Abstract
Aim:
To examine individual patient's demographic parameters and clinical variables related to return of consciousness (ROC) and the pharmacodynamic relationship between propofol effect-site concentration (Ce) and ROC from propofol-remifentanil anesthesia.
Methods:
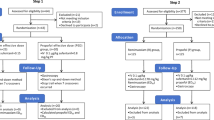
Ninety-four patients received propofol-remifentanil anesthesia using the effect-site target-controlled infusion (TCI) system. All clinical events were noted, and variables possibly related to propofol Ce at ROC were examined using linear correlation analyses. Pharmacodynamic modeling incorporating covariates was performed using NONMEM (Nonlinear Mixed Effects Modeling) VII software.
Results:
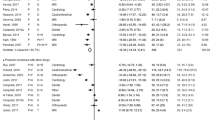
The Ce values of propofol at loss of consciousness (LOC) and ROC were 4.4±1.1 μg/mL and 1.1±0.3 μg/mL, respectively. Age was negatively correlated with propofol Ce at ROC (r=−0.48, P<0.01). Including age as a covariate in Ce50 (the effect-site concentration associated with 50% probability of return of consciousness) and λ (the steepness of the concentration-versus-response relationship) significantly improved the performance of the basic model based on the likelihood ratio test, with a significant decrease in the minimum value of the objective function. The Ce50 in 25-, 50-, and 75-year-old patients was predicted to be 1.38, 1.06, and 0.74 μg/mL, respectively. The λ in 25-, 50-, and 75-year-old patients was predicted to be 12.23, 8.70, and 5.18, respectively.
Conclusion:
Age significantly affects the relationship between propofol Ce and ROC, and pharmacodynamic modeling including age could lead to better predictions of ROC during emergence from propofol-remifentanil anesthesia.
Similar content being viewed by others
Introduction
Anesthesiologists are concerned not only about inducing rapid and safe anesthesia, but also about achieving a comfortable and precise return of consciousness (ROC) after surgery1. To date, studies have focused mainly on individual effects of anesthesia induction. The ability to predict the individual propofol effect-site concentration (Ce) for ROC would allow the dose of propofol to be adjusted to achieve an adequate ROC. It would also reduce the anesthesiologists workload, save time and resources, and allow for safer patient recovery2. Some studies of ROC show large variations (0.8–2.7 μg/mL) in propofol Ce producing ROC from anesthesia3, 4, making it difficult to predict the minimum concentration for effective sedation and the concentration of propofol during emergence. In the absence of individual pharmacodynamic information, propofol is usually dosed on the basis of the average population requirement. Hence pharmacodynamic modeling incorporating a population approach with covariates could be clinically useful for describing the dose-response relationship.
The objectives of our study were: 1) to identify the clinical variables related to the propofol Ce at ROC and 2) to apply a population pharmacodynamic modeling approach to data from propofol-remifentanil anesthesia.
Materials and methods
This study was approved by the ethics committee of the Yonsei University Health System (4-2010-0580). Patients (aged ≥ 20 years, ASA I–II) scheduled for elective minor surgery at the Eye and ENT Severance Hospital were included from January 2011 to September 2011. Exclusion criteria were as follows: cardiac, pulmonary, hepatic or renal disease; hearing loss or other neurological deficit; past history of allergy or adverse reaction to medication; any type of medication affecting the central nervous system; or body mass index more than 30. All of the patients provided written informed consent.
Anesthesia was induced according to the same standard protocol in all patients. Patients were premedicated iv with 0.1 mg of glycopyrrolate. Anesthesia was induced by effect-site target-controlled infusion (TCI) (Orchestra® Base Primea, Fresenius Vial, France) of propofol and remifentanil after the patients anthropometric data were entered. The pump was operated according to the model for propofol developed by Schnider et al5, 6 and the model for remifentanil developed by Minto et al7, 8. The initial target Ce values of propofol and remifentanil were 4 μg/mL and 2 ng/mL, respectively, for induction. Loss of consciousness (LOC) was defined as a patient's inability to open their eyes in response to their name being called loudly, ie, a score of 3 on the Observer's Assessment of Alertness/Sedation Scale (OAA/S)9. If LOC was not obtained with this initial Ce, the Ce of propofol was increased in increments of 0.5 μg/mL until LOC occurred. The remifentanil Ce was maintained at 2 ng/mL. Consciousness was assessed every 10 s. At the moment of LOC, the BIS index (BIS VISTA™, Aspect Medical System, Inc, Norwood, MA, USA) and the Ce of propofol and remifentanil were recorded. Rocuronium was given (0.6 mg/kg iv) as a neuromuscular blockade. After endotracheal intubation, ventilation was mechanically controlled with 50% oxygen in an air mixture to maintain the end-tidal carbon dioxide tension at 35 to 40 mmHg. After anesthesia was induced, the Ce of propofol was titrated to maintain BIS values between 40 and 60 throughout the intraoperative period. In addition, the Ce of remifentanil was adapted to intraoperative hemodynamics throughout the surgical procedure.
At the end of surgery, propofol and remifentanil infusion was stopped. The neuromuscular block was antagonized with 0.2 mg of glycopyrrolate and 1.0 mg of neostigmine. Return of consciousness was defined as a score of 3 on the OAA/S. At the end of surgery and at ROC, the BIS value and the Ce of propofol and remifentanil were recorded by an investigator blinded to the conditions. The total amount of propofol and remifentanil, duration of infusion, and the duration of anesthesia and surgery were also recorded. The duration of anesthesia was defined as the time from the start of propofol infusion for induction to extubation of the trachea; the duration of surgery was defined as the time from surgical incision to the application of the last suture. All of the patients were administered ramosetron (Astellas Pharma Inc, Tokyo, Japan) 0.3 mg and ketorolac (Hana Pharm Co, Seoul, Korea) 60 mg iv for the prevention of postoperative nausea, vomiting and pain in the operating room before the end of surgery.
Correlations between ROC and several clinical variables were determined by linear correlation analysis. Using the observed ROC, propofol Ce in the basic pharmacodynamic model was distributed between 0 (unconscious) or 1 (conscious). The relationship between the probability of ROC and the propofol Ce was analyzed using a sigmoidal Emax model:

where P is the probability of ROC from anesthesia, Ce50 is the Ce associated with 50% probability of ROC, and λ is the steepness of the concentration-versus-response relationship.
The likelihood, L, of the observed response, R(unconscious=0, conscious=1) is described by the following equation:

where P is the probability of ROC.
Model parameters were estimated using the option “LIKELIHOOD LAPLACE METHOD=conditional” in the NONMEM (Nonlinear Mixed Effects Modeling) software (version VII; GloboMax, Hanover, MD, USA). The inter-individual random variability of Ce50and λ was modeled using a log-normal model. For each analysis, NONMEM computes the minimum value of the objective function, a statistic that is proportional to negative twice the log likelihood of the data. To determine the relevant covariates in the final model, a forward inclusion and backward elimination approach was used in consecutive NONMEM runs. A covariate was considered significant when its inclusion lowered the minimum value of the objective function by at least 3.85 points. The difference in the minimum value of the objective function between two nested models was approximately χ2-distributed and could therefore be used for significance tests (P<0.05, with one degree of freedom).
Results
Ninety-four patients met the selection criteria. Fifty-five patients underwent eye surgery and 39 patients underwent ENT surgery. The duration of surgery and anesthesia were 66.9±53.0 and 97.5±54.0 min. The BIS values at baseline and LOC were 92.8±4.9 and 67.0±15.1. At LOC, the effect-site concentrations (Ces) of propofol and remifentanil were 4.4±1.1 μg/mL and 2.0±0.3 ng/mL, respectively. At the end of surgery, the BIS value, the Ces of propofol and remifentanil were 43.8±10.6, 3.2±1.0 μg/mL and 2.3±0.4 ng/mL, respectively. At ROC, the BIS value, the Ces of propofol and remifentanil were 75.7±6.0, 1.1±0.3 μg/mL and 0.8±1.0 ng/mL, respectively. Table 1 shows the data and correlation coefficients between the propofol Ce at ROC and the analyzed variables. The propofol Ce at LOC had a tendency to be positively correlated with the propofol Ce at ROC, but this correlation was not statistically significant (P=0.08). With the exception of age, no other clinical variable had a significant correlation with propofol Ce at ROC (Table 1). Age was significantly correlated with the propofol Ce at ROC, with a negative slope (P<0.01, Figure 1).
Because age was the only factor that was found to be correlated with propofol Ce at ROC, we included this as a covariate in Ce50 and λ. This pharmacodynamic modeling including age significantly improved the performance of the basic model based on the likelihood ratio test, with a decrease the minimum value of the objective function (P<0.01). Table 2 lists the model parameter estimates for the final selected model. The relationship between the probability of ROC and propofol Ce is shown in Figure 2. The effect of age on the probability of ROC as evaluated by computed estimation is presented in Figure 3. The values of age used for the predictions correspond to the 25-, 50-, and 75-year-old patients as distributed within the studied population. The Ce50in 25-, 50-, and 75-year-old patients was predicted to be 1.38, 1.06, and 0.74 μg/mL, respectively. The λ in 25-, 50-, and 75-year-old patients was predicted to be 12.23, 8.70, and 5.18, respectively.
Discussion
In this study, we searched for clinical factors influencing ROC during emergence from propofol-remifentanil anesthesia and found that age was strongly correlated with ROC. In addition, upon pharmacodynamic modeling, age proved to be a significant covariate of Ce50 and λ in the dynamic relationship between propofol Ce and ROC. This study is the first clinical investigation in which pharmacodynamic modeling of ROC has been carried out by incorporating covariates of ROC. It would be clinically advantageous if the individual propofol Ce for ROC could be predicted and applied rather than simply targeting a population-based average concentration. A nonlinear dynamic model was chosen to describe the relationship between propofol Ce and ROC, as quantal response data exhibit a sigmoid relationship. A sigmoidal Emax model using the Hill equation provided a better model than a linear regression since this combination can estimate not only the Ce50 value but the shape or, alternatively, the scale of the concentration-effect relationship (λ)10. Moreover, the Ce50values derived from a sigmoidal Emax model are not affected by extreme values to the same extent as in a linear regression model3.
In the present study, inter-individual variability in propofol Ce at ROC could be explained by incorporating age as a covariate. Although the patients anthropometric factors except age had little influence on ROC, other potential covariates such as genetics or environmental factors might also play an important role in determining individual ROC and hence contribute to the variability of inter-individual data sets11. The Schnider pharmacokinetic model was developed based on data from Caucasians, so it may be necessary to examine whether the administration of propofol using a TCI technique based on the Schnider model will provide the same estimated concentration and result in the same dynamic end points in Korean patients.
According to our prediction of the probability of ROC, the propofol Ce50 for a 25-year-old patient is around twice that for a 75-year-old patient. Younger patients may recover consciousness after receiving higher propofol concentrations than could be administered to elderly patients. The Ce5 value, which indicates a 95% probability that a 25-year-old patient does not recover consciousness, is around 1.8 μg/mL based on our concentration-response curve. To prevent accidental awareness in young patients with propofol-remifentanil anesthesia, levels at least above this Ce should be maintained during surgery. The value of λ, representing the steepness of the dose-response curve, was greater in younger patients than in older patients. This finding suggests that younger patients may recover more abruptly than older patients, which means that young patients may be easily arousable, able to be extubated, and oriented. However, this may lead to the possibility of trauma as a result of sudden movement, and more attention should be paid to patients safety. The reverse situation could also occur. Elderly patients may experience long and more difficult recovery times. Close monitoring is necessary for elderly patients to prevent re-sedation or respiratory depression due to residual sedative effects during post-anesthetic care after initial ROC.
In older patients, a smaller propofol Ce is required at ROC for both pharmacokinetic and pharmacodynamic reasons. We used the Schnider propofol pharmacokinetic model5, 6, which takes age into consideration, and hence the pharmacokinetic inter-patient variability caused by age would be excluded. In addition, the Schnider model, although still not perfect, has fewer limitations than the other pharmacokinetic models for propofol and therefore has the potential for being the recommended model of choice to be used for TCI12. The significant correlation between propofol Ce at ROC and age suggests that age has a considerable influence on the patient's sensitivity to propofol from a pharmacodynamic point of view.
When the effect of remifentanil Ce on ROC was analyzed, we did not find a significant correlation, which is consistent with previous reports13, 14. The Ce of remifentanil (0.7±0.8 ng/mL) at ROC was probably too low to affect ROC. However, when predicting the propofol Ce for ROC, it should be kept in mind that the Ce values of propofol might be different if another sedative, such as a benzodiazepine or a large dose of remifentanil, is also used. The type of surgery may also influence the propofol Ce at ROC. The Ce of propofol for ROC may be slightly increased in the presence of severe pain caused by major surgeries, eg, thoracic or abdominal surgery, compared to minor surgeries like those in our study15. The Ce of propofol at ROC was not correlated with the duration of propofol infusion or the mean dose of propofol during surgery, which is consistent with a previous study by Kazama et al16. These clinical contexts (duration or dose) would influence the time taken to reach an individual's propofol Ce for ROC. Current TCI devices display the time required for a calculated Ce to decline to a predetermined value of propofol Ce if the infusion is to be stopped. This allows anesthesiologists to predict the time to ROC, provided that the individual Ce at ROC is known17.
Although not statistically significant (P=0.08), there was a tendency for the Ce of propofol for LOC to positively correlate with the propofol Ce at ROC, which suggests that patients requiring a higher propofol Ce at LOC tend to recover consciousness at a higher propofol Ce as well. We also found that the mean propofol Ce for LOC was higher than that reported in other studies (4.4±1.1 μg/mL vs 1.25–2.35 μg/mL)6, 18. One possible explanation for the higher Ce observed in our study is the use of a different pharmacokinetic model. The Schnider model predicts much faster effect-site equilibration with the blood than the Marsh model, as the equilibration constant (Keo) is larger in the Schnider model than in the Marsh model (0.459 min−1 vs 0.26 min−1). The predicted Ce in the Schnider model will be higher than that in the Marsh model during the induction period19.
We note that our study has some limitations. We collected the data of dissipating propofol concentrations after stopping infusion, which could lead to a high performance error of TCI-based predictions of propofol Ce rather than stable propofol Ce. To eliminate the confounding effects of pharmacokinetic and pharmacodynamic variability in the response of patients to a certain stimulus, constant Ce values and blood to effect-site equilibration are required16. However, our study design is more applicable to daily clinical practice during emergence from propofol-remifentanil anesthesia.
We conclude that age significantly affects the pharmacodynamic relationship between propofol Ce and ROC. The propofol Ce for ROC can be predicted for individual patients of different ages, and patients can be expected to require shorter recovery times and awaken quickly with early titration of propofol upon surgery completion.
Author contribution
Dong-woo HAN and Bon-nyeo KOO designed research; Young-ran KANG and Jae-hoon LEE performed research; Dong-woo HAN, Jeong-rim LEE, Gyu-jeong NOH, and Jaehoon LEE analyzed data; Dong-woo HAN wrote the paper.
References
Larsen B, Seitz A, Larsen R . Recovery of cognitive function after remifentanil–propofol anesthesia: a comparison with desflurane and sevoflurane anesthesia. Anesth Analg 2000; 90: 168–74.
Nunes CS, Ferreira DA, Antunes L, Amorim P . Clinical variables related to propofol effect-site concentrations at recovery of consciousness after neurosurgical procedures. J Neurosurg Anesthesiol 2005; 17: 110–4.
Wessén A, Persson PM, Nilsson A, Hartvig P . Concentration-effect relationships of propofol after total intravenous anesthesia. Anesth Analg 1993; 77: 1000–7.
Chortkoff BS, Eger EI 2nd, Crankshaw DP, Gonsowski CT, Dutton RC, Ionescu P . Concentrations of desflurane and propofol that suppress response to command in humans. Anesth Analg 1995; 81: 737–43.
Schnider TW, Minto CF, Gambus PL, Andresen C, Goodale DB, Shafer SL, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology 1998; 88: 1170–82.
Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, et al. The influence of age on propofol pharmacodynamics. Anesthesiology 1999; 90: 1502–16.
Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology 1997; 86: 10–23.
Minto CF, Schnider TW, Shafer SL . Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology 1997; 86: 24–33.
Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, et al. Validity and reliability of the Observer's Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol 1990; 10: 244–51.
Lu W, Ramsay JG, Bailey JM . Reliability of pharmacodynamic analysis by logistic regression: mixed-effects modeling. Anesthesiology 2003; 99: 1255–62.
Dahaba AA, Zhong T, Lu HS, Bornemann H, Liebmann M, Wilfinger G, et al. Geographic differences in the target-controlled infusion estimated concentration of propofol: bispectral index response curves. Can J Anaesth 2011; 58: 364–70.
Masui K, Upton RN, Doufas AG, Coetzee JF, Kazama T, Mortier EP, et al. The performance of compartmental and physiologically based recirculatory pharmacokinetic models for propofol: a comparison using bolus, continuous, and target-controlled infusion data. Anesth Analg 2010; 111: 368–79.
Nunes CS, Ferreira DA, Antunes L, Lobo F, Santos IA, Amorim P . Individual effect-site concentrations of propofol at return of consciousness are related to the concentrations at loss of consciousness and age in neurosurgical patients. J Clin Anesth 2009; 21: 3–8.
Nho JS, Lee SY, Kang JM, Kim MC, Choi YK, Shin OY, et al. Effects of maintaining a remifentanil infusion on the recovery profiles during emergence from anaesthesia and tracheal extubation. Br J Anaesth 2009; 103: 817–21.
Iwakiri H, Nagata O, Matsukawa T, Ozaki M, Sessler DI . Effect-site concentration of propofol for recovery of consciousness is virtually independent of fentanyl effect-site concentration. Anesth Analg 2003; 96: 1651–5.
Kazama T, Ikeda K, Morita K, Sanjo Y . Awakening propofol concentration with and without blood-effect site equilibration after short-term and long-term administration of propofol and fentanyl anesthesia. Anesthesiology 1998; 88: 928–34.
McCormack J, Mehta D, Peiris K, Dumont G, Fung P, Lim J, et al. The effect of a target controlled infusion of propofol on predictability of recovery from anesthesia in children. Paediatr Anaesth 2010; 20: 56–62.
Iwakiri H, Nishihara N, Nagata O, Matsukawa T, Ozaki M, Sessler DI . Individual effect-site concentrations of propofol are similar at loss of consciousness and at awakening. Anesth Analg 2005; 100: 107–10.
Barakat AR, Sutcliffe N, Schwab M . Effect site concentration during propofol TCI sedation: a comparison of sedation score with two pharmacokinetic models. Anaesthesia 2007; 62: 661–6.
Acknowledgements
This work was supported in part by the Yonsei University Research Fund of 2009.
The authors thank Dr Go Un ROH MD (Department of Anesthesiology and Pain Medicine and Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea) for her assistance with analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koo, Bn., Lee, Jr., Noh, Gj. et al. A pharmacodynamic analysis of factors affecting recovery from anesthesia with propofol-remifentanil target controlled infusion. Acta Pharmacol Sin 33, 1080–1084 (2012). https://doi.org/10.1038/aps.2012.85
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.85
Keywords
This article is cited by
-
Predicting the optimal concentration of remifentanil for skull pin fixation with hemodynamic and analgesia nociception index monitoring
Scientific Reports (2024)
-
Monitoring of anesthetic depth and EEG band power using phase lag entropy during propofol anesthesia
BMC Anesthesiology (2020)
-
Propofol target-controlled infusion modeling in rabbits: Pharmacokinetic and pharmacodynamic analysis
Journal of Huazhong University of Science and Technology [Medical Sciences] (2016)