Abstract
Aim:
To investigate the protective effects of simvastatin (Sim) combined with nifedipine (Nif) on endothelial cells and elucidate the action mechanism.
Methods:
Human umbilical vein endothelial cells (HUVEC) were used. mRNA and protein levels were measured by using reverse-transcription polymerase chain reaction (RT-PCR) and Western blotting, respectively. Intracellular calcium and reactive oxygen species (ROS) were detected using confocal microscopy. The Griess assay was used to evaluate nitric oxide (NO) release.
Results:
Treatment of HUVEC with H2O2 100 μmol/L for 30 min inhibited the mRNA and protein expression of endothelial nitric oxide synthase (eNOS). With increased concentrations of Nif, eNOS mRNA and protein levels increased (P<0.05). Combined treatment with Sim 1.0 μmol/L and Nif 1.0 μmol/L significantly increased the mRNA and protein expression of eNOS and NO release compared with Sim or Nif alone (P<0.05). The combination significantly lowered the intracellular ROS level (P<0.05), which was correlated with the increase in eNOS and NO, but there was no visible change in intracellular calcium (P>0.05). Compared with individual drug treatment, Akt phosphorylation and the ratio of p-eNOS/eNOS were up-regulated in the combination group, and this effect was inhibited by the phosphatidylinositol 3-kinase (PI3K) inhibitors wortmannin and LY294002.
Conclusion:
The Sim-Nif combination effectively protects HUVEC against H2O2 injury by inhibiting intracellular ROS generation, increasing the ratio of p-eNOS/eNOS and up-regulating Akt phosphorylation.
Similar content being viewed by others
Introduction
Hypertension and arteriosclerosis are common maladies among aged people in China and remain the most important risk factors for cardiovascular disease. Aging hypertensive patients often co-present with arteriosclerosis1. Functional impairment of vascular endothelial cells is involved in the formation of hypertension and arteriosclerosis2. Therefore, maintenance of vascular endothelial function is important to prevent hypertension and arteriosclerosis3, 4.
Endothelial nitric oxide synthase (eNOS) and the nitric oxide (NO) excreted by eNOS are important regulatory factors of endothelial cells because they protect against the development of hypertension and arteriosclerosis by expanding the blood vessels, inhibiting platelet coagulation and preventing conglutination between blood cells and between blood cells and endothelial cells5, 6. A variety of anti-hypertension drugs have also shown anti-arteriosclerosis activities, independent of blood pressure control7. Both clinical8 and experimental9studies have indicated that drugs commonly used to control blood pressure, such as nifedipine (Nif), protect the blood vessel wall, inhibit the progress of arteriosclerosis via exerting anti-oxidation and anti-inflammation functions. Statins, another class of drugs used in blood lipid regulation, enhance the expression of eNOS10 and reduce reactive oxygen species (ROS) damage11. Elderly people with hypertension invariably present with arteriosclerosis. There have been no studies on whether a drug combination therapy can better protect endothelial cells against damage than individual drugs or on the specific mechanisms of such a combination therapy. Here, we used human umbilical vein endothelial cells (HUVEC) to explore the effect and the mechanism of action of combined simvastatin (Sim) and Nif treatment in endothelial cells.
Materials and methods
Reagents and drugs
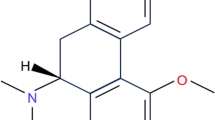
Nifedipine and simvastatin were purchased from Sigma (St Louis, MO, USA). Prior to use, 4.2 mg Sim was dissolved in 0.1 mL of 95% ethanol and then added to 0.15 mL of 0.1 mol/L NaOH, followed by incubation in a water bath for 2 h at 50 °C (this opened the closed lactone ring to activate it). Sim was brought to pH 7.2 with HCl and added to 1 mL deionized water, yielding a Sim concentration of 1 mol/L. It was kept at −20 °C until use12, 13. The phosphatidylinositol 3-kinase (PI3K) inhibitors wortmannin and LY294002 were purchased from Sigma. The calcium probe Fluo-3/AM, intensifier Pluronic F-127, intracellular ROS probe CM-H2DCFDA, fetal calf serum (FCS) and Dulbecco's modified Eagle's medium (DMEM) were purchased from Invitrogen (Eugene, OR, USA). H2O2 (AR Grade) was from Taopu Chemical Plant (Shanghai). Dilutions were made prior to use and were used within 5 min. The dilutions were kept out of direct light. The reagent box for the Griess assay was purchased from Beijing Kanghuiyu Technology Co, Ltd. Rabbit polyclonal anti-human eNOS, phosphorylated eNOS (Ser1177), Akt, p-Akt and β-actin antibodies and goat anti-rabbit IgG antibody were purchased from Santa Cruz Biotechnology Inc (Santa Cruz, CA, USA). Hanks' Buffered Saline solution (HBSS) (Sigma, St Louis, MO, USA) was used for normal cell buffer liquid.
Cell culture for HUVEC
HUVEC from ATCC (Manassas, VA, USA) were grown in DMEM with 10% FCS in 25-cm2 culture flasks at 37 °C and 5% CO2. Media were changed every 2−3 days.
Experimental groups
HUVEC were divided into seven groups:
Control
100 μmol/L H2O2 (100 μmol/L H2O2 cell incubation for 30 min)
100 μmol/L H2O2+0.1 μmol/L Nif (100 μmol/L H2O2+0.1 μmol/L Nif, cell incubation for 30 min)
100 μmol/L H2O2+1.0 μmol/L Nif (100 μmol/L H2O2+1.0 μmol/L Nif, cell incubation for 30 min)
100 μmol/L H2O2+10 μmol/L Nif (100μmol/L H2O2+10 μmol/L Nif, cell incubation for 30 min)
100 μmol/L H2O2+1.0 μmol/L Sim (1.0 μmol/L Sim, cell incubation for 2 h; 100 μmol/L H2O2, cell incubation for 30 min)
100 μmol/L H2O2+1.0 μmol/L Nif+1.0 μmol/L Sim (1.0 μmol/L Sim, cell incubation for 2 h; 100 μmol/L H2O2 and 1.0 μmol/L Nif, cell incubation for 30 min)
mRNA analysis by reverse transcriptase polymerase chain reaction (RT-PCR)
eNOS mRNA expression was detected by RT-PCR. HUVEC were split into 6-well plates, serum-starved for 12 h and stimulated as detailed above. After rinsing with HBSS, total RNA was extracted with Trizol according to the manufacturer's instructions (Invitrogen). cDNAs were made from 1.0 μg of total RNAs with the RT-PCR Reagent kit (Promega, Madison, WI, USA) following the manufacturer's instructions. Semiquantitative PCR was carried out with the PTC200 PCR thermocycler (MJ Research, Waltham,MA, USA). The genes encoding human eNOS and GAPDH (normalization control) were examined. The eNOS primer sequences were based on the human eNOS full-length cDNA sequence provided by GenBank and were designed with Prime5.0 software. The forward primer was 5′-AAG ATC TCC GCC TCG CTC A-3′; the reverse primer was 5′-GCT GTT GAA GCG GAT CTT A-3′. The eNOS amplicon length was 336 bp. The PCR mix contained cDNA 1.0 μL, 25 mmol/L MgCl2 5.0 μL, dNTP 1 μL, forward primer 0.25 μL, reverse primer 0.25 μL, 10×PCR reaction buffer 2.5 μL, and Taq DNA polymerase 0.5 μL. Deionized water was added to a final volume of 25 μL. The PCR program was 94 °C for 5 min, 35 cycles of 94 °C for 45 s, 56 °C for 45 s and 72 °C for 45 s, followed by extension at 72 °C for 7 min. The forward GAPDH primer was 5′-GAA TTT GGC TAC AGC AAC AGG GT G-3′; the reverse primer was 5′-TCT CTT CCT CTT GTG CTC TTG CTG-3′. The amplicon length was 204 bp. The PCR mix contained cDNA 1.0 μL, 25 mmol/L MgCl2 2.0 μL, dNTP 1.0 μL, forward primer 0.5 μL, reverse primer 0.5 μL, 10×PCR buffer 2.5 μL, Taq polymerase 0.25 μL, and deionized water to a final volume of 25 μL. The PCR program was 94 °C for 5 min, 35 cycles of 94 °C for 45 s, 58 °C for 45 s and 72 °C for 45 s, followed by extension at 72 °C for 7 min.
The expanded products were photographed after electrophoresis in 1.5% agarose. The grayscale of all bands was analyzed under a gel imaging system (ALPHA IMAGER2200).
Western blot analysis
HUVEC were grown to reach about 80% confluence, followed by serum-starving synchronization for 12 h and then applying the treatments. Each well was rinsed two times in HBSS, and total protein was extracted with 200 μL RIPA lysis solution (0.5 mmol/L Tris pH 7.4, 1.5 mmol/L NaCl, 10% Np-40, 10 mmol/L EDTA, 100 μg/mL PMSF), 2 μg/mL aprotinin, and 2 μg/mL leupeptin. A BCA protein reagent kit (Pierce, US) was used to measure protein concentration. Electrophoresis was carried out by loading 100 μg total protein in 10% polyacrylamide gels. Proteins were transferred to cellulose acetate membranes, blocked with 10% non-fat milk, and detected with 1:200 eNOS, 1:200 Akt, 1:200 p-Akt and 1:200 β-actin antibodies overnight at 4 °C. Anti-IgG secondary antibody (1:2000) conjugated to horseradish peroxidase was then added at room temperature for 1 h. After washing in TBST, the membrane was labeled with ECL reagents, and grayscale analysis was conducted using an image analysis system (Alphaimager 2200; Alpha Innotech Corp, San Leandro, CA, USA). The level of protein expression was analyzed by normalizing to β-actin.
Fluorescence measurement of intracellular calcium changes
The cultured HUVEC were cultured in 35-mm culture chambers designed for confocal microscopy (MatTek Corp, US). The cultured endothelial cells were synchronized with non-serum media for 12 h. After cells reached the dish walls, they were rinsed two times with 37°C HBSS and incubated for 15 min at 37 °C in 7.5 μmol/L Fluo-3 and 0.02% Pluronic F-127 diluted in HBSS containing Ca2+ and Mg2+. Cells were rinsed with HBSS three times, placed in a dark room for 10 min, and observed under the 60×oil-immersion objective of a Radiance 2000 laser scanning confocal microscope (LSCM) (Zeiss). The 49-mW argon ion laser was used, with an excitation wavelength of 488 nm. The fluorescent image of each layer of Fluo-3-stained cells was observed and collected. The scanning employed a time-course procedure with an interval of 5 min for collection of dynamic scanning data for seven cycles (ie, continuous detection for 30 min). The dynamic fluorescent image observed by high-speed computer was drawn in curved lines of fluorescence intensity changes of Ca2+. Lasersharp 2000 software (version 6.0) attached to the LSCM was used to analyze the data. At least 40 cells were selected for each experiment. The Ca2+ concentration in each cell was represented by mean fluorescence intensity (in arbitrary units).
Fluorescence measurement of intracellular reactive oxygen species (ROS)
The membrane-permeable CM-H2DCFDA entered endothelial cells and produced a fluorescent signal after intracellular oxidation by ROS, such as hydrogen peroxide and hydroxyl radical. Intracellular oxidant stress was monitored by measuring changes in fluorescence resulting from intracellular probe oxidation14, 15. The cultured HUVEC were plated in the 35-mm confocal microscopy culture dishes and synchronized with non-serum media for 12 h. After cells reached the dish walls, they were rinsed two times with 37 °C HBSS. CM-H2DCFDA diluted in HBSS to a final concentration of 5.0 μmol/L was added to the cells, which were incubated at 37 °C for 30 min. After three HBSS washes, cells were placed in a dark room for 10 min and observed by LSCM. Using the 49-mW argon ion laser, the excitation wavelength was 488 nm, and the emission wavelength was 505–530 nm. The intracellular ROS changes were observed in a dynamic state under the 60× oil-immersion lens (in a dark room). The scanning employed a time-course procedure with a 5-min interval for collection of dynamic scanning data and nine data collection points (ie, continuous detection for 40 min). The dynamic fluorescence image was analyzed as above. At least 35 cells were selected for each experimental group.
Measurement of NO levels
NO secreted from cells is rapidly oxidized to nitrite in culture medium; therefore, determination of nitrite concentrations was used as a measurement of NO production. A colorimetric Griess assay (Jiancheng Ins, Nanjing, China) was used. Briefly, HUVEC were cultured at 1×106/mL in a 24-well plate, 1 mL/well, at 37 °C and 5% CO2. The cells had grown to the wall after 24 h. The clear supernatant medium was removed and replaced with 1 mL fresh culture medium. The cells were divided according to the aforementioned experimental groups and collected 4 h after drug treatment. Following the manufacturer's instructions, the clear supernatant medium was collected to detect the NO level by the Griess method.
Statistical analysis
All data are presented as mean±SEM. Statistical significance was assessed using the Student's paired t-test and variance. All data analyses were performed using the software SPSS 10.0. P<0.05 was considered statistically significant.
Results
Simvastatin combined with nifedipine enhances the eNOS mRNA expression in endothelial cells
Stimulation with 100 μmol/L H2O2 for 30 min decreased eNOS mRNA expression remarkably compared with the control group. The eNOS mRNA expression was enhanced significantly after Nif was added (P<0.05 vs H2O2 group), and this effect was dose-dependent (P<0.05 vs 100 μmol/L H2O2+0.1 μmol/L Nif group, Figure 1).
The concentration-dependent effect of nifedipine on eNOS mRNA expression in endothelial cells after hydrogen peroxide-induced injury. Optical densities were obtained after normalization to GAPDH. Data are presented as mean±SEM from three independent experiments. bP<0.05 vs H2O2 group. eP<0.05 vs 100 μmol/L H2O2+0.1 μmol/L nifedipine group.
The eNOS mRNA expression increased significantly after 1.0 μmol/L Nif+1.0 μmol/L Sim stimulation compared with adding 1.0 μmol/L Nif or 1.0 μmol/L Sim alone, reaching 1.8-fold higher than that from Nif alone (P<0.05 vs H2O2 group, vs 100 μmol/L H2O2+1.0 μmol/L Sim group and vs 100 μmol/L H2O2 1.0 μmol/L Nif group). These results indicate that Nif protected endothelial cells from H2O2 damage and enhanced the expression of eNOS mRNA. This effect was enhanced significantly when Sim was added, indicating increased protection of endothelial cells (Figure 2).
The concentration-dependent effect of simvastatin combined with nifedipine on eNOS mRNA expression in endothelial cells after hydrogen peroxide-induced injury. Optical densities were obtained after normalization to GAPDH. Data are presented as mean±SEM from three independent experiments. bP<0.05 vs H2O2 group. eP<0.05 vs 100 μmol/L H2O2+1.0 μmol/L simvastatin group or 100 μmol/L H2O2+1.0 μmol/L nifedipine group.
Simvastatin combined with nifedipine enhances the expression of eNOS protein in endothelial cells
The eNOS protein in HUVEC decreased significantly after 30 min of stimulation with 100 μmol/L H2O2, and the expression of eNOS protein was enhanced dose dependently by Nif (P<0.05 vs H2O2 group; P<0.05; 100 μmol/L H2O2+0.1 μmol/L Nif group vs 100 μmol/L H2O2+10 μmol/L Nif group, Figure 3). We also found that the increased expression of eNOS protein was enhanced significantly by the combination of Sim and Nif compared with Sim or Nif alone (P<0.05 vs H2O2 group; P<0.05 vs 100 μmol/L H2O2+1.0 μmol/L Sim group and vs 100 μmol/L H2O2+1.0 μmol/L Nif group) (Figure 4). These results indicate that the expression of eNOS protein increased more by joint application of Sim and Nif than by application of Sim or Nif alone, thereby enhancing the protective action of these drugs for endothelial cells.
The concentration-dependent effect of nifedipine on eNOS protein expressions in endothelial cells after hydrogen peroxide-induced injury. Optical densities were obtained after normalization to β-actin. Data are presented as mean±SEM from three independent experiments. bP<0.05 vs H2O2 group. eP<0.05 vs 100 μmol/L H2O2+0.1 μmol/L nifedipine group or 100 μmol/L H2O2+1.0 μmol/L nifedipine group.
Effect of simvastatin combined with nifedipine on endothelial eNOS protein expression in endothelial cells after hydrogen peroxide-induced injury. Optical densities were obtained after normalization to β-actin. Data are presented as mean±SEM from three independent experiments. bP<0.05 vs H2O2 group. eP<0.05 vs 100 μmol/L H2O2+1.0 μmol/L simvastatin group or 100 μmol/L H2O2+1.0 μmol/L nifedipine group.
Simvastatin combined with nifedipine enhances NO secretion more than individual treatments in endothelial cells
The above results showed that Nif and Sim enhanced the expression of eNOS protein and mRNA. However, the increased eNOS does not automatically imply a protective effect of these two drugs for the cells. Therefore, further investigation was carried out by using the Griess assay to examine NO secretion in the cells upon different drug treatments. Table 1 shows that NO generation decreased markedly in the cells treated with 100 μmol/L H2O2 compared with no treatment (69.43±6.80 μmol/L vs 40.22±6.70 μmol/L, P<0.01, n=6). NO secretion increased to 60.80±6.67 μmol/L or 52.74±5.40 μmol/L, respectively, after adding 1.0 μmol/L Nif or 1.0 μmol/L Sim (P<0.01, n=6). Upon combined drug treatment, the secretion of NO increased to 82.68±6.51 μmol/L (P<0.01 vs 1.0 μmol/L Nif and vs 1.0 μmol/L Sim separately, n=6). These results indicate that joint drug treatment increased NO secretion in endothelial cells compared with Sim or Nif treatment separately, thereby providing better protection for endothelial cells against oxidative damage.
Stronger inhibitory effect on ROS generation from joint Sim and Nif treatment compared with separate treatments
The above results show that the expression of eNOS mRNA and protein was reduced by 100 μmol/L H2O2 in endothelial cells and that Nif and Sim inhibited this damaging effect. It has been reported7, 8 that calcium channel blockers and statins affect eNOS expression via many pathways, such as ROS signaling, calcium signaling and the bradykinin pathway.
To investigate the mechanism of protection provided by Sim and Nif, intracellular ROS were marked with the specific fluorescent probe CM-H2DCFDA in HUVEC, and we carried out dynamic real-time detection by LSCM. The fluorescence intensity of CM-CDFDA increased remarkably from stimulation with 100 μmol/L H2O2, reaching a peak after 30 min, which meant that H2O2 stimulation was able to increase ROS in cells. Moreover, ROS generation was inhibited by Nif in a dose-dependent manner (P<0.05 vs B group, n=35–45 cells) (Figure 5). However, adding 1.0 μmol/L Sim along with 1.0 μmol/L Nif significantly reduced the fluorescence intensity in HUVEC compared with the 1.0 μmol/L Nif and 1.0 μmol/L Sim groups (Figure 6, between A, C, E, and G groups, without statistical difference, P>0.05; P<0.05 vs B group; P<0.05 vs D, F group; n=40–45 cells), indicating that Nif+Sim enhanced the inhibition of ROS generation in HUVEC.
The concentration-dependent effect of nifedipine on ROS in endothelial cells after hydrogen peroxide-induced injury. Cells were pretreated with or without nifedipine (0.1, 1.0, and 10.0 μmol/L) and 100 μmol/L H2O2 for 30 min. Production of cellular ROS was determined by measuring the fluorescence intensity of the CM-H2DCFDA probe at 0 min and 30 min. Cell brightness was measured using LaserPix Image software. Results are presented as mean±SEM for 35−45 cells. Arbitrary units (au) represent fluorescent intensity corresponding to ROS changes. Groups at 0 min: no significant difference. bP<0.05 vs 100 μmol/L H2O2 group at 30 min.
Effect of nifedipine combined with simvastatin on ROS in endothelial cells after hydrogen peroxide-induced injury. Cells were pretreated with 1.0 μmol/L nifedipine for 30 min or 1.0 μmol/L simvastatin for 2 h and 100 μmol/L H2O2 for 30 min. Production of cellular ROS was determined by measuring the fluorescence intensity of the CM-H2DCFDA probe at 0 min and 30 min. Cell brightness was measured using LaserPix Image software. Results are presented as mean±SEM for 40−45 cells. Arbitrary units (au) represent fluorescent intensity corresponding to ROS changes. Groups at 0 min: no significant difference. bP<0.05 vs 100 μmol/L H2O2 group at 30 min. eP<0.05 vs 100 μmol/L H2O2+1.0 μmol/L Nif group or 100 μmol/L H2O2+1.0 μmol/L Sim group at 30 min.
Impact of simvastatin and nifedipine on Ca2+ concentration changes in endothelial cells
Calcium ion is the most physiologically important second messenger in endothelial cells, and it serves as the primary medium for communicating information in the cells. Nifedipine is a calcium antagonist, but whether its protective effect on endothelial cells results from inhibiting Ca2+ increases remains unclear. We first stimulated HUVEC with 100 μmol/L H2O2, which induced increased intracellular Ca2+ concentration ([Ca2+]i) in endothelial cells (P>0.05, n=40–45 cells, Figure 7). This effect on [Ca2+]i was significant after 10 min of stimulation and persisted up to 30 min. Different concentrations of Nif (0.1, 1.0, and 10 μmol/L) followed by the addition of 100 μmol/L H2O2 also resulted in increased [Ca2+]i. There was no significant difference in [Ca2+]i before and after Nif stimulation. Thus, H2O2-induced increases in [Ca2+]i cannot be inhibited by Nif. This indicates that the protective effect of Nif on endothelial cells had no relation to the calcium signal. Further comparisons between combined 1.0 μmol/L Nif+1.0 μmol/L Sim and the individual treatments of 1.0 μmol/L Nif and 1.0 μmol/L Sim also showed no significant difference in [Ca2+]i stimulated by 100 μmol/L H2O2. Therefore, the enhanced protective effect on endothelial cells by Sim did not occur via changes in intracellular calcium.
Effect of nifedipine combined with simvastatin on intracellular Ca2+ in endothelial cells after hydrogen peroxide-induced injury. The change in intracellular Ca2+ was determined by measuring the fluorescence intensity of the Fluo-3 probe. Cell brightness was analyzed by LaserPix Image software without enhancement. All experiments were performed with at least 40–45 cells. Arbitrary units (au) represent fluorescent intensity corresponding to intracellular Ca2+ changes. No significant difference. P>0.05.
Combination treatment of nifedipine and simvastatin enhances Akt phosphorylation and the ratio of p-eNOS/eNOS in endothelial cells
We wanted to investigate the mechanism by which increased eNOS regulates specific cellular functions. A previous report showed that ROS regulates the expression and activity of eNOS via the PI3K–Akt signaling pathway16. Akt activation led to activation of eNOS, increased eNOS phosphorylation (p-eNOS), and greater NO release. Here, we observed that, compared with the individual drug groups, combined Sim and Nif treatment up-regulated the level of Akt phosphorylation (without affecting total Akt) (P<0.05 vs groups 2 and 3), enhanced p-eNOS (P<0.05 vs groups 2 and 3) and total eNOS levels (P<0.05 vs groups 2 and 3), and increased the proportion of p-eNOS/eNOS (P<0.05 vs groups 2 and 3). These effects were inhibited by the PI3K inhibitors wortmannin and LY294002 (P<0.05 vs groups 1, 5, and 6). Taken together, these results indicate that combination treatment of Nif and Sim enhances the activity of eNOS via regulation of Akt activity (phosphorylation), which is the basis for the protective role of Nif+Sim in endothelial cells (Figure 8).
Effect of simvastatin combined with nifedipine on p-eNOS/eNOS and p-AKT/AKT expression in endothelial cells after hydrogen peroxide-induced injury. Optical densities of eNOS, p-eNOS, p-AKT, and AKT were obtained after normalization to β-actin. Data are presented as mean±SEM from three independent experiments. bP<0.05 vs H2O2 alone group, H2O2+Nif+Sim+Wortmannin group, and H2O2+Nif+Sim+LY294002 group. eP<0.05 vs H2O2+Nif or H2O2+Sim group.
Discussion
Endothelial cells are involved in many aspects of the generation and development of many cardiovascular maladies, such as hypertension and arteriosclerosis. Nitric oxide plays a role in stretching blood vessels, inhibiting the conglomeration of blood platelets and preventing conglutination between endothelial cells and between blood cells and endothelial cells. Nitric oxide plays a protective role in preventing the formation of hypertension and arteriosclerosis. Moreover, the expression of eNOS is the key factor for NO generation in endothelial cells. The synthesis and release of NO are markedly reduced in vascular endothelial cells of hypertension patients. Therefore, regulating eNOS expression and enhancing NO secretion will be important methods of reducing hypertension and preventing and controling arteriosclerosis17, 18, 19.
A typical model of endothelial cell damage is H2O2-induced damage. The use of this model helps in the study of the pathogenesis of cardiovascular diseases and in screens for drugs that protect blood vessels. The present investigations of eNOS mRNA and protein levels demonstrated that Nif enhances the expression of eNOS in endothelial cells and participates in the protection of endothelial cells. The expression of eNOS was also up-regulated by treatment with Sim alone. Moreover, we showed that the protective effect on endothelial cells was enhanced by combination treatment of Sim and Nif compared with either drug treatment separately. As shown here and previously20, 21, 1.0 μmol/L Nif and 1.0 μmol/L Sim are not cytotoxic to endothelial cells; on the contrary, they have a protective effect on endothelium.
For the regulatory mechanism of eNOS expression, it has been reported that an increased ROS level in endothelial cells inhibits the expression of eNOS22, 23, which is one of the reasons for hypertension in elderly people. The results of our study show that stimulation of endothelial cells with H2O2 can enhance the ROS level in endothelial cells. Nifedipine inhibited this ROS generation in a dose-dependent manner. The fluorescence intensity was further reduced in the cells with the combination treatment of Sim and Nif, which was concomitant with increased eNOS expression and NO level. This indicates that Sim combined with Nif enhances eNOS expression and NO secretion by inhibiting intracellular ROS generation.
Although Nif serves as an inhibitor of cell membrane L-type calcium channel, it is still disputed whether it protects endothelial cells via inhibiting extracellular calcium ion influx. It has been reported that increased intracellular Ca2+ may inhibit the expression of eNOS. Therefore, we asked whether the combination treatment of Nif and Sim could also enhance eNOS expression by inhibiting intracellular Ca2+ changes. We found no visible Ca2+ changes in HUVEC after stimulation with H2O2 with or without Nif and/or Sim. This indicates that enhanced eNOS expression by Nif and Sim was not a result of the inhibition of calcium influx, in agreement with the results of Aono et al24. A recent study indicated that L-type Ca2+ channels did not exist in the endothelial cell membrane25. It was reported in other studies26 that Nif combines with cell membrane lipids directly to inhibit ROS production, due to the specificity of its molecular structure. Moreover, endothelial cells stimulated with H2O2 may induce a series of biological effects via the release of endoplasmic reticulum Ca2+ to increase Ca2+ concentration in the cytoplasm27. Here, Nif was unable to block the increase of influx of extracellular Ca2+ into the cells. Therefore, this result is not in contradiction with Nif serving as an antagonist of the calcium signaling pathway. Nif protects endothelial cells by directly inhibiting ROS generation.
PI3K/Akt signaling regulates the activity of eNOS and enhances NO release from endothelial cells28. The excessive production of ROS damages the cells, but lower concentrations of ROS are able to activate the PI3K/Akt/eNOS pathway and enhance the activity of eNOS (raise the level of eNOS phosphorylation), thereby protecting the endothelial cells. The results of this study also support this conclusion, as the combination treatment of Nif and Sim reduced ROS levels, up-regulated Akt phosphorylation relative to total Akt, enhanced the levels of both phosphorylated and total eNOS, and raised the proportion of p-eNOS/eNOS. This effect was more significant from the combination treatment than from each drug separately. Our results are consistent with a mechanism in which Nif combines with cell membrane lipids directly to resist ROS over-production. Yamagishi et al29, 30. demonstrated that Nif directly abrogates vascular reduced nicotinamide-adenine dinucleotide phosphate (NADPH) oxidase activity in endothelial cells. Furthermore, Sim inhibits ROS (O2−, OH−) production, possibly by decreasing NADPH oxidase and increasing peroxiredoxin 3/thioredoxin 2 antioxidant activities31.
In summary, we discovered that combination treatment of Sim and Nif enhanced the expression of eNOS mRNA and protein, up-regulated the ratio of p-eNOS/eNOS, increased NO secretion and enhanced the protective effect of the two drugs individually on endothelial cells. The combination treatment works by reducing the generation of ROS in the cells and up-regulating Akt activation, rather than via inhibition of calcium signaling. These results provide the basis for their use in clinical practice, and they indicate that Sim combined with Nif will be useful in reducing hypertension and preventing/treating arteriosclerosis.
Author contribution
Zhuo YANG and Ming FAN designed the research; Xiao-niao CHEN performed the experiments; Zhe FENG and Jing-yao HAN contributed new reagents or analytic tools; Jun XU analyzed data; Xiao-niao CHEN and Zhuo YANG wrote the paper.
References
Jiang JY, Wong MC, Zhang XH, Fung H, Griffiths S, Mercer S . Profiles of mortality among Chinese hypertensive patients in Hong Kong: a cohort study. J Hum Hypertens 2009; 23: 735–42.
Matthys KE, Bult H . Nitric oxide function in atherosclerosis. Mediators Inflamm 1997; 6: 3–21.
Ross R . The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 1993; 362: 801–9.
Noll G, Tschudi M, Nava E, Luscher TF . Endothelium and high blood pressure. Int J Microcirc Clin Exp 1997; 17: 273–9.
Moncada S, Palmer RM, Higgs EA . Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol Rev 1991; 43: 109–42.
Rabelink TJ, Luscher TF . Endothelial nitric oxide synthase: host defense enzyme of the endothelium? Arterioscler Thromb Vasc Biol 2006; 26: 267–71.
Zanchetti A . The antiatherogenic effects of antihypertensive drugs: experimental and clinical evidence. Clin Exp Hypertens A 1992; 14: 307–31.
Lichtlen PR, Hugenholtz PG, Rafflenbeul W, Hecker H, Jost S, Deckers JW . Retardation of angiographic progression of coronary artery disease by nifedipine. Results of the International Nifedipine Trial on Antiatherosclerotic Therapy (INTACT). INTACT Group Investigators. Lancet 1990; 335: 1109–13.
Matsubara M, Hasegawa K . Benidipine, a dihydropyridine-calcium channel blocker, prevents lysophosphatidylcholine-induced injury and reactive oxygen species production in human aortic endothelial cells. Atherosclerosis 2005; 178: 57–66.
Deng HF, Xiong Y . Effect of pravastatin on impaired endothelium-dependent relaxation induced by lysophosphatidylcholine in rat aorta. Acta Pharmacol Sin 2005; 26: 92–8.
Ma FX, Liu LY, Xiong XM . Protective effects of lovastatin on vascular endothelium injured by low density lipoprotein. Acta Pharmacol Sin 2003; 24: 1027–32.
Gerson RJ, MacDonald JS, Alberts AW, Kornbrust DJ, Majka JA, Stubbs RJ, et al. Animal safety and toxicology of simvastatin and related hydroxy-methylglutaryl-coenzyme A reductase inhibitors. Am J Med 1989; 87: 28S–38S.
Todd PA, Goa KL . Simvastatin. A review of its pharmacological properties and therapeutic potential in hypercholesterolaemia. Drugs 1990; 40: 583–607.
Ye G, Metreveli NS, Ren J, Epstein PN . Metallothionein prevents diabetes-induced deficits in cardiomyocytes by inhibiting reactive oxygen species production. Diabetes 2003; 52: 777–83.
Brunt KR, Fenrich KK, Kiani G, Tse MY, Pang SC, Ward CA, et al. Protection of human vascular smooth muscle cells from H2O2-induced apoptosis through functional codependence between HO-1 and AKT. Arterioscler Thromb Vasc Biol 2006; 26: 2027–34.
Koneru S, Penumathsa SV, Thirunavukkarasu M, Samuel SM, Zhan L, Han Z, et al. Redox regulation of ischemic preconditioning is mediated by the differential activation of caveolins and their association with eNOS and GLUT-4. Am J Physiol Heart Circ Physiol 2007; 292: H2060–72.
Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G . Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci USA 1987; 84: 9265–9.
Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, et al. Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature 1995; 377: 239–42.
Hyndman ME, Parsons HG, Verma S, Bridge PJ, Edworthy S, Jones C, et al. The T-786→C mutation in endothelial nitric oxide synthase is associated with hypertension. Hypertension 2002; 39: 919–22.
Mak IT, Boehme P, Weglicki WB . Protective effects of calcium channel blockers against free radical-impaired endothelial cell proliferation. Biochem Pharmacol 1995; 50: 1531–4.
Henrich D, Seebach C, Wilhelm K, Marzi I . High dosage of simvastatin reduces TNF-alpha-induced apoptosis of endothelial progenitor cells but fails to prevent apoptosis induced by IL-1beta in vitro. J Surg Res 2007; 142: 13–9.
Ungvari Z, Csiszar A, Kaley G . Vascular inflammation in aging. Herz 2004; 29: 733–40.
Hansson GK . Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005; 352: 1685–95.
Aono Y, Ariyoshi H, Sakon M, Ueda A, Tsuji Y, Kawasaki T, et al. Human umbilical vein endothelial cells (HUVECs) show Ca2+ mobilization as well as Ca2+ influx upon hypoxia. J Cell Biochem 2000; 78: 458–64.
Himmel HM, Whorton AR, Strauss HC . Intracellular calcium, currents, and stimulus-response coupling in endothelial cells. Hypertension 1993; 21: 112–27.
Cominacini L, Fratta Pasini A, Garbin U, Pastorino AM, Davoli A, Nava C, et al. Antioxidant activity of different dihydropyridines. Biochem Biophys Res Commun 2003; 302: 679–84.
Mason RP, Trumbore MW . Differential membrane interactions of calcium channel blockers. Implications for antioxidant activity. Biochem Pharmacol 1996; 51: 653–60.
Lenasi H, Kohlstedt K, Fichtlscherer B, Mulsch A, Busse R, Fleming I . Amlodipine activates the endothelial nitric oxide synthase by altering phosphorylation on Ser1177 and Thr495. Cardiovasc Res 2003; 59: 844–53.
Yamagishi S, Nakamura K, Takenaka K, Matsui T, Inoue H . Pleiotropic effects of nifedipine on atherosclerosis. Curr Pharm Des 2006; 12: 1543–7.
Yamagishi S, Nakamura K, Matsui T . Role of oxidative stress in the development of vascular injury and its therapeutic intervention by nifedipine. Curr Med Chem 2008; 15: 172–7.
Thomas SR, Witting PK, Drummond GR . Redox control of endothelial function and dysfunction: molecular mechanisms and therapeutic opportunities. Antioxid Redox Signal 2008; 10: 1713–65.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Xn., Xu, J., Feng, Z. et al. Simvastatin combined with nifedipine enhances endothelial cell protection by inhibiting ROS generation and activating Akt phosphorylation. Acta Pharmacol Sin 31, 813–820 (2010). https://doi.org/10.1038/aps.2010.58
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2010.58
Keywords
This article is cited by
-
Fluvastatin attenuated the effect of expression of β1 integrin in PAN-treated podocytes by inhibiting reactive oxygen species
Molecular and Cellular Biochemistry (2015)
-
Current Therapeutic Strategies to Mitigate the eNOS Dysfunction in Ischaemic Stroke
Cellular and Molecular Neurobiology (2012)