Abstract
Aim:
To evaluate the effects of tanshinone IIA (Tan IIA), a lipophilic diterpene from the Chinese herb Salvia miltiorrhiza, on lipopolysaccharide (LPS)-induced disseminated intravascular coagulation (DIC) in rabbits.
Methods:
LPS-induced DIC model was made in adult male New Zealand rabbits by continuous intravenous infusion of LPS (0.5 mg/kg) via marginal ear vein for 6 h. The animals were simultaneously administered with Tan IIA (1, 3 and 10 mg/kg) or heparin (500 000 IU/kg) through continuous infusion via the contralateral marginal ear vein for 6 h. Before and 2 and 6 h after the start of LPS infusion, blood samples were taken for biochemical analyses.
Results:
Continuous infusion of LPS into the rabbits gradually impaired the hemostatic parameters, damaged renal and liver functions, increased the plasma TNF-α level, and led to a high mortality rate (80%). Treatment of the rabbits with Tan IIA dose-dependently attenuated the increase in activated partial thromboplastin time (APTT), prothrombin time (PT) and fibrin-fibrinogen degradation products (FDP); ameliorated the decrease in plasma levels of fibrinogen and platelets; and reversed the decline in activity of protein C and antithrombin III. Meanwhile, the treatment significantly suppressed the increase in the plasma levels of aminotransferase, creatinine and TNF-α, and led to much lower mortality (46.7% and 26.7% for the medium- and high-dose groups). Treatment of the rabbits with the high dose of heparin also effectively improved the hemostatic parameters, ameliorated liver and renal injuries, and reduced the plasma level of TNF-α, and significantly reduced the mortality (33.3%).
Conclusion:
Tan IIA exerts a protective effect against DIC in rabbits.
Similar content being viewed by others
Introduction
Disseminated intravascular coagulation (DIC) is an acquired syndrome characterized by the activation of intravascular coagulation and subsequent intravascular fibrin formation. It occurs secondary to an underlying disorder such as cancer, trauma, or infection. DIC frequently results in organ failure because numerous microthrombi form in the organ, creating a disturbance in the microcirculation1,2. This process is a serious health hazard and is a cause for the poor prognosis in cases of DIC. The basic pathological mechanism of DIC includes the spread of microvascular thromboses and the excessive release of pro-inflammatory cytokines such as tumor necrosis factor alpha (TNF-α)3. Current clinical trials aim at an interruption of the “latent coagulation” in DIC by administering coagulation inhibitors such as heparin, which depend on activating the antithrombin (AT) in plasma; however, in DIC, AT is also consumed, so the anticoagulant effect of heparin could be limited4.
Chinese herbs have been widely used to treat inflammatory and thrombotic diseases throughout history. The dried root, or rhizome, of Salvia miltiorrhiza is officially listed in the Chinese Pharmacopoeia (Pharmacopoeia Commission of the People's Republic of China, 2000) for the treatment of inflammation and cardiovascular diseases, including thrombolytic diseases5,6. Tanshinone IIA (Tan IIA) is a lipophilic diterpene compound found as a marker component in Salvia miltiorrhiza. Previous pharmacological studies indicated that Tan IIA could inhibit platelet aggregation7, suppress LPS-induced TNF-α release8, and inhibit thrombus formation9. Furthermore, our previous study also found that an injection of a compound Salvia miltiorrhiza injection could have a protective effect on LPS-induced DIC in rabbits10. These research advances suggested that Tan IIA may be an attractive agent for the treatment of DIC.
Although many of the properties of Tan IIA are known, there are few studies investigating its effects on DIC. In this study, we found that Tan IIA protected against LPS-induced DIC through its anticoagulation activity and its inhibition of TNF-α.
Materials and methods
Reagents
Sodium tanshinone IIA sulfonate (Tan IIA, C19H17NaO6S, purity 99.0%) was purchased from Topharman Shanghai Co Ltd (Shanghai, China). The solution of Tan IIA was freshly prepared before use. Lipopolysaccharide (LPS) and heparin were purchased from Sigma (St Louis, USA). A TNF-α ELISA kit was purchased from RapidBio Lab (Calabasas, USA). The reagent packs for the activity assays of antithrombin III (ATIII) and protein C were obtained from Sun Biotechnology Company (Shanghai, China). All other reagents were of analytical grade and obtained from commercial sources.
Animals
Adult male New Zealand white rabbits (weighing 2–3 kg, Grade II) were supplied by the Experimental Animal Center of Zhongshan Medical College, Sun Yat-sen University, China.
Experimental models and drug treatments
All animal experiments were conducted in accordance with the National Research Council Guide for the Care and Use of Laboratory Animals and were approved by the Sun Yat-sen University Animal Care and Use Committee (Guangzhou, China).
Animals were anesthetized by an intramuscular injection of 30 mg/kg of ketamine hydrochloride, followed by intramuscular supplements of 10 mg/kg of ketamine hydrochloride given 2 h, 4 h, and 6 h after the start of the ketamine infusion. DIC experimental models were performed according to the previous report11 and were induced by infusing an LPS solution (0.5 mg/kg of LPS into 60 mL of saline) at a rate of 10 mL/h through the marginal ear vein of the rabbits over a period of 6 h. The LPS control group was infused with 60 mL of saline solution. Treatments were started through the contralateral marginal ear vein simultaneously with the LPS infusion.
Twelve different treatment groups were established, 6 containing 10 animals each (for the measurement of biochemical indexes and TNF-α) and 6 containing 15 animals each (for the measurement of survival rate). Within each set of 6, treatment groups were given either 1, 3, or 10 mg/kg of Tan IIA (low-, medium-, or high-dose, respectively) in 60 mL of saline solution over a period of 6 h (a solution infusion rate of 10 mL/h). The heparin control group was infused with 500 000 IU/kg of heparin in 60 mL of saline solution over a period of 6 h. The additional rabbits, which were given neither LPS nor Tan IIA, were infused with 60 mL of saline solution (10 mL/h) through both marginal ear veins.
Biochemical analyses
Blood samples of 1 mL were taken immediately before LPS infusion and at 2 h and 6 h after the start of the infusion. The activities of ATIII and protein C were measured according to the reagent pack instructions based on chromogenic substrates. An automatic analyzer (Sysmex SE-9500, Sysmex CA 1500, Japan) was used to determine the activated partial thromboplastin time (APTT) and, prothrombin time (PT), as well as the plasma levels of platelets, fibrinogen and fibrin-fibrinogen degradation products (FDP). A 7170A automatic analyzer (HITACHI, Japan) was used to detect the plasma levels of alanine aminotransferase (ALT, the marker of liver injury) and creatinine (Cr, the marker of renal injury).
Measurement of TNF-α concentration
One milliliter of each rabbit's plasma was collected in a tube and stored at -20 °C until assayed. The concentrations of TNF-α in the animal plasma samples were determined using an ELISA kit.
Measurement of survival rate
After the experiment, animals were allowed to recover from anesthesia with access to food and water ad libitum. The 24-h survival rate in the different groups was recorded.
Data analyses
Differences between group data were evaluated for significance using either a non-parametric test (the Kruskal-Wallis H test) or two-way repeated measures. The repeated measures analysis of variance was used for the multivariate analyses. All experiments were repeated at least three times, and the data were presented as the mean±SD unless otherwise noted. Data of the activities of ATIII and protein C and the concentration of ALT and Cr at 2 h and 6 h were converted to percentages, with a value of 100% assumed for basal data. Survival curves of LPS-induced DIC were analyzed by the Kaplan-Meyer log-rank test. Differences with P values of less than 0.05 were considered to be statistically significant.
Results
Protective effects of Tan IIA on LPS-induced DIC
We investigated the protective effects of Tan IIA on LPS-induced DIC using a rabbit model, a clinically relevant animal model for human DIC12. Twenty percent (3/15) of the rabbits infused with LPS survived 24 h following the start of the experiment. Tan IIA treatment was started simultaneously with LPS induction of DIC. Our results showed that the Tan IIA treatment significantly increased the survival rate (P<0.05, compared with the LPS control group, Figure 1). Eight of fifteen rabbits (53.3%) survived in the medium-dose of Tan IIA-treated group, and eleven of fifteen rabbits (73.3%) survived in the high-dose Tan IIA-treated group. Heparin, the agent clinically used in DIC therapy, increased the survival rate from 20% to 66.7%. All of the animals in the sham group without LPS survived (data not shown).
Effects of Tan IIA on biochemical and pathological damages in LPS-induced DIC
To further elucidate the outcome of Tan IIA on DIC induced by LPS, we systematically investigated the biochemical and pathological effects using a rabbit model. Table 1 summarizes the plasma APTT, PT, platelet counts, fibrinogen levels, and FDP levels as well as the activities of protein C and ATIII for all the groups — normal rabbits, LPS-induced DIC rabbits, Tan IIA-treated rabbits and heparin-treated rabbits. The values of APTT, PT, and FDP for the LPS-induced DIC rabbits were all significantly higher than those for the normal rabbits (P<0.05, Table 1); however, the values of both fibrinogen and platelet counts and the activities of protein C and ATIII were significantly lower than those for the normal rabbits (P<0.05, Table 1). The infusions of both Tan IIA and heparin significantly attenuated the increased APTT, PT, and levels of FDP as well as the decreased levels of fibrinogen and platelets; treatment also improved the decreased activities of protein C and ATIII (P<0.05, compared with the LPS control group, Table 1). Furthermore, the infusion of heparin significantly moderated the increased APTT and PT at 6 h along with the decreased platelet counts at 2 h and 6 h when compared with the low-dose Tan IIA-treated group (P<0.05, Table 1).
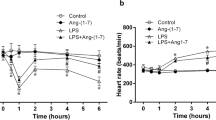
Effects of Tan IIA on liver and renal injury in LPS-induced DIC
We investigated the effects of Tan IIA on liver and renal injuries in LPS-induced DIC rabbits. The plasma levels of ALT, an indicator of liver injury, were increased by LPS infusion. However, the levels of ALT were significantly lower in Tan IIA- and heparin-treated rabbits (P<0.05, compared with the LPS control group, Figure 2). A similar finding was observed in the plasma levels of Cr, which is an indicator of renal injury. An increase in Cr levels was observed in the LPS group, which was significantly suppressed by both Tan IIA and heparin (P<0.05, compared with the LPS control group, Figure 3). Furthermore, the infusion of heparin significantly suppressed the increased plasma levels of ALT and Cr at 6 h compared with the low-dose Tan IIA-treated group (P<0.05, Figure 2, 3).
Effect of Tan IIA 1, 3, and 10 mg/kg on the plasma levels of ALT in LPS-induced DIC rabbits. Blood samples were taken immediately before LPS infusion and 2 h, 6 h after the start of the infusion. An automatic analyzer detected the plasma levels of ALT. Results of ALT at 2 h and 6 h were converted to percentages assuming a value of 100% for basal data. Values are expressed as the mean±SD percent of the initial value before LPS infusion. bP<0.05 vs the LPS control group; n=10.
Effect of Tan IIA 1, 3, and 10 mg/kg on the plasma levels of Cr in LPS-induced DIC rabbits. Blood samples were taken immediately before LPS infusion and 2 h, 6 h after the start of the infusion. An automatic analyzer detected the plasma levels of Cr. Results of Cr at 2 h and 6 h were converted to percentages assuming a value of 100% for basal data. Values are expressed as the mean±SD. percent of the initial value before LPS infusion. bP<0.05 vs DIC group. n=10.
Effect of Tan IIA on TNF-α in vivo
TNF-α is an important inflammatory marker and generally increases significantly during the early period of DIC. Therefore, we tested whether Tan IIA had any effect on the plasma levels of TNF-α. Rabbits were injected with 0.5 mg/kg of LPS, and the levels of TNF-α were dramatically increased at 1, 4, 8, and 12 h (P<0.05, compared with normal rabbits, Figure 4). However, the infusions of 1, 3, and 10 mg/kg of Tan IIA significantly reduced the increased plasma levels of TNF-α at each of those time points (P<0.05, compared with normal rabbits, Figure 4). An infusion of 500 000 IU/kg of heparin also significantly reduced the increased plasma levels of TNF-α at 1, 4, 8, and 12 h (P<0.05, compared with the LPS control group; P<0.05, compared with the low-dose Tan IIA-treated group, Figure 4).
Discussion
LPS, a constituent of the outer membrane of gram-negative bacteria, is a major pathogenic factor contributing to the initiation of life-threatening DIC, which occurs often in intensive care unit patients. Induction of DIC leads to the generation of pro-inflammatory cytokines by monocytes and endothelial cells, which in turn activate coagulation and fibrinolytic pathways13. In this study, an infusion of LPS resulted in the typical changes of DIC: a significant increase in APTT, PT, FDP levels, and TNF-α levels; a severe decrease in the activities of ATIII and protein C; a decrease in the levels of fibrinogen and platelets; and a high mortality rate, which was consistent with our previous results10.
In this study, we reported that Tan IIA had a significant protective effect against the lethal effects of LPS-induced DIC in rabbits. Using this rabbit model of DIC, we found that all 3 doses of Tan IIA administered could not only improve the biochemical signs of DIC but could also ameliorate organ injury and decrease the mortality of LPS-treated animals (P<0.05). This dramatic benefit was further verified by a significant reduction in the levels of TNF-α observed in Tan IIA-treated rabbits.
The hallmark of the coagulation disorder in DIC is the imbalance between intravascular fibrin formation and its removal. The serious reduction in anticoagulant capacity and the inhibition of fibrinolysis result in a massive activation of coagulation, finally leading to overwhelming fibrin formation and the consumption of clotting factors and inhibitors. Abundant intravascular fibrin formation leads to microvascular thrombosis, which contributes to the development of multiple organ failure14.
To investigate whether the coagulation process was altered in Tan IIA-treated animals, we first measured the APTT and PT to evaluate the intrinsic and extrinsic pathways of coagulation, respectively. It was observed that the infusion of Tan IIA induced a decrease in PT and APTT when compared to the LPS control group. Platelet aggregation is one of the important triggers of blood coagulation in the pathologic thrombosis associated with DIC15. DIC produces massive thrombin, stimulates platelet aggregation and triggers the blood coagulation cascades. Those cascades result in a lowering of the blood's platelet counts and its fibrinogen level, enhancing the FDP concentration and prolonging both PT and APTT. The procoagulant environment predisposes the animals to develop excessive microthrombi and increases the consumption of platelets and fibrinogen. Thus, we also measured platelet counts, fibrinogen concentrations, and FDP, which were the useful parameters in diagnosing DIC. It was observed that an infusion of Tan IIA could improve all of these parameters when compared with the LPS control group. In our previous study, we found that an injection of a compound from Salvia miltiorrhiza could have a protective effect on LPS-induced DIC in rabbits. These current results suggested that the increase in the activation times of the extrinsic and intrinsic coagulation pathways was related to a delay in the coagulation process, which in turn was due to a slowing of fibrin clot formation and an inhibition of platelet aggregation (as shown by the improvement in platelet numbers).
The initial decrease in protein C and/or ATIII levels may have particular prognostic significance for the clinical management of DIC, which has an almost absolute lethality16,17. In this study, the improvements in protein C and ATIII activity by the infusion of Tan IIA were remarkable among the observed coagulation-related parameters. The chief cause of protein C and ATIII deficiency in LPS-induced DIC is not a decrease in production but an increase in consumption due to the enhanced generation of thrombin. The antithrombotic and/or anticoagulant effect of Tan IIA would reduce the consumption of coagulation factors during the development of DIC. Lastly, we also observed that Tan IIA significantly attenuated both the increased APTT and PT and the decreased plasma levels of platelets and fibrinogen as well as treatment with heparin.
Abundant evidence has shown that inflammation and thrombosis are closely related during DIC. Severe inflammation can both induce coagulation and lead to disturbances of coagulation. Severe coagulation dysfunction can promote further inflammation, causing increased morbidity and mortality18,19. Among proinflammatory cytokines, TNF-α is the trigger of an inflammatory cascade and is thus crucial in local and distant organ injury; its levels also correlate well with the severity of DIC20,21. In the present study, Tan IIA reduced the TNF-α levels in LPS-induced DIC rabbits. These results could suggest one of the main mechanisms of action of Tan IIA against DIC.
As the onset of multiorgan dysfunction syndrome has been shown to forecast mortality in patients with DIC, the protection of organs, particularly the liver and kidney, is important in DIC treatment22. In the present study, we demonstrated that Tan IIA had a protective effect on LPS-induced DIC in rabbits by ameliorating organ dysfunction. Two possible mechanisms are implicated in these favorable results. First, the effect of Tan IIA on biochemical plasma levels may be a consequence of its effect of improving blood flow to organs; we observed that plasma levels of ALT and Cr, which were increased by LPS infusion, were significantly decreased in Tan IIA-treated animals. Second, Tan IIA has been shown to have an anti-inflammatory result through its proteolytic effect on TNF-α, which is the critical mediator of LPS-induced organ failure. Taken together, these two actions of Tan IIA have a favorable therapeutic effect on LPS-induced DIC rabbits.
We also analyzed the effects of heparin on LPS-induced DIC in rabbits. The traditional anticoagulant heparin, especially at high therapeutic dosages, is effective in interrupting intravascular clotting in cases of acute DIC, which confirms the results of clinical studies in humans as well as experimental studies on rats and rabbits23,24. In the present study, a high dose of heparin (500 000 IU/kg) was used for modulation of the DIC process and aided in prevention as well as treatment. When rabbits were treated with heparin alone, hemostatic parameters were improved, liver and renal injuries were ameliorated, mortality was significantly reduced, and the concentration of TNF-α was reduced.
In conclusion, Tan IIA may have protective effects on DIC by reducing coagulation, aiding the breakdown of TNF-α, and ameliorating organ dysfunction. Our study indicated that Tan IIA could be a good candidate for the development of new agents to fight against DIC. However, we emphasize that the true utility of Tan IIA in combating DIC will require further direct testing through clinical trials.
Abbreviations
APTT, activated partial thromboplastin time; PT, prothrombin time; Tan IIA, sodium tanshinone IIA; LPS, lipopolysaccharide; FDP, fibrin-fibrinogen degradation products; ALT, alanine aminotransferase; Cr, creatinine; TNF-α, tumor necrosis factor alpha.
Author contribution
Liang-cai WU designed the study; Hao SUN performed the research; Xi LIN contributed new analytical tools and reagents; Liang-cai WU and Xi LIN analyzed the data and wrote the paper.
References
Markwardt F, Nowak G, Meerbach W, Rudiger KD . Studies in experimental animals on disseminated intravascular coagulation (DIC). Thromb Diath Haemorrh 1975; 34: 513–21.
Wilde JT, Roberts KM, Greaves M, Preston FE . Association between necropsy evidence of disseminated intravascular coagulation and coagulation variables before death in patients in intensive care units. J Clin Pathol 1988; 41: 138–42.
Levi M, ten Cate H . Disseminated intravascular coagulation. N Engl J Med 1999; 341: 586–92.
Klein HG, Bell WR . Disseminated intravascular coagulation during heparin therapy. Ann Intern Med 1974; 80: 477–81.
Lei XL, Chiou GC . Studies on cardiovascular actions of Salvia miltiorrhiza. Am J Chin Med 1986; 14: 26–32.
Wang N, Luo HW, Niwa M, Ji J . A new platelet aggregation inhibitor from Salvia miltiorrhiza. Planta Med 1989; 55: 390–1.
Liu JQ, Lee TF, Miedzyblocki M, Chan GC, Bigam DL, Cheung PY . Effects of tanshinone IIA, a major component of Salvia miltiorrhiza, on platelet aggregation in healthy newborn piglets. J Ethnopharmacol 2011; 137: 44–9.
Wan JM, Sit WH, Lee CL, Fu KH, Chan DK . Protection of lethal toxicity of endotoxin by Salvia miltiorrhiza BUNGE is via reduction in tumor necrosis factor alpha release and liver injury. Int Immunopharmacol 2006; 6: 750–8.
Ji HS, Yu F, Yang J . Comparative research on pharmacodynamics of Danshen co-microemulsion on hemorheology in rats with hyperlipidemia. Zhong Yao Cai 2008; 31: 566–9.
Lin X, Qi JZ, Qiu PX, Chen JS . Effect of compound Salvia miltiorrhiza injection on LPS-induced disseminated intravascular coagulation in rabbits. Chin J Pathophysiol 2011; 27: 464–8.
Lin X, Liang XX, Chen JS, Chen Q, Qiu PX, Yan GM . The effect of fibrinolytic enzyme FIIa from Agkistrodon acutus venom ondisse minated intravascular coagulation in rabbits. Transl Res 2007; 150: 295–302.
Levi M, ten Cate H, van der Poll T, van Deventer SJ . Pathogenesis of disseminated intravascular coagulation in sepsis. JAMA 1993; 270: 975–9.
Warr TA, Rao LV, Rapaport SI . Disseminated intravascular coagulation in rabbits induced by administration of endotoxin or tissue factor: effect of anti-tissue factor antibodies and measurement of plasma extrinsic pathway inhibitor activity. Blood 1990; 75: 1481–9.
Zeerleder S, Hack CE, Wuillemin WA . Disseminated intravascular coagulation in sepsis. Chest 2005; 128: 2864–75.
Hathcock JJ . Flow effects on coagulation and thrombosis. Arterioscler Thromb Vasc Biol 2006; 26: 1729–37.
Sakata Y . Treatment of DIC associated with myelogenous leukemia. Nihon Rinsho 2009; 67: 1978–83.
Oh D, Jang MJ, Lee SJ, Chong SY, Kang MS, Wada H . Evaluation of modified non-overt DIC criteria on the prediction of poor outcome in patients with sepsis. Thromb Res 2010; 126: 18–23.
Taveira da Silva AM, Kaulbach HC, Chuidian FS, Lambert DR, Suffredini AF, Danner RL . Brief report: shock and multiple-organ dysfunction after self-administration of Salmonella endotoxin. N Engl J Med 1993; 328: 1457–60.
Fong Y, Tracey KJ, Moldawer LL, Hesse DG, Manogue KB, Kenney JS, et al. Antibodies to cachectin/tumor necrosis factor reduce interleukin 1 beta and interleukin 6 appearance during lethal bacteremia. J Exp Med 1989; 170: 1627.
Schabbauer G, Tencati M, Pedersen B, Pawlinski R, Mackman N . PI3K-Akt pathway suppresses coagulation and inflammation in endotoxemic mice. Arterioscler Thromb Vasc Biol 2004; 24: 1963–9.
Cataldegirmen G, Zeng S, Feirt N, Lppagunta N, Dun H, Qu W, et al. RAGE limits regeneration after massive liver injury by coordinated suppression of TNF-α and NF-κB. J Exp Med 2005; 201: 473–84.
Levi M . Disseminated intravascular coagulation: what's new? Crit Care Clin 2005; 21: 449–67.
Fujishima Y, Yokota K, Sukamoto T . The effect of danaparoid sodium (danaparoid) on endotoxin-induced experimental disseminated intravascular coagulation (DIC) in rats. Thromb Res 1998; 91: 221–7.
Hamano S, Kinukawa M, Komatsu H, Miyata H, Sakuragawa N . Effects of low molecular weight heparin (FR-860) on the experimental disseminated intravascular coagulation models. Nihon Yakurigaku Zasshi 1991; 98: 53–62.
Acknowledgements
This project was supported by the National Natural Science Foundation of China (No 81000209), the Key Project of the Chinese Ministry of Education (No 210255), and the Fundamental Research Funds for the Central Universities (No 21609304). The authors declare that they have no competing financial interest in Tan IIA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, Lc., Lin, X. & Sun, H. Tanshinone IIA protects rabbits against LPS-induced disseminated intravascular coagulation (DIC). Acta Pharmacol Sin 33, 1254–1259 (2012). https://doi.org/10.1038/aps.2012.84
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.84
Keywords
This article is cited by
-
Efficacy of Sodium Tanshinone IIA Sulfonate in Patients with Non-ST Elevation Acute Coronary Syndrome Undergoing Percutaneous Coronary Intervention: Results from a Multicentre, Controlled, Randomized Trial
Cardiovascular Drugs and Therapy (2021)
-
Quinone diterpenes from Salvia species: chemistry, botany, and biological activity
Phytochemistry Reviews (2019)
-
Tanshinone-1 induces tumor cell killing, enhanced by inhibition of secondary activation of signaling networks
Cell Death & Disease (2013)