ca2+ from the sarcoplasmic reticulum to cause a transient increase in [Ca2+]i, which could be associated with the NE-induced phasic contraction in pulmonary arterial rings in Ca2+-free medium.
To investigate the effect of ECH on the extracellular calcium influx, CaCl2 (2.5 mmol/L) was added under Ca2+-free conditions. The addition of ECH (30, 100, and 300 μmol/L) significantly reduced the maximum contraction, with the most significant effect observed with 300 μmol/L ECH. This suggested that ECH inhibits intracellular calcium release and extracellular calcium influx in PASMCs. However, further studies are needed to elucidate the relationship between ECH and inhibitors of L-type calcium channels.
To investigate the role of calcium, Fluo 4-AM was used to determine intracellular calcium concentrations in rat PASMCs. Because the addition of NE (1 μmol/L) resulted in a rapid change in the tension of vessel rings (Figure 2), rat PASMCs were first loaded with Fluo 4-AM, and then NE and ECH were added. The results showed that 1 μmol/L NE could increase the intracellular calcium concentration, which was in agreement with previous studies, and the mean fluorescence intensity was lower in the NE+ECH100 group than in the NE group. Thus, it was concluded that ECH could reduce the intracellular calcium concentration in rat PASMCs pretreated with NE. Because it is preferable to detect intracellular calcium concentration in a real-time manner, further research is being conducted to observe the real-time changes of intracellular calcium concentration using confocal microscopy.
K+ channels contribute to the regulation of pulmonary vascular tone through cytoplasmic K+ and Ca2+ concentration and membrane potential. The opening of K+ channels leads to an efflux of K+ that causes the cell membrane to become hyperpolarized, leading to the closure of L-type calcium channels and the reduction of intracellular Ca2+15,16. In this study, we found that BaCl2 (an inhibitor of KIR channels) and TEA (an inhibitor of BKCa channels) remarkably reduced the vasorelaxant effect of ECH, indicating that the KIR and BKCa channels could be involved in this effect. However, 4-AP (an inhibitor of Kv channels) and Gli (a KATP inhibitor) had no such effect, indicating that the Kv or KATP channels were not involved.
BKCa channels, with seven transmembrane domains and a calcium-binding region (bowl), are somewhat structurally unique, even within the KCa family17,18. They are expressed widely in smooth muscle cells and play an important role in regulating vascular tone, which is activated by both membrane depolarization and intracellular calcium19,20,21. BKCa channels have also been proposed as potential therapeutic targets for cardiovascular diseases because of their ability to regulate vascular tone22,23. We found that TEA, an inhibitor of BKCa channels, caused the concentration-response curve to shift up and a significant increase in the EC50. We also found that the ECH-induced relaxation was significantly weaker at the highest concentration of ECH in rings after treatment with TEA (1 mmol/L) compared with the control. NO-induced vasodilation is due in part to a cGMP-dependent, protein kinase G-mediated activation of BKCa channels24. Therefore, we assumed that ECH induced rat pulmonary artery vasorelaxation via the NO-cGMP-PKG-BKCa channels, which led to a decrease in intracellular Ca2+ levels and the relaxation of PASMCs. An interesting observation was that different concentrations of ECH reduced the maximum contraction induced by extracellular calcium influx and shortened the sustained contraction, which may be related to the opening of BKCa channels.
KIR channels are the simplest channels, with only two transmembrane domains. They are involved in regulating the driving force for calcium entry in pulmonary vascular endothelial cells; therefore, they have been implicated in regulating vascular permeability25 and responses to shear stress26. In this study, we showed that the KIR inhibitor caused the concentration-response curve to shift up and a significant increase in EC50, and that ECH (300 μmol/L)-induced relaxation was significantly weaker compared with the control. All these results indicated that ECH had a vasorelaxant effect on the pulmonary artery via the KIR channels. However, given the complex role of K+ channels in regulating vascular tone, further studies are required to elucidate this issue. K+ channels have recently been suggested to participate in vascular remodeling by regulating cell proliferation and apoptosis18. Global hypoxia, as it occurs at high altitude, causes pulmonary vasoconstriction or vascular remodeling and increases pulmonary vascular resistance27. Impaired K+ channels (KATP, KCa, KV, and KIR) in vascular smooth muscle cells are also related to the development of hypertension22,28.
Hypoxic inhibition of K+ channels results in membrane depolarization, the activation of voltage-dependent Ca2+ (CaV) channels, extracellular Ca2+ influx and intracellular Ca2+ release, thus resulting in an increase in [Ca2+]i, followed by pulmonary vasoconstriction and proliferation of PASMCs29. Opening K+ channels contributes to the regulation of hypoxic pulmonary vasoconstriction and vascular remodeling. Thus, ECH may open the K+ channels, thereby attenuating hypoxic pulmonary vasoconstriction as well as reducing vascular remodeling.
Conclusion
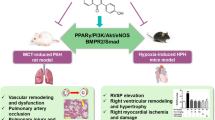
ECH induces vasorelaxation in rat pulmonary arteries precontracted with NE, and such an effect can be observed in both intact endothelium and endothelium-denuded rings. This is most likely related to the opening of the NO-cGMP-PKG-BKCa channels and the reduction of intracellular Ca2+ levels, thereby relaxing the PASMCs (Figure 8).
Graphical abstract. ECH induced vasorelaxation of rat pulmonary arteries precontracted with NE, and this effect could be observed in both intact endothelium and endothelium-denuded rings. In PASMCs, ECH attenuated both extracellular calcium influx and intracellular calcium release, which resulted in vasoconstriction; additionally, the NO-cGMP pathway and the opening of K+ channels (BKCa and KIR) appeared to play a major role in ECH-induced rat pulmonary artery vasorelaxation.
Author contribution
Ri-li GE and Xiang-yun GAI designed the study; Xiang-yun GAI, Yu-hai WEI, Ta-na WUREN, Ya-ping WANG, Zhan-qiang LI, and Yi ZHOU performed the research; Wei ZHANG and Yu-hai WEI contributed new reagents and analytical tools; Xiang-yun GAI and Shou LIU analyzed the data; Xiang-yun GAI wrote the paper; and Lan MA, Dian-xiang LU modified the paper.
References
Hultgren HN, editor. High Altitude Medicine. Stanford: Hultgren Publications; 1997.
Humbert M, Sitbon O, Simonneau G . Treatment of pulmonary arterial hypertension. N Engl J Med 2004; 351: 1425–36.
Ge RL . Life on the Qinghai-Tibetan Plateaus. Beijing: Peking University Medical Press; 2007. Chinese.
Xin Y, Hu F, Dong Q, Peng M . Determination of echinacoside and acteoside in Tibetan herb Lagotis brevituba Maxim. Chin J Pharm Anal 2012; 32: 1183–5.
Zhao Q, Gao J, Li W, Cai D . Neurotrophic and neurorescue effects of Echinacoside in the subacute MPTP mouse model of Parkinson's disease. Brain Res 2010; 1346: 224–36.
Yang XL, L F, Yang YN, Shen JY, Zou R, Zhu PP, et al. Efficacy and safety of echinacoside in a rat osteopenia model. Evid Based Complement Alternat Med 2013; 2013: 1–10.
He WJ, Fang TH, Ma X, Zhang K, Ma ZZ, Tu PF . Echinacoside elicits endothelium-dependent relaxation in rat aortic rings via an NO-cGMP pathway. Planta Med 2009; 75: 1400–4.
Warshaw DM, Mulvany MJ, Halpern W . Mechanical and morphological properties of arterial resistance vessels in young and old spontaneously hypertensive rats. Circ Res 1979; 45: 250–9.
Shen M, Zhao L, Wu RX, Yue SQ, Pei JM . The vasorelaxing effect of resveratrol on abdominal aorta from rats and its underlying mechanisms. Vascul Pharmacol 2012; 58: 64–70.
Gai XY, Tang F, MA J, Zeng KW, Wang SL, Wang YP, et al. Antiproliferative effect of echinacoside on rat pulmonary artery smooth muscle cells under hypoxia. J Pharmacol Sci 2014; 126: 155–63.
Mandal SK, Pendurthi UR, Rao LVM . Tissue factor trafficking in fibroblasts: involvement of protease-activated receptor-mediated cell signaling. Blood 2007; 110: 161–70.
Toque HA, Teixeira CE, Priviero FB, Morganti RP, Antunes E, De Nucci G . Vardenafil, but not sildenafil or tadalafil, has calcium-channel blocking activity in rabbit isolated pulmonary artery and human washed platelets. Br J Pharmacol 2008; 154: 787–96.
Fonseca-Magalhães PA, Sousa DF, de Siqueira RJ, Jorge RJ, Meneses GC, Alves RS, et al. Inhibitory effects of sertraline in rat isolated perfused kidneys and in isolated ring preparations of rat arteries. J Pharm Pharmacol 2011; 63: 1186–94.
Berridge MJ . Inositol trisphosphate and calcium signalling mechanisms. Biochim Biophys Acta 2009; 1793: 933–40.
Hu F, Koon CM, Chan JY, Lau KM, Kwan YW, Fung KP . Involvements of calcium channel and potassium channel in Danshen and Gegen decoction induced vasodilation in porcine coronary LAD artery. Phytomedicine 2012; 19: 1051–8.
Matsumoto T, Kobayashi T, Ishida K, Hirasawa Y, Morita H, Honda T, et al. Vasodilator effect of Cassiarin A, a novel antiplasmodial alkaloid from Cassia siamea, in rat isolated mesenteric artery. Biol Pharm Bull 2010; 33: 844–8.
Dubuis E, Potier M, Wang R, Vandier C . Continuous inhalation of carbon monoxide attenuates hypoxic pulmonary hypertension development presumably through activation of BKCa channels. Cardiovasc Res 2005; 65: 751–61.
Moudgil R, Michelakis ED, Archer SL . The role of K+ channels in determining pulmonary vascular tone, oxygen sensing, cell proliferation, and apoptosis: implications in hypoxic pulmonary vasoconstriction and pulmonary arterial hypertension. Microcirculation 2006; 13: 615–32.
Eichhorn B, Dobrev D . Vascular large conductance calcium-activated potassium channels: functional role and therapeutic potential. Naunyn Schmiedebergs Arch Pharmacol 2007; 376: 145–55.
Ko EA, Han J, Jung ID, Park WS . Physiological roles of K+ channels in vascular smooth muscle cells. J Smooth Muscle Res 2008; 44: 65–81.
Ledoux J, Werner ME, Brayden JE, Nelson MT . Calcium-activated potassium channels and the regulation of vascular tone. Physiology 2006; 21: 69–78.
Bonnet S, Archer SL . Potassium channel diversity in the pulmonary arteries and pulmonary veins: implications for regulation of the pulmonary vasculature in health and during pulmonary hypertension. Pharmacol Ther 2007; 115: 56–69.
Feletou M . Calcium-activated potassium channels and endothelial dysfunction: therapeutic options? Br J Pharmacol 2009; 156: 545–62.
Archer SL, Huang J, Hampl V, Nelson DP, Shultz PJ, Weir EK . Nitric oxide and cGMP cause vasorelaxation by activation of a charybdotoxin-sensitive K channel by cGMP-dependent protein kinase. Proc Natl Acad Sci U S A 1994; 91: 7583–7.
Shimoda LA, Welsh LE, Pearse DB . Inhibition of inwardly rectifying K+ channels by cGMP in pulmonary vascular endothelial cells. Am J Physiol Lung Cell Mol Physiol 2002; 283: L297–304.
Chatterjee S, Al-Mehdi AB, Levitan I, Stevens T, Fisher AB . Shear stress increases expression of a KATP channel in rat and bovine pulmonary vascular endothelial cells. Am J Physiol Lung Cell Mol Physiol 2003; 285: C959–67.
Bartsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O . Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med 1991; 325: 1284–9.
Park WS, Han J, Earm YE . Physiological role of inward rectifier K+ channels in vascular smooth muscle cells. Pflugers Arch 2008; 457: 137–47.
Wang YX, Zheng YM . ROS-dependent signaling mechanisms for hypoxic Ca2+ responses in pulmonary artery myocytes. Antioxid Redox Signal 2010; 12: 611–23.
Acknowledgements
We thank Liang YANG and her laboratory (Center for Mitochondrial Biology and Medicine, The Key Laboratory of Biomedical Information Engineering of Ministry of Education, School of Life Science and Technology and Frontier Institute of Science and Technology, Xi'an Jiaotong University, Xi'an 710049, China) for their help in detecting the intracellular calcium concentration of rat PASMCs.
This project is supported by the National Program on Key Basic Research Project of China (No 2012CB518200), the Program of International Science and Technology Cooperation of China (No 2011DFA32720), the National Natural Science Foundation of China (No 31160219), the Key Laboratories Development Program of Qinghai Province (No 2013-Z-Y05, No 2014-Z-Y-30, and No 2014-Z-Y-07), Qinghai-Utah Joint Research Key Lab for High Altitude Medicine, the National Natural Science Foundation of China (No 81160012), the Ministry of Education New Century Outstanding Talents Support Program of China (No NCET-12-1022) and the National Natural Science Foundation of Qinghai (No 2012-Z-915Q).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gai, Xy., Wei, Yh., Zhang, W. et al. Echinacoside induces rat pulmonary artery vasorelaxation by opening the NO-cGMP-PKG-BKCa channels and reducing intracellular Ca2+ levels. Acta Pharmacol Sin 36, 587–596 (2015). https://doi.org/10.1038/aps.2014.126
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2014.126
Keywords
This article is cited by
-
Molecular pathogenesis and current pathology of pulmonary hypertension
Heart Failure Reviews (2016)